Contents
- Pumping breastmilk
- How to pump breast milk
- How to keep your breast pump clean
- When to start pumping breast milk?
- How long to pump breast milk?
- How often to pump breast milk?
- How much breast milk will I get when I pump?
- Storing breast milk
- How to store breast milk
- Where should I store my breast milk?
- How long can I store my breast milk?
- Why does my milk smell or taste soapy?
- Why is my milk separating?
- How do I thaw and warm breast milk once I’m ready to use it?
- Is it safe to refreeze my milk after thawing?
- Can I reuse previously fed milk if my baby does not finish?
- Is it safe to store my milk in a shared refrigerator?
- I have thrush; is my breast milk safe?
- How long should a mother breastfeed?
- Will there be times that my baby needs more milk than I have ready?
- Can what I eat and drink affect my breast milk?
- Do I need to take vitamins or supplements when I’m breastfeeding?
- Can smoking while breastfeeding hurt my baby?
- Can I pass alcohol or street drugs to your baby through breast milk?
- Are prescription medicines safe to take when I’m breastfeeding?
- Is it safe to take prescription opioids when I’m breastfeeding?
- Are over-the-counter medicines safe to take when you’re breastfeeding?
- What medical conditions make breastfeeding unsafe for your baby?
- If I’ve been exposed to lead, is it safe to breastfeed?
- What are human milk banks?
- Is it safe for families to buy breast milk on the internet?
Pumping breastmilk
Pumping breast milk is when you take milk out of your breast with either a hand-held pump or an electric pump. You might want to express your breastmilk because your breasts feel swollen or engorged or because you want to have some breastmilk stored in the fridge or freezer for using at a later time.
Some women find it easy to express, and other women find it more difficult. It can sometimes take a while to learn how to express. Most mums find pumping breastmilk easier if they’re in a comfortable, private place. Get yourself relaxed and comfortable, and have a glass of water handy to drink. Give yourself plenty of time too – especially when you’re first learning to express.
Different women can express different amounts of breastmilk. It depends on many things, including your body, your baby’s last feed, your baby’s age and how often you express. If you can’t express much (or any) milk, check with your midwife, child and family health nurse or lactation consultant to make sure you’re expressing correctly.
There are three ways to express breastmilk:
- by hand
- with a hand-held pump
- with an electric pump.
When you are away from your baby, you can pump or hand express milk from your breasts ahead of time so that your baby can drink your breast milk from a bottle.
How to pump breast milk
Using the breast pump helpful suggestions:
- Assemble the clean electric breast pump kit using the maker’s instructions. There will be written instructions with the kit and you would have been shown how to put it together by the your breastfeeding consultant from whom you hired the pump. If you have any questions please ring her so you know you have it connected properly.
- Set the pump to the lowest suction setting. Try to start your let-down by using some of the ideas listed above. When putting on the breast cup, make sure the nipple is in the center and that the cup has good skin contact all around to stop air entering. If your nipple hurts when you start expressing with the pump, stop and check to make sure the nipple is centered in the breast cup and the suction is low.
- At first, you may find it helps to keep the session short, gradually lengthening sessions. Some mothers find it useful to change breasts several times during the session. If you use a double pump kit, the session will be shorter than expressing with a single kit. Once you are comfortable with using the pump, you can increase the suction setting. Make sure it is still comfortable for you. Keep the kit upright while you are expressing to prevent milk from going into the tubing. If milk does go into the tubing, stop the pump and rinse the tubing with water. It is best not to use the pump when the tubing is wet, particularly in pumps where the tubing connects to the inside of the pump. It can draw moisture into the pump and cause damage. In pumps with a closed kit, slight dampness or moisture in the tubing should not be a problem. However, after expressing with wet tubing, take the kit apart to allow all parts to dry.
- In the first few days or so after the birth, you will make only small amounts of the first milk, called colostrum. It is usually best to express this by hand. You will find that you will have a lot more milk a few days later, once the milk comes in. An electric breast pump is then very useful. The milk supply settles down within a few weeks to be the right amount to meet the baby’s needs. The mother of a premature baby makes slightly different milk to the mother of a term baby, because her milk is more suited to her baby’s level of maturity. Be guided by your medical advisers for your baby’s feeding needs. You will be able to express more milk as you get used to expressing.
- While you still have colostrum in your breasts, the milk will have a yellow color and may look rather creamy. It will form layers on standing. The color of colostrum from different mothers can vary a lot, so don’t be surprised if yours looks quite different to another mother’s. This is quite normal. As your milk supply increases, the color of the milk becomes more bluish-white.
- It still forms layers on standing, with the creamy layer at the top. Milk may look different at different times of the day and this also depends on how long it has been since you have expressed or fed your baby. Your milk is right for your baby.
- Some mothers find that after expressing for many weeks their milk supply decreases. This is because a baby is better at getting the milk from the breast than a pump. When you are able to feed your baby at the breast, you will find that with frequent feeds, your supply will soon increase. If you are unable to feed your baby at the breast, expressing more often will help to increase your milk supply. After a week or so, you may be able to return to your previous expressing schedule. It can be helpful to finish off each session with a few minutes of hand expressing. This will help to empty your breasts and help increase your milk supply. If your supply is decreasing despite your attempts to increase it, you may wish to contact your breastfeeding consultant to discuss other ideas.
- Contact the breastfeeding counselor from whom you hired the pump if any of the following happen:
- the breast pump is not working (please check the instructions first)
- your milk supply seems to be dropping
- you feel the pump is not helping you
- you need someone to talk to about breastfeeding or breastmilk.
Please contact your breastfeeding consultant at least once a week to let her know how you are getting on.
