Fetal development timeline
A normal pregnancy lasts nine months (280 days). Each three-month period of pregnancy is called a trimester. During each trimester, the fetus grows and develops.
The actual embryo or fetal age also known as “conceptual age” is the time elapsed from fertilization (the union of an egg and a sperm into a single cell) of the egg near the time of ovulation . However, because most women do not know when ovulation occurred, but do know when their last menstrual period (LMP) began, the time elapsed since the first day of the last normal menstrual period (LNMP), the menstrual age, is used to determine the age of a pregnancy. The menstrual age is also known as the gestational age. Gestational age is conventionally expressed as completed weeks. Therefore, a 36 week, 6 day fetus is considered to be a 36 week fetus 1).
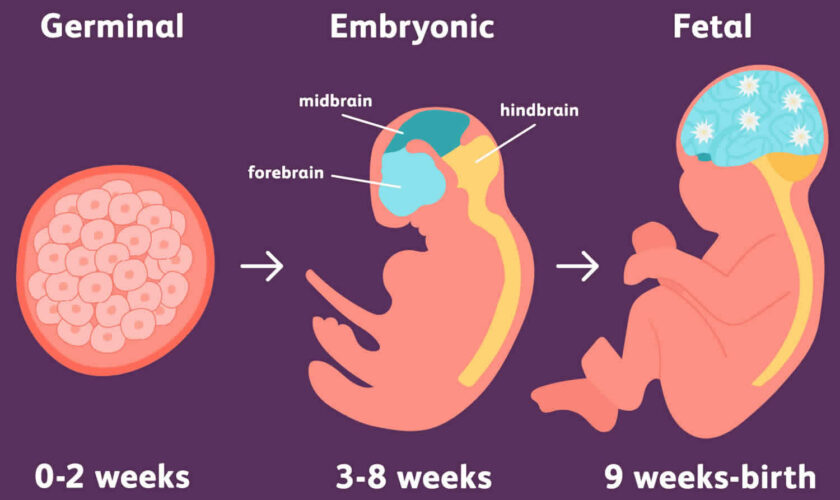
Pregnancy begins when a man’s sperm fertilizes a woman’s egg. Fertilization takes place in the fallopian tube. Over the next few days, the single cell divides into multiple cells. At the same time, the small cluster of dividing cells moves through the fallopian tube to the lining of the uterus. There it implants and starts to grow. From implantation until the end of the eighth week of pregnancy, it is called an embryo. From the ninth week of pregnancy until birth, it is called a fetus.
Since you don’t always know when fertilization occurred, doctors calculate pregnancy based on the first day of your last menstrual period (LMP). A normal pregnancy lasts about 40 weeks from the first day of your last menstrual period (LMP). Your doctor will count forward 40 weeks from your LMP to estimate the due date. Pregnancy is assumed to start 2 weeks after the first day of the LMP. Therefore, an extra 2 weeks is counted at the beginning of your pregnancy when you are not actually pregnant. Pregnancy “officially” lasts 10 months (40 weeks)—not 9 months—because of these extra weeks. Most births occur between weeks 38 and 42. If you have an ultrasound early in your pregnancy, your doctor may measure the baby to determine your due date instead.
The day your baby is due is called the estimated due date (EDD). Only about 1 in 20 women give birth on their due dates. Still, the estimated due date (EDD) is useful for a number of reasons. It determines your fetus’s gestational age throughout pregnancy so that the fetus’s growth can be tracked. It also provides a timeline for certain tests that you will have throughout your pregnancy.
Your estimated due date (EDD) is calculated from the first day of your last menstrual period (LMP). But when the date of the LMP is uncertain, an ultrasound exam may be done during the first trimester to estimate the due date. If you have had in vitro fertilization, the estimated due date (EDD) is set by the age of the embryo and the date that the embryo is transferred to the uterus.
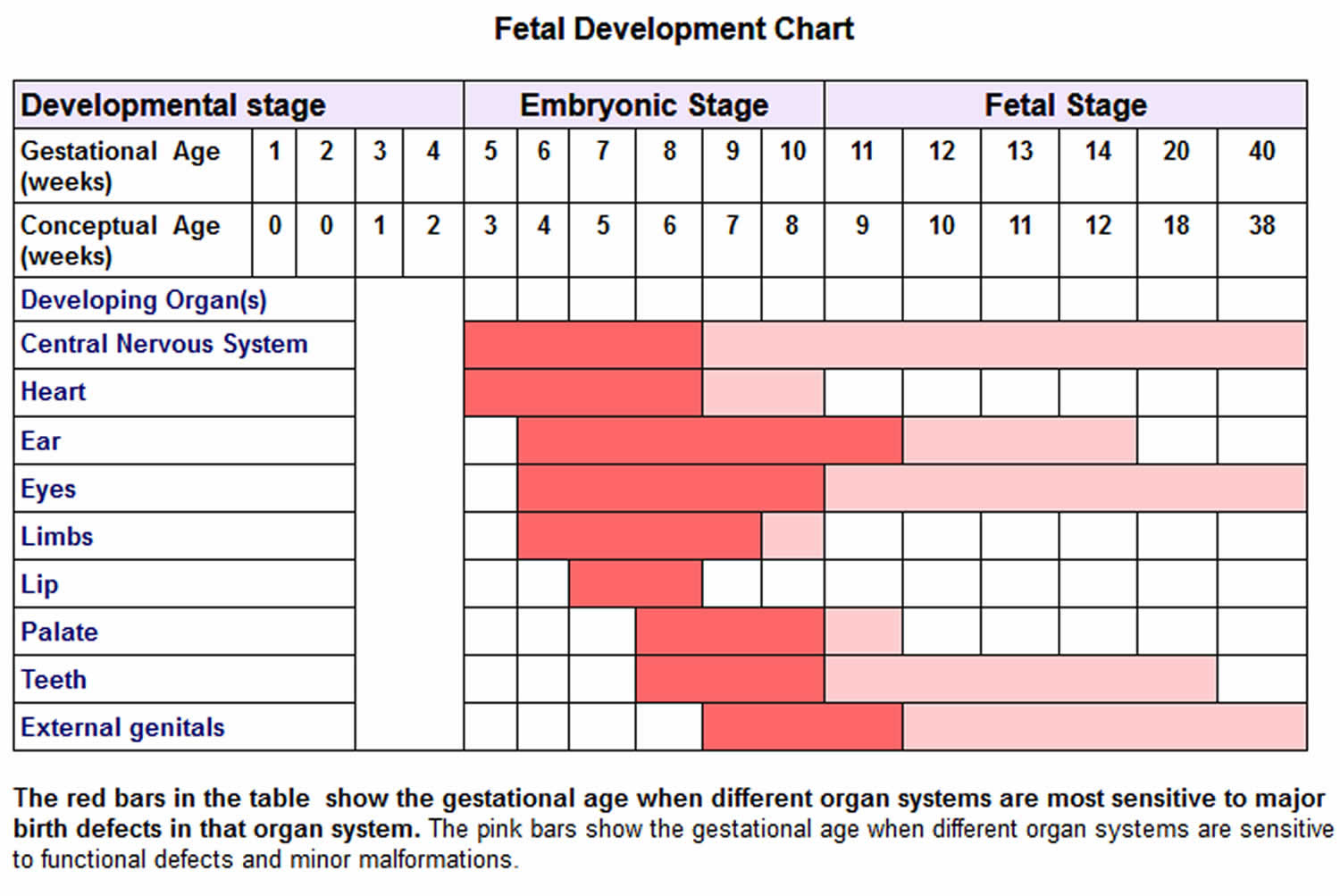
Figure 1. Fetal development chart
First trimester (week 1–week 12)
Pregnancy begins when a man’s sperm fertilizes a woman’s egg. Since you don’t always know when fertilization occurred, doctors calculate pregnancy based on the first day of your last menstrual period (LMP). Your doctor will count forward 40 weeks from your LMP to estimate the due date. Most births occur between weeks 38 and 42. If you have an ultrasound early in your pregnancy, your doctor may measure the baby to determine your due date instead.
After conception, your baby begins a period of dramatic change known as the embryonic stage. This stage runs from the 5th through the 10th week of pregnancy. During this stage, the baby is called an embryo.
There are numerous changes that occur during the embryonic stage. First, the cells of the embryo called embryonic stem cells multiply and develop. They become the hundreds of different types of cells needed to make a whole human body. Your baby’s major organs and body parts begin to take shape.
The placenta forms during the embryonic stage. The placenta takes nutrients, oxygen, and water from your blood and passes these along to your baby through the umbilical cord. It also removes the baby’s wastes. The placenta will filter out most of the harmful substances that may be present in your body.
The amniotic sac forms during this stage as well. It is filled with amniotic fluid, which surrounds and protects your baby in the uterus.
Below are some of the highlights that occur during the embryonic stage.
- Nervous system. This is one of the first things to develop. It includes the formation of your baby’s brain, spinal cord, and nerves.
- Heart. An S-shaped tube forms on the front of the embryo. This will become your baby’s heart. At first the heart does not beat, but soon it starts beating and pumping an early form of blood.
- Face. Your baby’s facial features begin to take shape. The eyes and ears form on the sides of the head and are linked to the brain. The eyes move forward on the face, and eyelids form to protect the developing eyes. Pieces of tissue grow and join together to create the forehead, nose, cheeks, lips, and jaw. The nasal passages, mouth, and tooth buds form the baby’s first teeth. A tongue with taste buds also forms.
- Arms and legs. At first, your baby’s arms and legs begin as little buds that sprout from the embryo’s sides. As they grow, the arms look like paddles and the legs look like flippers. A ridge appears on the end of each one. They eventually become your baby’s fingers and toes.