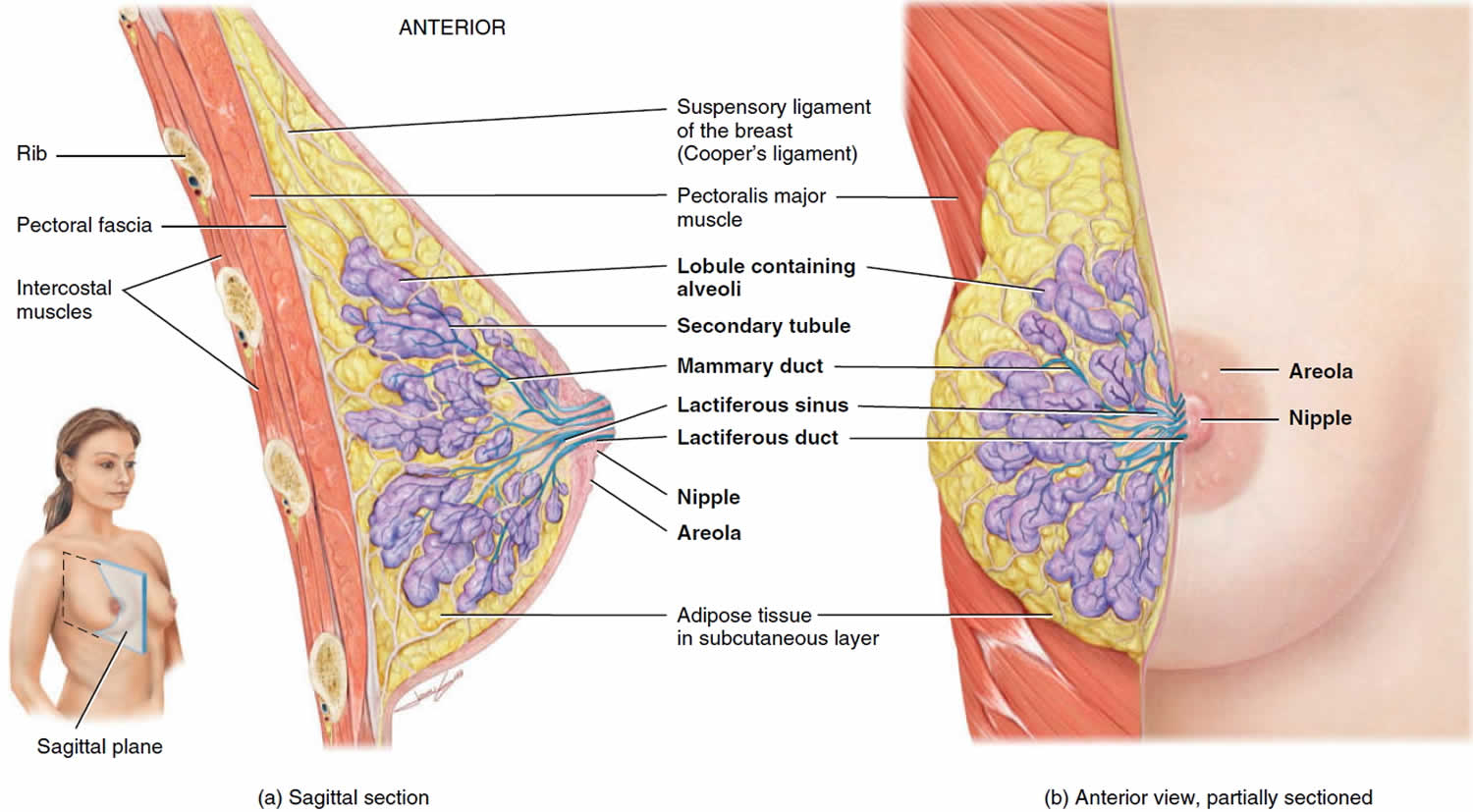
Figure 1. Normal breast (female)
How do breast pumps work?
All pumps have a shield that covers your breast and a container that collects breast milk. If you’re not sure what kind of pump is best for you, ask your lactation consultant. This is a person who has special training to help women breastfeed. Check with your health insurance company to see if it helps pay for a pump.
You may not know how often you’ll need to pump until you have your baby. So you may want to wait until after your baby is born to get one.
There are two kinds of breast pumps:
- Manual breast pump. This is a pump that you work by hand. You can use a manual pump anywhere because it doesn’t need electricity. This kind of pump is good if you don’t need to pump very often or if you don’t need a lot of milk at one time.
- Powered breast pump. This pump uses batteries or electricity. It has a motor to pump your breasts. You can use a single pump that works on one breast at a time. Or you can use a double pump that works on both breasts at the same time. If you’re going back to school or work, you may like double pumps because they’re faster than single pumps.
Do all breastfeeding moms use a breast pump?
No. But if there are times you’ll be away from your baby, like if you’re going back to work or school, you may need a breast pump. A breast pump helps you remove breast milk from your breasts. You can use the milk at a later time to feed your baby. Breast milk that you pump from your breasts is called expressed milk.
Breast pumps can help you in lots of ways:
- If you go back to work or school, you still can feed your baby breast milk.
- Your partner or another caregiver can feed your baby breast milk.
- Pumping helps keep your breast milk from building up in your breasts. This helps prevent discomfort and infection.
Expressing breastmilk with a hand-held pump
Hand-held breast pumps usually consist of a suction cup attached to a pump handle and collection bottle or container.
Just as with hand-expressing, the first step in expressing breastmilk with a hand-held pump is getting yourself relaxed and comfortable. This helps get your let-down happening in whatever way works for you. Gentle massage as described above is a good idea too.
Here are the next steps, when you’re ready:
- Place the suction cup of the pump directly over your breast with your nipple centered.
- Squeeze the pump handle gently and rhythmically – you might see only drops of milk until your let-down happens, and then it’ll spray.
- Pump until your milk flow stops.
Expressing breastmilk with an electric pump
Electric breast pumps are much like hand-held pumps, except that you don’t have to do the pumping yourself. Attach the suction cup to your breast (or breasts, in the case of double pumps).
As with expressing breastmilk by hand or by hand-help pump, get comfortable and relaxed to start. This helps with your let-down.
Here are the next steps, when you’re ready:
- Place the suction cup of the pump directly over your breast with your nipple centred.
- Start with low suction and increase it to a level that’s comfortable for you.
- Pump until your milk flow stops.
You can often get more milk by hand-expressing after the flow with the pump has stopped.
You can buy or hire electric breast pumps. You’ll need to buy your own pump kit to attach to the electric pump.
Expressing breastmilk by hand
Here are the basic steps for expressing breastmilk by hand.
Getting ready to express breastmilk by hand:
- Wash your hands with soap and warm water.
- Gently massage your breast. Start from the top of your breast and stroke towards your nipple. Massage the underside of your breast too. Do this several times to ensure the whole breast is massaged. This helps improve your let-down reflex.
- Place a clean plastic dish or a wide bowl under your breast, either between your legs or on a low table, leaving both your hands free. You might need a clean towel to catch any spills or to wipe slippery, wet fingers.
Expressing by hand:
- You can support your breast with one hand if you have large and heavy breasts.
- Place your thumb and finger directly opposite each other, either side of and well back from your nipple.
- Gently press inward towards the centre of the breast, until you feel the bulk of the breast. Expressing shouldn’t hurt.
- Gently press finger and thumb towards each other using a rhythmic rolling movement. This will compress the ducts, and milk will flow out of your nipple. There might be only drops until your let-down reflex happens. After this, you should get sprays from the nipple with each squeeze.
- Once the milk flow slows, move your fingers to a different position around the nipple and press again. This expresses more milk and empties all sectors of the breast. Change hands if your fingers get tired.
- Repeat the process on the other breast. Expressing milk can be tiring, so stopping for a drink of water might help you relax before you start again.
- If you need more milk, change from breast to breast, or wait and try again later.
How to keep your breast pump clean
Germs can grow quickly in breast milk or breast milk residue that remains on pump parts. Following these steps can keep your breast pump clean and help protect your baby from these germs. If your baby was born prematurely or has other health concerns, your baby’s health care providers may have more recommendations for pumping breast milk safely.
Before each use:
- Wash hands. Wash your hands well with soap and water for 20 seconds.
- Assemble. Assemble clean pump kit. Inspect whether the pump kit or tubing has become moldy or soiled during storage. If your tubing is moldy, discard and replace immediately.
- Clean if using a shared pump.Clean pump dials, power switch, and countertop with disinfectant wipe.
After each use:
- Store milk safely. Cap milk collection bottle or seal milk collection bag, label with date and time, and immediately place in a refrigerator, freezer, or cooler bag with ice packs.
If milk collection container will be stored at a hospital or childcare facility, add name to the label. - Clean pumping area. Especially if using a shared pump, clean the dials, power switch, and countertop with disinfectant wipes.
- Take apart and inspect pump kit. Take apart breast pump tubing and separate all parts that come in contact with breast/breast milk for example, flanges, valves, membranes, connectors, and milk collection bottles.
- Rinse pump kit. Rinse breast pump parts that come into contact with breast/breast milk under running water to remove remaining milk
- Clean pump kit. As soon as possible after pumping, clean pump parts that come into contact with breast/breast milk in one of the following ways.
- Clean by hand.
- Use a wash basin. Place pump parts in a clean wash basin used only for washing infant feeding equipment. Do not place pump parts directly in the sink, because germs in sinks or drains could contaminate the pump.
- Add soap and water. Fill wash basin with hot water and add soap.
- Scrub. Scrub items according to pump kit manufacturer’s guidance. If using a brush, use a clean one that is used only to clean infant feeding items.
- Rinse. Rinse by holding items under running water, or by submerging in fresh water in a separate basin that is used only for cleaning infant feeding items.
- Dry. Allow to air-dry thoroughly. Place pump parts, wash basin, and bottle brush on a clean, unused dish towel or paper towel in an area protected from dirt and dust. Do not use a dish towel to rub or pat items dry because doing so may transfer germs to the items.
- Clean in a dishwasher (if recommended by pump kit manufacturer).
- Wash. Place disassembled pump parts in dishwasher. Be sure to place small items into a closed-top basket or mesh laundry bag so they don’t end up in the dishwasher filter. If possible, run the dishwasher using hot water and a heated drying cycle (or sanitizing setting); this can help kill more germs.
- Remove from dishwasher. Wash your hands with soap and water before removing and storing cleaned items. If items are not completely dry, place items on a clean, unused dish towel or paper towel to air-dry thoroughly before storing. Do not use a dish towel to rub or pat items dry because doing so may transfer germs to the items.
- Clean by hand.
- Clean wash basin and bottle brush. If you use a wash basin or bottle brush when cleaning your pump parts, rinse them well and allow them to air-dry after each use. Consider washing them every few days, either in a dishwasher with hot water and a heated drying cycle, if they are dishwasher-safe, or by hand with soap and warm water.
For extra germ removal, sanitize pump parts at least once daily. Sanitizing is especially important if your baby is less than 3 months old, was born prematurely, or has a weakened immune system due to illness or medical treatment (such as chemotherapy for cancer). Daily sanitizing of pump parts may not be necessary for older, healthy babies, if the parts are cleaned carefully after each use. Sanitize all items (even the bottle brush and wash basin!) by using one of the following options.
Note: If you use a dishwasher with hot water and a heating drying cycle (or sanitizing setting) to clean infant feeding items, a separate sanitizing step is not necessary.
- Clean first. Pump parts, bottle brushes, and wash basins should be sanitized only after they have been cleaned.
- Sanitize. Sanitize the pump kit, bottle brushes, and wash basins using one of the following options. Check manufacturer’s instructions about whether items may be steamed or boiled.
- Steam: Use a microwave or plug-in steam system according to the manufacturer’s directions.
- Boil:
- Place disassembled items that are safe to boil into a pot and cover with water.
- Put the pot over heat and bring to a boil.
- Boil for 5 minutes.
- Remove items with clean tongs.
- Allow to air-dry thoroughly. Place sanitized pump parts, wash basin, and bottle brush on a clean, unused dish towel or paper towel in an area protected from dirt and dust. Do not use a dish towel to rub or pat items dry because doing so may transfer germs to the items.
Allow the clean pump parts, bottle brushes, and wash basins to air-dry thoroughly before storing to help prevent germs and mold from growing. Once completely dry, the items should be stored in a clean, protected area to prevent contamination during storage.
- Wash hands. Wash hands well with soap and water.