- Sexual organs. Cells form to become your baby’s eggs or sperm. Your baby’s penis or vagina is visible at the end of the embryonic period. However, it is still too soon to tell on an ultrasound if your baby is a girl or boy.
- Muscles and movement. Muscles develop and the embryo begins to move. At first it’s only twitching and reacting to touch. Once the nerves and muscles start working together, your baby can start moving on purpose.
By the end of the embryonic stage at week 10, your baby will be about 1 inch long. That’s still too small for you to feel your baby’s movements. You’ll probably feel them starting in the middle of the second trimester.
After the embryonic stage, the fetal stage begins and your baby is called a fetus. This stage runs from the 11th week until birth. Your baby will grow longer and gain weight quicker. Their organs and body parts will continue to develop.
The last 2 to 3 weeks of the first trimester are the beginning of the fetal stage. In those weeks, fingernails and toenails begin to form and the kidneys start working. By the end of the first trimester, your baby has tripled in length to about 3 inches long.
Second trimester (week 13–week 28)
From the moment of conception to the time of delivery, your growing baby goes through several stages of development. The middle part of your pregnancy is called the second trimester. It is made up of weeks 13 or 14 through weeks 26 or 27. The timeframe can vary based on your doctor. During this time, your baby continues to grow and change almost daily. Here is a summary of how your baby develops during the second trimester.
When the second trimester starts, your baby is about 3 inches long. Your doctor might tell you your baby measures a certain length “from crown to rump.” This means your baby is being measured from the top of its head to its bottom (instead of head to toe) because the legs are curled up to the baby’s stomach.
At the beginning of the second trimester, your baby’s head is the biggest part of his or her body. During the next few weeks, the rest of your baby’s body will get longer in order to catch up. By the end of the second trimester, your baby may be 9 inches — or even longer.
Below are other highlights of the second trimester.
- Your baby will start to hear certain sounds, such as your heartbeat, by about the 18th week of pregnancy. Your baby’s hearing will continue to improve and they will be able to hear your voice.
- Your baby’s eyes may open as early as the 20th week. Before this, the eyelids have been sealed shut. However, your baby’s eyes cannot see anything until the third trimester.
- Your baby will have fingerprints and footprints by the end of the second trimester.
- Fine hair and a white waxy substance cover and protect your baby’s skin. The skin is thin, loose, and wrinkled. In the third trimester, some fat will start to fill in under the skin.
- Your baby’s digestive system will start to function. The baby also will begin to produce and release urine, which becomes amniotic fluid.
- By the middle of your second trimester, the baby’s sex should be clear. If you have an ultrasound, you should be able learn your baby’s sex, if you want. Keep in mind your baby has to be in an ideal position for the doctor or technician to see the sex organs.
Things to consider
Your baby is moving almost all the time throughout your pregnancy. However, you won’t start to feel it until about the 20th week. At first, you may notice a fluttering feeling. It can be hard to tell if this is your baby or something else. Soon enough, the movements will become very noticeable. Your partner may be able to feel the baby move as well. You might even be able to see your belly move when your baby “kicks.”
Your baby’s movements are helping them prepare for life outside your body. Muscles grow stronger as your baby learns to kick, suck, and open and close their hands. Your baby also practices making faces, such as frowning, smiling, and squinting.
Third trimester (week 29–week 40)
By the end of the second trimester, all of your baby’s organs and body parts are present and working. The final part of your pregnancy is the third trimester. It is weeks 27 through birth. During this time, your baby is grows and matures.
In the third trimester, your baby’s senses continue to progress. Your baby uses its senses of hearing and touch to learn about its body and your womb. They still can’t see much, though. Their eyes can detect bright light, but it’s too dark to see in the uterus. Your baby hears and knows your voice and may move in response to music. Your baby also starts to practice important movements, including grasping and sucking. They may even start sucking on their thumb.
Other highlights of the third trimester:
- By the end of the third trimester, your baby has eyelashes and eyebrows. They may have a full head of hair or be bald. Nails have grown to the tips of the fingers and toes.
- The white waxy substance and fine hair that covered and protected your baby’s skin has begun to fall off. You may see some of the leftover hair after your baby is born. Most of this usually is gone within the first few weeks of life.
- Most babies move to a head-down position in the uterus toward the end, with the head on the mother’s pubic bone.
- The lungs are the last major organ to finish developing. When fully mature, they produce a chemical that affects the hormones in your body. Doctors are not sure why labor starts, but this chemical may be one of the causes.
Will my baby be big enough to survive if they are born before my due date?
Your due date is an estimate. Only 5 percent of babies are born on their actual due dates. Your baby is “full-term” (not premature) if they are born during or after week 37. If this is your first pregnancy, your baby is likely to be born after your due date.
If your baby is born earlier, near the beginning of the third trimester, they are likely to survive. However, the longer the baby is in your womb, the better.
Will I still feel my baby move?
You’ll feel your baby kicking, punching, and moving often in the early weeks of the third trimester. Later, as your baby gets larger, you’ll feel more stretches and rolls, and fewer kicks and punches.