- Reassemble. Put together the clean, dry pump parts.
- Store safely. Place reassembled pump kit in a clean, protected area such as inside an unused, sealable food storage bag. Store wash basins and bottle brushes in a clean area.
When to start pumping breast milk?
If you are planning to return to work or school or will be away from your baby for other reasons, you may want to start pumping 1 or 2 weeks in advance. This helps you learn how your pump works and will give you the chance to practice pumping and will give your baby time to get used to feeding from a bottle.
You can pump right after your baby eats or between feedings. Or you may prefer to pump from one breast while you feed your baby from the other.
Starting at home also helps you build a collection of breast milk. You can store it for your baby’s feedings when you return to work.
How long to pump breast milk?
It takes about the same time to pump breast milk as it does to breastfeed. With practice, you may be able to pump in as little as 10 to 15 minutes. While you are at work, try to pump as often as your baby usually feeds. This may be every 3 to 4 hours for 15 minutes each time. To keep up your milk supply, give your baby extra feedings when you are together. You also can pump right after your baby feeds to help your breasts make more milk.
How often to pump breast milk?
When away from your baby, try to pump at the same times or as often as your baby is breastfeeding. This will help remind your body to keep making the amount of milk your baby needs.
How much breast milk will I get when I pump?
You may not get much breast milk when you first start pumping. This will change as you continue to pump regularly. Pumping at the same times or as often as your baby normally breastfeeds should help your body make about the amount of milk your baby needs. Your breasts will begin to make more milk. This amount may differ from baby to baby and can change as babies grow. The more often you pump, the more milk your breasts make. Drink lots of water to stay hydrated. This will also help your milk supply.
If you find that you are not able to pump as much milk as your baby wants to eat while you are away, you may want to consider adding another pumping session to increase your milk supply.
Storing breast milk
By following recommended storage and preparation techniques, breastfeeding mothers and caretakers of breastfed infants and children can maintain the safety and quality of expressed breast milk for the health of your baby.
Table 1 are general guidelines for storing human milk at different temperatures. Various factors (milk volume, room temperature when milk is expressed, temperature fluctuations in the refrigerator and freezer, and cleanliness of the environment) can affect how long human milk can be stored safely.
The American Academy of Pediatrics recommends breastfeeding as the sole source of nutrition for your baby for about 6 months and can be continued for as long as both mother and baby desire it.
Stored breast milk can vary in color. It can be bluish, yellowish, or brownish. It is normal for breast milk to separate (the fatty part of the milk goes to the top). Shake the bottle or sealed bag and the fat should go back into the milk. If it does not, then the breast milk may be bad. You should smell the milk before feeding it to your baby. Bad milk smells sour. If you still aren’t sure, try tasting the milk. If it tastes sour, then it is bad and needs to be thrown away.
If you choose to freeze breast milk, you need to thaw it before giving it to your baby. Safe thawing of breast milk:
- Always thaw the oldest breast milk first. Remember first in, first out. Over time, the quality of breast milk can decrease.
- While many infants may be content drinking room temperature milk, some may have a preference for warmer milk. It is recommended to warm milk slowly in lukewarm water to protect fat content and nutrients.
- There are 2 ways you can thaw the milk:
- Put the container of milk in warm water. Swirl the container around in the water until the milk thaws.
- Put the container of milk in the refrigerator the day before it is to be used.
- Never thaw or heat breast milk in a microwave. Microwaving can destroy nutrients in breast milk and create hot spots, which can burn a baby’s mouth.
- Avoid boiling as this method will cause loss of nutritional properties of human milk and could unevenly hot making it dangerous for infants to drink.
- Use breast milk within 24 hours of thawing in the refrigerator (this means from the time it is no longer frozen or completely thawed, not from the time when you took it out of the freezer).
- Once breast milk is brought to room temperature or warmed after storing in the refrigerator or freezer, it should be used within 2 hours.
- Never refreeze breast milk once it has been thawed.
Thawed breast milk can be refrigerated for up to 24 hours, but it should not be refrozen. Do not use hot water to thaw breast milk. The milk could get too hot and burn your baby’s mouth. Do not thaw frozen breast milk in a microwave. This can damage valuable proteins in breast milk.
Table 1. Guidelines for storage of breastmilk at home for use with healthy, full-term babies
| Breast milk status | Room temperature (78.8 °F [26°C] or lower) | Refrigerator (39.2 °F [4°C] or lower) | Freezer |
|---|---|---|---|
| Freshly expressed into container | 6–8 hours If refrigerator is available store milk there |
3–5 days Store at back where it is coldest |
2 weeks in freezer compartment inside refrigerator 3 months in freezer section of refrigerator with separate door 6–12 months in deep freeze (-0.4 °F [-18°C] or lower) |
| Previously frozen thawed in refrigerator but not warmed | 4 hours or less – that is, the next feeding | 24 hours | NEVER refreeze human milk after it has been thawed |
| Thawed outside refrigerator in warm water | For completion of feeding | 4 hours or until next feeding | NEVER refreeze human milk after it has been thawed |
| Infant has begun feeding | Only for completion of feeding | Discard | Discard |
Breast milk storage containers
- Bottles
- glass or hard-sided plastic containers with well-fitting tops
- avoid containers made with the chemical bisphenol A (BPA), identified with a number 3 or 7 in the recycling symbol. A safe alternative is polypropylene, which is soft, semi-cloudy, and has the number 5 recycling symbol and/or the letters PP. You can avoid the risks of plastic completely by using glass.
- containers which have been washed in hot, soapy, water, rinsed well, and allowed to air-dry before use or washed and dried in a dishwasher
- containers should not be filled to the top – leave an inch of space to allow the milk to expand as it freezes
- Bags
- freezer milk bags that are designed for storing human milk
- squeeze out the air at the top before sealing, and allow about an inch for the milk to expand when frozen.
- stand/lay the bags in another container at the back of the refrigerator shelf or in the back of freezer where the temperature will remain the most consistently cold.
Disposable bottle liners or plastic bags are not recommended. With these, the risk of contamination is greater. Bags are less durable and tend to leak, and some types of plastic may destroy nutrients in milk.
Before expressing or handling breast milk:
- Wash your hands well with soap and water. If soap and water are not available, use an alcohol-based hand sanitizer that contains at least 60% alcohol.
- Mothers can express breast milk by hand or with a manual or electric pump.
- If using a pump, inspect the pump kit and tubing to make sure it is clean. Discard and replace moldy tubing immediately.
- If using a shared pump kit, clean pump dials, power switch, and countertop with disinfectant wipe.
Techniques you can use to encourage your let-down reflex when expressing your breast milk
There are several techniques you can use to encourage your let-down reflex when expressing. For example:
- Consciously try to relax, using whatever method suits you. Try to express in a quiet, warm, relaxing area, away from distractions. While expressing, breathe slowly and deeply. You could express in the place you usually sit to feed. Some mothers have a warm drink first or listen to soft music. Warmth (expressing after a warm shower, warm face washers on the breast for a few minutes before starting) may also help.
- Gently massaging your breasts by stroking down towards the nipple, and gently rolling the nipple between your fingers. While you can’t actually push the milk out of your breasts by massage, you can help trigger the let-down by touching your breasts.
- Thinking about your baby and how much your breastmilk is helping her will encourage your let-down reflex. If she is premature or sick in hospital,you might find it easier to express near her cot or just after you leave her. If you are away from her, looking at her photo can help.
- Having someone support you. Many mothers find they manage much better when they have an encouraging partner or friend.
Safe cleaning of infant feeding items and pumping equipment
- Carefully cleaning, sanitizing, and storing your pump equipment, baby’s bottles, and other feeding items will help to protect your breast milk from contamination. CDC has guidance on how to safely clean and store pump equipment and infant feeding items.
Storing breast milk after expressing:
- Use breast milk storage bags or clean food-grade containers with tight fitting lids made of glass or plastic to store expressed breast milk.
- Avoid bottles with the recycle symbol number 7, which indicates that the container may be made of a BPA-containing plastic.
- Never store breast milk in disposable bottle liners or plastic bags that are not intended for storing breast milk.
- Freshly expressed or pumped milk can be stored:
- At room temperature (77 °F [25 °C] or colder) for up to 4 hours.
- In the refrigerator for up to 4 days.
- In the freezer for about 6 months is best; up to 12 months is acceptable. Although freezing keeps food safe almost indefinitely, recommended storage times are important to follow for best quality.
Storage tips:
- Clearly label the breast milk with the date it was expressed.
- Do not store breast milk in the door of the refrigerator or freezer. This will help protect the breast milk from temperature changes from the door opening and closing.
- If you don’t think you will use freshly expressed breast milk within 4 days, freeze it right away. This will help to protect the quality of the breast milk.
- Freeze breast milk in small amounts of 2 to 4 ounces (or the amount that will be offered at one feeding) to avoid wasting breast milk that might not be finished.
- When freezing breast milk, leave about an inch of space at the top of the container because breast milk expands as it freezes.
- If you will be delivering breast milk to a childcare provider, clearly label the container with the child’s name and talk to your childcare provider about other requirements they might have for labeling and storing breast milk.
- Breast milk can be stored in an insulated cooler bag with frozen ice packs for up to 24 hours when you are traveling. Once you arrive at your destination, milk should be used right away, stored in the refrigerator, or frozen.
Feeding expressed breast milk
- Breast milk does not need to be warmed. It can be served room temperature or cold.
- If you decide to warm the breast milk, here are some tips:
- Keep the container sealed while warming.
- Warm breast milk by placing the container of breast milk into a separate container or pot of warm water for a few minutes or by running warm (not hot) tap water over the container for a few minutes.
- Do not heat breast milk directly on the stove or in the microwave.
- Test the temperature of the breast milk before feeding it to your baby by putting a few drops on your wrist. It should feel warm, not hot.
- Swirl the breast milk to mix the fat, which may have separated.
- If your baby did not finish the bottle, the leftover breast milk can still be used within 2 hours after the baby is finished feeding. After 2 hours, leftover breast milk should be discarded.
How to store breast milk
There are a couple of ways you can store breast milk. You can use a plastic or glass bottle with a sealable top. Or you can use a sterile, sealable bag. Store your breast milk in the amount your baby consumes in a feeding. This way you don’t waste any milk. For example, if your baby eats 4 ounces in a feeding, put 4 ounces of breast milk in the storage container. Always put a date on the container of breast milk so you know how long it will last.
Where should I store my breast milk?
Store your pumped breast milk in a refrigerator or cooler with ice as soon as possible. You also can freeze the milk if you aren’t going to use it right away.
How long can I store my breast milk?
The life of breast milk varies based on how it is stored.
- At room temperature (less than 77°F), it lasts up to 6 hours.
- In a cooler with ice packs, it lasts up to 24 hours.
- At the back of a refrigerator, it lasts for 3 to 8 days.
- At the back of a freezer, it lasts up to 6 months.
Why does my milk smell or taste soapy?
Sometimes thawed milk may smell or taste soapy. This is due to an enzyme in milk known as lipase 1). The milk is safe and most babies will still drink it. If there is a rancid smell from high lipase when the milk has been chilled or frozen, the milk can be heated to scalding (bubbles around the edges, not boiling) after expression, then quickly cooled and frozen. This deactivates the lipase enzyme. Scalded milk is still a healthier choice than commercial infant formula.
Why is my milk separating?
Human milk naturally separates into a milk layer and a cream top when it is stored. This is normal. It is safe to shake or swirl the milk to combine the cream prior to feeding.
How do I thaw and warm breast milk once I’m ready to use it?
To thaw frozen breast milk:
- Make sure the container is sealed tight.
- Put the container under running cold water.
- Pour the amount of thawed milk you need for your baby into a bottle for feeding.
- Use the thawed milk within 24 hours. Don’t refreeze breast milk after it’s been thawed.
To warm thawed or refrigerated milk:
- Put the container under running hot water or in a bowl of warm water.
- Pour the amount of milk you need for your baby into a bottle for feeding.
- Put a drop or two of milk on the back of your hand to test the temperature. If it’s too hot, let it cool.