As your uterus gets more crowded, you may feel your baby move less. If you think your baby is less active than usual, do a “kick count”. Keep track of the number of movements in one hour. If your baby moves fewer than 10 times in an hour, call your doctor.
How big will my baby grow during the third trimester?
As your baby grows, they add layers of fat to provide warmth after birth. The fat fills the extra space under the skin, making the skin less wrinkled. At birth, most babies weigh between 6 and 9 pounds. They are usually between 19 and 21 inches long.
Fetal development timeline week by week
Gestation is the period of time between conception and birth when a baby grows and develops inside the mother’s womb. Because it’s impossible to know exactly when conception occurs, gestational age is measured from the first day of the mother’s last menstrual cycle to the current date. It is measured in weeks.
This means that during weeks 1 and 2 of pregnancy, a woman is not yet pregnant. This is when her body is preparing for a baby. A normal gestation lasts anywhere from 37 to 42 weeks.
Week 1 to 2
- The first week of pregnancy starts with the first day of a woman’s menstrual period. She is not yet pregnant.
- During the end of the second week, an egg is released from an ovary. This is when you are most likely to conceive if you have unprotected intercourse.
During the first two weeks after the last menstrual period egg follicles mature in the ovaries under the stimulus of follicle-stimulating hormone (FSH) a hormone secreted by the pituitary gland in the brain. High levels of the hormone estradiol, produced by the developing egg follicle, cause secretion of luteinizing hormone (LH) ,yet another hormone from the pituitary gland. LH causes release of the egg from its follicle (ovulation)
For women with 28-day cycles, ovulation usually occurs on days 13 to 15.
Conception also called fertilization usually happens about 2 weeks after the start of your last menstrual period (also called LMP). Conception is when a man’s sperm fertilizes a woman’s egg. Conception happens in one of your fallopian tubes. These are the tubes between your ovaries and your uterus (womb).
You may not know the exact day you get pregnant. This is why health care providers use your ast menstrual period to find out how far along you are in pregnancy.
Week 3 (Gestational Age 3 weeks or Embryonic Age 1 week)
- During intercourse, sperm enters the vagina after the man ejaculates. The strongest sperm will travel through the cervix (the opening of the womb, or uterus), and into the fallopian tubes.
- A single sperm and the mother’s egg cell meet in the fallopian tube. When the single sperm enters the egg, conception occurs. The combined sperm and egg is called a zygote.
- The zygote contains all of the genetic information (DNA) needed to become a baby. Half the DNA comes from the mother’s egg and half from the father’s sperm.
- The zygote spends the next few days traveling down the fallopian tube. During this time, it divides to form a ball of cells called a blastocyst.
- A blastocyst is made up of an inner group of cells with an outer shell.
- The inner group of cells will become the embryo. The embryo is what will develop into your baby.
- The outer group of cells will become structures, called membranes, which nourish and protect the embryo.
The fertilized egg also called a zygote will begin producing the hormone human chorionic gonadotropin (hCG) the pregnancy hormone. Human chorionic gonadotropin (hCG) first becomes detectable in the mother’s blood and urine between 6 and 14 days after fertilization (3 to 4 weeks gestational age). During the 3rd week the sex of the fetus is determined by the father’s sperm, and twins may be formed. Fatigue and swollen or tender breasts are sometimes the first signs of pregnancy.
Week 4 (Gestational Age 4 weeks or Embryonic Age 2 weeks)
- Once the blastocyst reaches the uterus, it buries itself in the uterine wall (also called implantation).
- At this point in the mother’s menstrual cycle, the lining of the uterus is thick with blood and ready to support a baby.
- The blastocyst sticks tightly to the wall of the uterus and receives nourishment from the mother’s blood.
Week 5 (Gestational Age 5 weeks or Embryonic Age 3 weeks)
- Week 5 is the start of the “embryonic period” which lasts from the the 5th to the 10th week. This is when all the baby’s major systems and structures develop.
- The embryo’s cells multiply and start to take on specific functions. This is called differentiation.
- Blood cells, kidney cells, and nerve cells all develop.
- The embryo grows rapidly, and the baby’s external features begin to form.
- Your baby’s brain, spinal cord, and heart begin to develop.
- Tiny buds start to appear that become your baby’s arms and legs.
- Baby’s gastrointestinal tract starts to form.
- It is during this time in the first trimester that the baby is most at risk for damage from things that may cause birth defects. This includes certain medicines, illegal drug use, heavy alcohol use, infections such as rubella, and other factors.
Weeks 6 (Gestational Age 6 weeks or Embryonic Age 4 weeks)
- The embryo is now about the size of a pea.
- The average crown to rump length is about 0.2 inches (0.4 cm)
- The eyes, nostrils, and arms are taking shape.
- The heart is beating at about 110 beats per minute and sometimes may be seen using a transvaginal ultrasound at this time.
Weeks 7 (Gestational Age 7 weeks or Embryonic Age 5 weeks)
- The embryo is now about 0. 4 inches (1 cm ) long.
- Arm and leg buds start to grow.
- Your baby’s brain forms into 5 different areas. Some cranial nerves are visible.
- Your baby’s eyes, nose, mouth, fingers, toes and ears are forming and begin to take shape.
- Tissue grows that will become your baby’s spine and other bones.
- Baby’s heart continues to grow and now beats at a regular rhythm (about 120 times a minute). This can be seen by vaginal ultrasound.
- Blood pumps through the main vessels.
- Your baby’s bones start to form but are still soft. They harden as you get farther along in your pregnancy.
- Your baby has eyelids, but they stay shut.
- Your baby’s genitals begin to form.
- By week 7 the trachea and bronchi of the lungs have formed and the pseudoglandular stage of lung development begins 2)
- Movement of the embryo can be detected by ultrasound.
- Crown–rump length of 7 mm or greater and no heartbeat, or mean sac diameter of 25 mm or greater and no embryo is considered consistent with early pregnancy loss 3)
Week 8 (Gestational Age 8 weeks or Embryonic Age 6 weeks)
- The average embryo at 8 weeks is 0.6 inches (1.6 cm) long and weighs less than 1/2 ounce (15 grams).
- Baby’s arms and legs have grown longer.
- Hands and feet begin to form and look like little paddles.
- Your baby’s brain continues to grow.
- The lungs start to form.
- In a process is called physiological gut herniation, the intestine elongates and moves outside of the abdomen herniating into the base of the umbilical cord and rotate counter-clockwise at about 8 weeks . The intestine returns into the fetal abdomen by about 12 weeks 4).
- The placenta is working.
Week 9 (Gestational Age 9 weeks or Embryonic Age 7 weeks)
- The average embryo at 9 weeks is 0.9 inches (2.3 cm) long and weighs less than 1/2 ounce (15 grams).
- Nipples and hair follicles form.
- Arms grow and elbows develop.
- Baby’s toes can be seen.
- All baby’s essential organs have begun to grow.
- Tiny buds appear that become your baby’s teeth.
- The heart is beating at about 170 beats per minute.
Week 10 (Gestational Age 10 weeks or Embryonic Age 8 weeks)
- The average fetus at 10 weeks is 1.2 inches (3.2 cm) long and weighs 1.2 ounces (35 grams).
- The embryo’s tail has disappeared and it is now called a fetus. Fingerprints are being formed 5) and bone cells are replacing cartilage.
- Your baby’s eyelids are more developed and begin to close.
- The outer ears begin to take shape.
- Baby’s facial features become more distinct.
- The intestines rotate.
- Fingers and toes continue to develop and your baby’s nails grow.
- You may be able to hear your baby’s heartbeat at your prenatal care checkup.
- At the end of the 10th week of pregnancy, your baby is no longer an embryo. It is now a fetus, the stage of development up until birth.
Week 11 (Gestational Age 11 weeks or Embryonic Age 9 weeks)
- The average fetus at 11 weeks is 1.6 inches (4.2 cm) long and weighs 1.6 ounces (45 grams).
- The fetus is starting to have breathing movements. It can open its mouth and swallow.
Weeks 12 (Gestational Age 12 weeks or Embryonic Age 10 weeks)
- The average fetus at 12 weeks is 2.1 inches (5.3 cm) long and weighs 2 ounces (58 grams).
- The fetus is starting to make random movements.
- The fetus begins to concentrate iodine in its thyroid and produce thyroid hormone at about this time.
- The pancreas is beginning to make insulin, and the kidneys are producing urine. The heart beat can usually be heard with and electronic monitor at this time.
Weeks 13 (Gestational Age 13 weeks or Embryonic Age 11 weeks)
- The average fetus at 13 weeks is 2.5 inches (6.5 cm) long and weighs 2.6 ounces (73 grams).
- Your baby’s eyelids close and will not reopen until about the 28th week.
- Baby’s face is well-formed.
- Limbs are long and thin.
- Nails appear on the fingers and toes.
- Genitals appear.
- Baby’s liver is making red blood cells.
- The head is very large — about half of baby’s size.
- Your little one can now make a fist.
- Tooth buds appear for the baby teeth.
- Your baby’s nose and taste buds are developing.
- Her skin starts to thicken, and hair follicles under her skin begin to grow.
- Your baby opens and closes her hands and brings them to her mouth.
- All major organs are formed now, but they are too immature for the fetus to survive out of the womb.
- Physiological gut herniation should be complete by this time
- The fetal bladder can be consistently seen using ultrasound after 13 weeks 6).
Weeks 14 (Gestational Age 14 weeks or Embryonic Age 12 weeks)
- The average fetus at 14 weeks is 3.1 inches (7.9 cm) long and weighs 3.3 ounces (93 grams)
- The fetus’s toenails are appearing. The gender may sometimes be seen
- Your baby’s eyelids close and will not reopen until about the 28th week.
- Baby’s face is well-formed.
- Limbs are long and thin.