Never heat breast milk in the microwave. It kills nutrients in the milk and can burn your baby’s mouth.
Is it safe to refreeze my milk after thawing?
Previously frozen milk that has been thawed can be kept in the refrigerator for up to 24 hours 2). There is currently limited research that supports the safety of refreezing breastmilk as this may introduce further breakdown of nutrients and increases the risk of bacterial growth. At this time, the accepted practice is not to refreeze thawed milk.
Can I reuse previously fed milk if my baby does not finish?
If baby does not finish the bottle during a feed, the recommendation is milk may be reused within 1-2 hours and after this time frame should be discarded to avoid transfer of bacteria from baby’s mouth to bottle 3). Many moms find storing milk in smaller quantities can help reduce waste if baby does not finish the bottle.
Expressed milk can be kept in a common refrigerator at the workplace or in a day care center. The US Centers for Disease Control and Prevention (CDC) and the US Occupational Safety and Health Administration agree that human milk is not among the body fluids that require special handling or storage in a separate container.
CDC does not list human breast milk as a body fluid to which universal precautions apply 4). Occupational exposure to human breast milk has not been shown to lead to transmission of HIV or Hepatitis B infection. However, because human breast milk has been implicated in transmitting HIV from mother to infant, gloves may be worn as a precaution by health care workers who are frequently exposed to breast milk (e.g., people working in human milk banks (defined below). For additional information regarding universal precautions as they apply to breast milk in the transmission of HIV and Hepatitis B infections, visit the following resources:
- Centers for Disease Control and Prevention. Perspectives in disease prevention and health promotion update: universal precautions for prevention of transmission of human immunodeficiency virus, Hepatitis B virus, and other bloodborne pathogens in health-care settings (https://www.cdc.gov/mmwr/preview/mmwrhtml/00000039.htm)
- Centers for Disease Control and Prevention. Recommendations for prevention of HIV transmission in health-care settings (https://www.cdc.gov/mmwr/preview/mmwrhtml/00023587.htm)
I have thrush; is my breast milk safe?
If you or your baby has a thrush or yeast/fungus infection, continue to breastfeed during the outbreak and treatment. While being treated, you can continue to express your milk and give it to your baby. Label any milk stored while you or baby is undergoing treatment. Be aware that refrigerating or freezing milk does not kill yeast. The safest, most conservative option is to discard pumped milk during thrush treatment. Some research shows using frozen milk pumped during thrush treatment should not pose any risk to healthy babies especially if the milk is boiled prior to use 5).
How long should a mother breastfeed?
The American Academy of Pediatrics recommends that infants be exclusively breastfed for about the first 6 months with continued breastfeeding along with introducing appropriate complementary foods for 1 year or longer. The World Health Organization (WHO) also recommends exclusive breastfeeding up to 6 months of age with continued breastfeeding along with appropriate complementary foods up to 2 years of age or longer.
Mothers should be encouraged to breastfeed their children for at least 1 year. The longer an infant is breastfed, the greater the protection from certain illnesses and long-term diseases. The more months or years a woman breastfeeds (combined breastfeeding of all her children), the greater the benefits to her health as well.
The American Academy of Pediatrics recommends that children be introduced to foods other than breast milk or infant formula when they are about 6 months old.
Will there be times that my baby needs more milk than I have ready?
Yes, your baby needs more milk during growth spurts. These occur at about 2 weeks and 6 weeks of age and again at about 3 months and 6 months of age. The best way to increase your milk supply for a growth spurt is to breastfeed or pump more often.
Can what I eat and drink affect my breast milk?
Yes. Nutrients in foods and drinks help make your breast milk healthy. When you’re breastfeeding, eat healthy foods, like fruits, vegetables, whole-grain breads and lean meats. Eat fewer sweets and salty snacks. You may need 450 to 500 extra calories a day when you’re breastfeeding to make breast milk for your baby.
Drink lots of water. It’s important to stay hydrated (have fluid in your body) when you’re breastfeeding. Drink when you’re thirsty. A simple way to make sure you drink enough water is to have a glass each time you breastfeed.
Limit caffeine when you’re breastfeeding. Caffeine is a drug that’s found in things like coffee, tea, soda, energy drinks, chocolate and some energy drinks and medicines. Too much caffeine in breast milk can make your baby fussy or have trouble sleeping. If you drink coffee, have no more than two cups a day while you’re breastfeeding.
Do I need to take vitamins or supplements when I’m breastfeeding?
Yes. Food is the best source of nutrients. But even if you eat healthy foods every day, you may not get all the nutrients you need. So you may need a little help from supplements. A supplement is a product you take to make up for certain nutrients that you don’t get enough of in food. For example, you may take a vitamin supplement to help you get more vitamin B or C. Or you may take an iron or calcium supplement.
When you’re breastfeeding, take a multivitamin every day or keep taking your prenatal vitamin. A multivitamin contains many vitamins (like vitamins B and C and folic acid) and minerals (like iron and calcium) that help your body stay healthy. A prenatal vitamin is a vitamin made for pregnant women. Don’t take any vitamin or supplement without talking to your provider first.
Here are some nutrients you may need supplements for during breastfeeding:
DHA is short for docosahexaenoic acid. DHA is a kind of fat called omega-3 fatty acid that helps with growth and development. If you’re breastfeeding, you need 200 to 300 milligrams of DHA each day to help your baby’s brain and eyes develop. You can get this amount from foods, like fish that are low in mercury, like herring, salmon, trout, anchovies and halibut. Or you can get it from foods that have DHA added to them, like orange juice, milk and eggs. If you don’t get enough DHA from food, you can take a DHA supplement. Talk to your provider to make sure you get the right amount of DHA each day.
Iodine. When you’re breastfeeding, you need 290 micrograms of iodine each day. Iodine in your breast milk helps your baby’s body make thyroid hormones that help his bones and nerves develop. You may not get enough iodine from food you eat. And not all multivitamins and prenatal vitamins contain iodine. So talk to your provider to make sure you’re getting enough iodine each day. You can get iodine by:
- Eating foods that are high in iodine, like fish, bread, cereal and milk products
- Taking an iodine or iodide supplement. Iodide is a form of iodine.
- Using iodized salt. This is salt that has iodine added to it. Read the package label to make sure your salt is iodized.
Vitamin B12. Vitamin B12 in your breast milk supports your baby’s brain development and helps him make healthy red blood cells. You can get vitamin B12 from foods, like meat, fish, eggs, milk and products made from milk. Or you may need a supplement. Ask your provider about taking a vitamin B12 supplement to make sure you and your baby get the right amount. You may need extra vitamin B12 if you:
- Are a strict vegetarian or vegan. A vegetarian is someone who doesn’t eat meat and mostly east foods that come from plants. A vegan is someone who doesn’t eat meat or anything made with animal products, like eggs or milk.
- Have had gastric bypass surgery. This is surgery on the stomach and intestines to help you lose weight.
- Have digestive conditions, like celiac disease or Crohn’s disease. These conditions affect how your body digests (breaks down) food.
Don’t take herbal products, like ginkgo or St. John’s wort, when you’re breastfeeding. Herbal products are made from herbs. Herbs are plants used in cooking and medicine. Even though herbs are natural, they may not be safe for your baby. It’s best not to use these products while you’re breastfeeding.
Can smoking while breastfeeding hurt my baby?
Yes. Don’t smoke if you’re breastfeeding. Nicotine is a drug found in cigarettes. It passes to your baby in breast milk and can cause problems, like:
- Making your baby fussy
- Making it hard for your baby to sleep
- Reducing your milk supply so your baby may not get all the milk he needs
Secondhand smoke also is bad for your baby. Secondhand smoke is smoke from someone else’s cigarette, cigar or pipe. It can cause lung and breathing problems. Babies of mothers who smoke are more likely than babies of non-smokers to die from sudden infant death syndrome (also called SIDS). SIDS is the unexplained death of a baby younger than 1 year old.
If you do smoke, it’s OK to breastfeed. But smoke as little as possible and don’t smoke around your baby.
Can I pass alcohol or street drugs to your baby through breast milk?
Yes. Don’t drink alcohol when you’re breastfeeding. Alcohol includes beer, wine, wine coolers and liquor. If you do drink alcohol, don’t have more than two drinks a week. Wait at least 2 hours after each drink before you breastfeed.
You also can pass street drugs, like heroin and cocaine, to your baby through breast milk. Tell your health care provider if you need help to quit using street drugs.
If you’re breastfeeding, don’t use marijuana. It’s not safe for your baby. You may pass THC and other chemicals from marijuana to your baby through breast milk. If you breastfeed your baby and smoke marijuana, your baby may be at increased risk for problems with brain development. Marijuana also may affect the amount and quality of breast milk you make. Even if marijuana is legal to use in your state, don’t use it when you’re breastfeeding.
Are prescription medicines safe to take when I’m breastfeeding?
Some are, and some aren’t. A prescription medicine (drug) is one your provider says you can take to treat a health condition. You need a prescription (an order from your provider) to get the medicine. Some prescription drugs, like medicine to help you sleep, some painkillers and drugs used to treat cancer or migraine headaches, aren’t safe to take while breastfeeding. Others, like certain kinds of birth control, may affect the amount of breast milk you make.
Here’s what you can do to make sure prescription medicine you take is safe for your baby when you’re breastfeeding:
- Talk to your health care provider and your baby’s provider about breastfeeding before your baby is born. Tell each provider about any medicine you take. If you take a medicine that’s not safe for your baby, your provider may switch you to a safer one. Don’t start or stop taking any medicine during breastfeeding without talking to your providers first.
- Make sure any doctor who prescribes you medicine knows that you’re breastfeeding.
- Check with your provider even if you take medicine that’s usually prescribed for your baby, like baby aspirin.
- Tell your baby’s doctor if your baby has any signs that may be a reaction to your medicine, like diarrhea, sleepiness, a change in eating or crying more than usual.
If you have a chronic health condition and you plan to breastfeed, talk to your providers about how your condition affects breastfeeding. You most likely can breastfeed even with a chronic health condition. Your provider can help you make sure that any medicine you take is safe for your baby. A chronic health condition is one that lasts for 1 year or more. It needs ongoing medical care and can limit a person’s usual activities and affect daily life. Examples are diabetes, high blood pressure, obesity and depression. Chronic health conditions need treatment from a health care provider.
Is it safe to take prescription opioids when I’m breastfeeding?
Prescription opioids are painkillers your provider may prescribe if you’ve been injured or had surgery or dental work. They’re sometimes used to treat a cough or diarrhea. If you had an episiotomy or a cesarean birth (also called a c-section), your provider may prescribe an opioid like codeine or tramadol to help relieve your pain. An episiotomy is a cut made at the opening of the vagina to help let your baby out. A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus (womb).
Opioid use during pregnancy is the most common cause of neonatal abstinence syndrome also called NAS. Neonatal abstinence syndrome is a group of conditions caused when a baby withdraws from certain drugs she’s exposed to in the womb before birth. If your baby has neonatal abstinence syndrome, breastfeeding may help make her symptoms less severe. This may help her need less medicine and be able to leave the hospital sooner. If your baby has neonatal abstinence syndrome, talk to your provider and your baby’s provider about breastfeeding and how to make sure it’s safe for your baby.
If you’re using prescription opioids with your doctor’s supervision, you can breastfeed depending on the opioid you take. Some opioids can cause life-threatening problems for your baby. Make sure the provider who prescribes you the opioid knows you’re breastfeeding, and take the medicine exactly as our provider tells you to. If you take any of these opioids, talk to your provider about switching to a safer medicine:
- Codeine or medicines that contain codeine
- Hydrocodone
- Meperidine
- Oxycodone
- Tramadol
If you’re in treatment for opioid use disorder with medicines like methadone or buprenorphine (also called medication-assisted therapy or MAT or opioid-assisted therapy or OAT), you can breastfeed your baby if:
- Your health is stable and you’re no longer misusing opioids or using street drugs, like cocaine or marijuana.