- Nails appear on the fingers and toes.
- Genitals appear.
- Baby’s liver is making red blood cells.
- The head is very large — about half of baby’s size.
- Your little one can now make a fist.
- Tooth buds appear for the baby teeth.
- Your baby’s nose and taste buds are developing.
- Her skin starts to thicken, and hair follicles under her skin begin to grow.
- Your baby opens and closes her hands and brings them to her mouth.
- All major organs are formed now, but they are too immature for the fetus to survive out of the womb.
Weeks 15 (Gestational Age 15 weeks or Embryonic Age 13 weeks)
- The average fetus at 15 weeks is 6.4 inches (16.4 cm) long and weighs 4.1 ounces (117 grams).
- Fetal movement may be sensed now (called quickening). Some mothers don’t feel the fetus moving until about 25 weeks.
Weeks 16 to 17 (Gestational Age 16 to 17 weeks or Embryonic Age 14 to 15 weeks)
- The average 16 week fetus is 7.1 inches (18.3 cm) long and weighs 5.2 ounces (146 grams).
- The average 17 week fetus is 7.9 inches (20.1 cm) long and weighs 6.4 ounces (181 grams).
- Hearing is beginning to form 7)
- The canalicular period of lung development has started and will continue until 25 weeks 8)
- The pseudoglandular stage of lung development ends at about 17 weeks. There are still NO ALVEOLI (the air sacs in the lungs where the exchange of oxygen and carbon dioxide occurs), so respiration is not possible at this time 9).
Weeks 18 (Gestational Age 18 weeks or Embryonic Age 16 weeks)
- The average 18 week fetus is 8.6 inches (22 cm) long and weighs 7.9 ounces (223 grams).
- The ears are standing out, and the fetus is beginning to respond to sound.
- The cerebellar vermis can be demonstrated to be fully formed on ultrasound 10).
- At this stage, baby’s skin is almost transparent.
- Fine hair called lanugo develops on baby’s head.
- Muscle tissue and bones keep developing, and bones become harder.
- Baby begins to move and stretch.
- The liver and pancreas produce secretions.
- Your little one now makes sucking motions.
Weeks 19 (Gestational Age 19 weeks or Embryonic Age 17 weeks)
- The average fetus at 19 weeks is 9.3 inches (23.7 cm) long and weighs 9.6 ounces (273 grams).
- The ears, nose and lips are now recognizable.
Weeks 20 (Gestational Age 20 weeks or Embryonic Age 18 weeks)
- The average fetus at 20 weeks is 9.9 inches (25.5 cm) long and weighs 11.7 ounces (331 grams).
- The fetus is covered in fine hair called lanugo, has some scalp hair, and is capable of producing IgG and IgM ( two types of antibodies)
Weeks 21 (Gestational Age 21 weeks or Embryonic Age 19 weeks)
- The average fetus at 21 weeks is 10.6 inches (27.2 cm) long and weighs 14.1 ounces (399 grams).
- Your baby can hear.
- The baby is more active and continues to move and float around.
- The mother may feel a fluttering in the lower abdomen. This is called quickening, when mom can feel baby’s first movements.
- By the end of this time, baby can swallow.
- The fetus is now able to suck and grasp, and may have bouts of hiccups.
- Some women may begin feeling Braxton Hicks contractions at this time.
Week 22 (Gestational Age 22 weeks or Embryonic Age 20 weeks)
- The average fetus at 22 weeks is 11.2 inches (28.8 cm) long and weighs 1.1 pound (478 grams).
- Survival out of the womb at this age would be expected to be ~9%.
- Survival without major morbidity among infants surviving to discharge would be expected to be 0% 11)
- Lanugo hair covers baby’s entire body.
- Meconium, baby’s first bowel movement, is made in the intestinal tract.
- Eyebrows and lashes appear.
- The baby is more active with increased muscle development.
- The mother can feel the baby moving.
- Baby’s heartbeat can be heard with a stethoscope.
- Nails grow to the end of baby’s fingers.
Weeks 23 (Gestational Age 23 weeks or Embryonic Age 21 weeks)
- The average fetus at 23 weeks is 11.9 inches (30.4 cm) long and weighs 1.2 pounds (568 grams).
- The fetus is having rapid eye movements (REM) during sleep.
- The entire corpus callosum may not be be seen using transabdominal ultrasound before this age 12)
- Survival out of the womb at this age would be expected to be ~33%.
- Survival without major morbidity* among infants surviving to discharge would be expected to be ~2% 13)
Weeks 24 (Gestational Age 24 weeks or Embryonic Age 22 weeks)
- The average fetus at 24 weeks is 12.5 inches (32 cm) long and weighs 1.5 pounds (670 grams).
- The terminal saccular stage of lung development has started 14)
- Survival out of the womb at this age would be expected to be ~65%.
- Survival without major morbidity* among infants surviving to discharge would be expected to be ~ 9% 15)
Weeks 25 (Gestational Age 25 weeks or Embryonic Age 23 weeks)
- The average fetus at 25 weeks is 13.1 inches (33.6 cm) long and weighs 1.7 pounds (785 grams).
- The canalicular period of lung development is ending. Respiration is possible towards the end of this period 16)
- Survival out of the womb at this age would be expected to be ~81%.
- Survival without major morbidity* among infants surviving to discharge would be expected to be ~ 25% 17)
- Bone marrow begins to make blood cells.
- The lower airways of the baby’s lungs develop.
- Your baby begins to store fat.
Week 26 (Gestational Age 26 weeks or Embryonic Age 24 weeks)
- The average fetus at 26 weeks is 13.7 inches (35.1 cm) long and weighs 2 pounds (913 grams).
- Survival out of the womb at this age would be expected to be ~87%.
- Survival without major morbidity* among infants surviving to discharge would be expected to be ~ 29% 18)
- Eyebrows and eyelashes are well-formed.
- All parts of baby’s eyes are developed.
- Your baby may startle in response to loud noises.
- Footprints and fingerprints are forming.
- Air sacs form in baby’s lungs, but lungs are still not ready to work outside the womb.
Weeks 27 (Gestational Age 27 weeks or Embryonic Age 25 weeks)
- The average fetus at 27 weeks is 14.2 inches (36.5 cm) long and weighs 2.3 pounds (1055 grams).
- Survival out of the womb at this age would be expected to be ~94%. Survival without major morbidity among infants surviving to discharge would be expected to be ~ 50% 19)
Weeks 28 (Gestational Age 28 weeks or Embryonic Age 26 weeks)
- The average fetus at 28 weeks is 14.8 inches (37.9 cm) long and weighs 2.7 pounds (1210 grams).
- Survival out of the womb at this age would be expected to be ~94%.
- Survival without major morbidity among infants surviving to discharge would be expected to be ~ 59% 20)
- Baby’s brain grows rapidly.
- The nervous system is developed enough to control some body functions.
- Your baby’s eyelids can open and close.
- The respiratory system, while immature, produces surfactant. This substance helps the air sacs fill with air.
Weeks 29 to 30 (Gestational Age 29 to 30 weeks or Embryonic Age 27 to 28 weeks)
- The average fetus at 29 weeks is 15.3 inches (39.3 cm) long and weighs 3 pounds (1379 grams).
- The average fetus at 30 weeks is 15.8 inches (40.6 cm) long and weighs 3.4 pounds (1559 grams).
- Baby’s brain grows rapidly.
- The nervous system is developed enough to control some body functions.
- Your baby’s eyelids can open and close.
- The respiratory system, while immature, produces surfactant. This substance helps the air sacs fill with air.
Weeks 31 to 34 (Gestational Age 31 to 34 weeks or Embryonic Age 29 to 32 weeks)
- The average fetus at 31 weeks is 16.4 inches (41.9 cm) long and weighs 3.9 pounds (1751 grams).
- The average fetus at 32 weeks is 16.8 inches (43.2 cm) long and weighs 4.3 pounds (1953 grams).
- The average fetus at 33 weeks is 17.3 inches (44.4 cm) long and weighs 4.8 pounds (2162 grams).
- The average fetus at 34 weeks is 17.8 inches (45.6 cm) long and weighs 5.2 pounds (2377 grams).
- Your baby grows quickly and gains a lot of fat.
- Rhythmic breathing occurs, but baby’s lungs are not fully mature.
- Baby’s bones are fully developed, but are still soft.
- Your baby’s body begins storing iron, calcium, and phosphorus.
- If the fetus is a boy, his testicles are descending.
- The distal femoral epiphysis ossification center can usually be seen in 72 % of fetuses at 33 weeks 21)
Weeks 35 to 37 (Gestational Age 35 to 37 weeks or Embryonic Age 33 to 35 weeks)
- The average 35 week fetus is 18.2 inches (46.7 cm) long and weighs 5.7 pounds (2595 grams).
- The average 36 week fetus is 18.6 inches (47.8 cm) long and weighs 6.2 pounds (2813 grams).
- The average 37 week fetus is 19.1 inches ( 48.9 cm) long and weighs 6.7 pounds (3028 grams).
- Baby weighs about 5 1/2 pounds (2.5 kilograms).
- Your baby keeps gaining weight, but will probably not get much longer.
- The skin is not as wrinkled as fat forms under the skin.
- Baby has definite sleeping patterns.
- Your little one’s heart and blood vessels are complete.
- Muscles and bones are fully developed.
- The proximal tibial epiphysis ossification center may be seen in 35 % of fetuses at 35 weeks 22)
- The proximal humeral epiphysis ossification center may be seen at 38 weeks 23)
Week 38 to 40 (Gestational Age 38 to 40 weeks or Embryonic Age 36 to 38 weeks)
- The average 38 week fetus is 19.5 inches (49.9 cm) long and weighs 7.1 pounds (3236 grams).
- The average 39 week fetus is 19.8 inches (50.9 cm) long and weighs 7.6 pounds (3435 grams).