- You don’t have HIV (stands for human immunodeficiency virus. HIV is the virus that causes AIDS (stands for acquired immunodeficiency syndrome).
- Your treatment is closely supervised and monitored.
- You have social support from friends and family throughout your treatment.
- Your baby continues to gain weight as you breastfeed.
If you’re breastfeeding and taking tramadol, codeine or medicines that contain codeine, call your baby’s doctor or emergency services number right away if your baby:
- Is sleepier than usual. Breastfed babies usually eat every 2 to 3 hours and shouldn’t sleep more than 4 hours at a time.
- Is limp
- Has trouble breathing
- Has trouble breastfeeding
Are over-the-counter medicines safe to take when you’re breastfeeding?
Most over-the-counter also called OTC medicine, like pain relievers and cold medicine, are OK to take when you’re breastfeeding. For example, OTC pain relievers like ibuprofen (Advil®) or acetaminophen (Tylenol®) are safe to use when breastfeeding.
Here’s what you can do to help make sure an OTC medicine is safe for your baby:
- Don’t take an OTC medicine during breastfeeding without talking to your provider first. If you take a medicine that’s not safe for your baby, your provider can recommend a safer one.
- Read the label on the package for information about how an OTC drug may affect breastfeeding.
- Take the smallest dose (amount) of medicine to help lessen the amount that gets passed to your baby in breast milk.
- Don’t take medicine that is extra-strength, long-acting (you take it just once or twice a day) or multi-symptom (treats more than one symptom). These medicines may have larger doses that stay in your body and breast milk longer than medicines with smaller doses.
- Tell your baby’s doctor if your baby has signs of reaction, like diarrhea, sleepiness, a change in eating, or crying more than usual.
What medical conditions make breastfeeding unsafe for your baby?
Breastfeeding may be harmful to a baby if:
- Your baby has galactosemia. Babies with this genetic condition can’t digest the sugar in breast milk (or any kind of milk). They can have brain damage or even die if they eat or drink breast milk, milk or anything made with milk. Babies with galactosemia need to eat a special formula that is not made with milk of any kind. Your baby gets tested for this condition soon after birth as part of newborn screening.
- You have human immunodeficiency virus (HIV). You can pass HIV to your baby through breast milk. Note: recommendations about breastfeeding and HIV may be different in other countries 6).
- You have cancer and are getting treated with medicine or radiation.
- You have human T-cell lymphotropic virus type I or type II 7). This is a virus that can cause blood cancer and nerve problems.
- You have untreated, active tuberculosis. This is an infection that mainly affects the lungs.
- You have Ebola, a rare but very serious disease that can cause heavy bleeding, organ failure and death. It’s spread by coming in contact with body fluids from a person who has the disease. A mother who has Ebola should not have close contact—including breastfeeding—with her baby. This can help keep her baby safe from the disease. While the virus has been found in breast milk, we don’t know for sure if you can pass Ebola to your baby through breast milk.
- You are using an illicit street drug, such as PCP (phencyclidine) or cocaine1 (Exception: Narcotic-dependent mothers who are enrolled in a supervised methadone program and have a negative screening for HIV infection and other illicit drugs can breastfeed)
Mothers should temporarily NOT breastfeed and should NOT feed expressed breast milk to their infants if:
- Mother is infected with untreated brucellosis 8).
- Mother is taking certain medications 9).
- The mother is undergoing diagnostic imaging with radiopharmaceuticals 10).
- Mother has an active herpes simplex virus (HSV) infection with lesions present on the breast 11). Note: Mothers can breastfeed directly from the unaffected breast if lesions on the affected breast are covered completely to avoid transmission.
Mothers should temporarily NOT breastfeed, but CAN feed expressed breast milk if:
- Mother has untreated, active tuberculosis 12). Note: The mother may resume breastfeeding once she has been treated appropriately for 2 weeks and is documented to be no longer contagious.
- Mother has active varicella (chicken pox) infection that developed within the 5 days prior to delivery to the 2 days following delivery 13).
If you’ve had breast surgery or piercing, it’s most likely safe to breastfeed. Breast surgery includes getting implants, having a breast reduction or having a lump removed. Piercing means inserting jewelry into the breast, including nipple piercing. If you’ve had surgery or piercing, talk to your doctor or lactation consultant. A lactation consultant is a person with special training in helping women breastfeed.
If I’ve been exposed to lead, is it safe to breastfeed?
It depends on the amount of lead you have in your body. Lead is a metal that comes from the ground, but it can be in the air, water and food. You can’t see, smell or taste it. High levels of lead in your body called lead poisoning can cause serious health problems.
If you think you’ve been exposed to lead and are breastfeeding or planning to breastfeed, tell your provider. She can test your lead levels to see if breastfeeding is safe for your baby. If you have more than 40 micrograms/dL of lead in your system, it’s not safe to breastfeed. Pump your breast milk and throw it out until your lead levels are safe.
What are human milk banks?
Human milk banks are a service established for the purpose of collecting milk from donors and processing, screening, storing, and distributing donated milk to meet the specific needs of individuals for whom human milk is prescribed by licensed health care providers. When possible, human milk banks also serve healthy infants who have been adopted or are not able to get their own mother’s milk.
Is it safe for families to buy breast milk on the internet?
The American Academy of Pediatrics (https://www.aappublications.org/content/34/12/29.6) and the Food and Drug Administration (https://www.fda.gov/science-research/pediatrics/use-donor-human-milk) recommend avoiding Internet-based milk sharing sites and instead recommend contacting milk banks. Research 14) has demonstrated that some milk samples sold online have been contaminated with a range of bacteria.
Nonprofit donor human milk banks, where processed human milk comes from screened donors, have a long safety record in North America. All member banks of the Human Milk Banking Association of North America (HMBANA) must operate under specific evidence-based guidelines that require extensive testing and processing procedures as well as self-reported health information and a health statement from both the donor’s health care provider and the infant’s health care provider. Because most of the milk from milk banks is given to hospitalized and fragile infants, milk banks may not have enough to serve healthy infants at all times. To find a human milk bank, contact HMBANA (https://www.hmbana.org).
References [ + ]