- The average 40 week fetus is 20.2 inches (52 cm) long and weighs 8 pounds (3619 grams).
- The average 41 week fetus is 20.5 inches (52.7 cm) long and weighs 8.3 pounds (3787 grams).
- The proximal humeral epiphysis ossification center may be seen at 38 weeks 24)
- Lanugo is gone except for on the upper arms and shoulders.
- Fingernails may extend beyond fingertips.
- Small breast buds are present on both sexes.
- Head hair is now coarse and thicker.
- In your 40th week of pregnancy, it has been 38 weeks since conception, and your baby could be born any day now.
Critical periods of fetal development
In every pregnancy, a woman starts out with a 3-5% chance of having a baby with a birth defect. This is called her background risk.
In pregnancy, each part of the baby’s body forms at a specific time. During these times, the body can be very sensitive to damage caused by medications, alcohol or other harmful exposures. Doctors call this specific time the “critical period of development” for that body part.
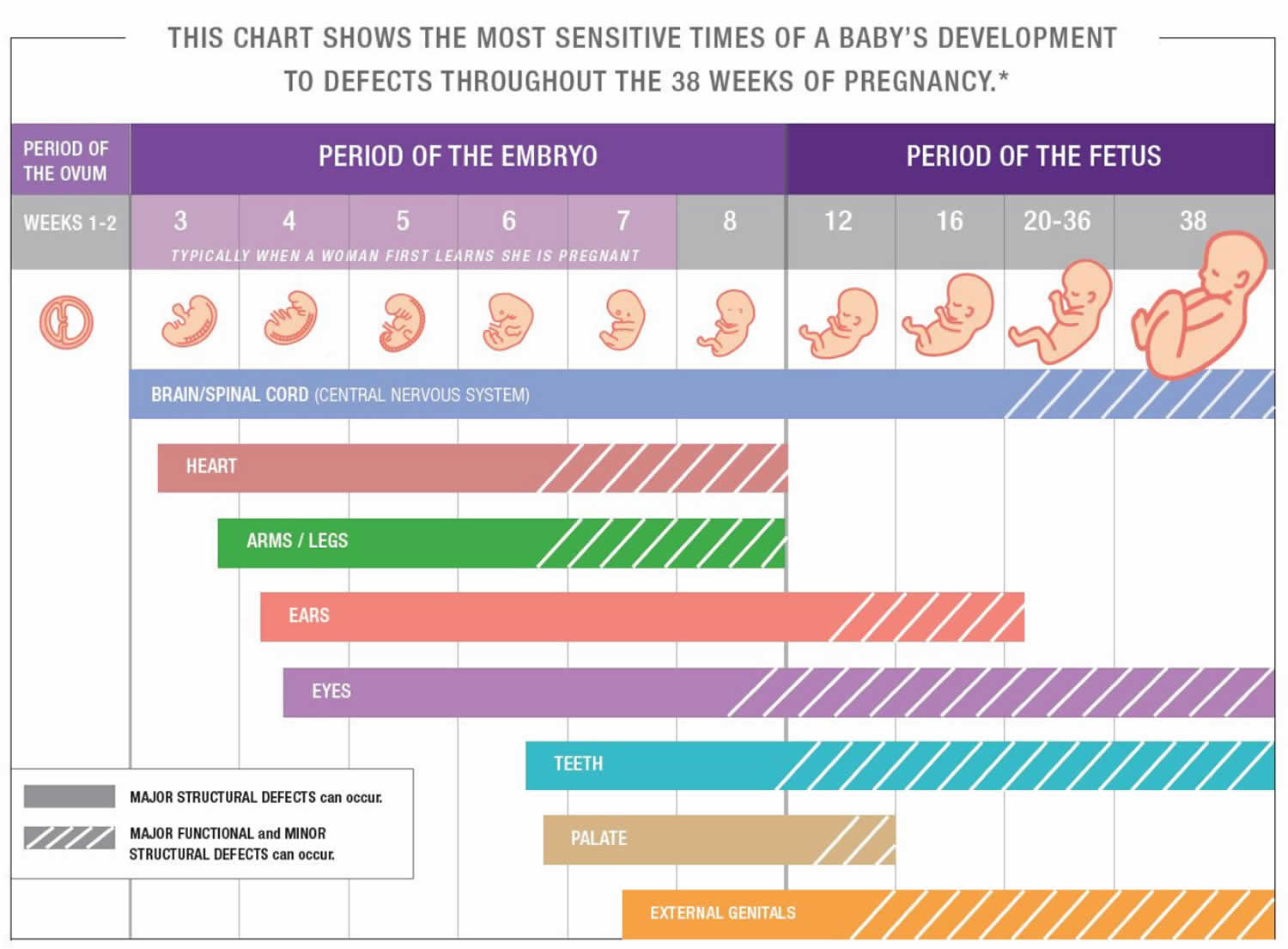
Figure 2. Critical periods of fetal development
Does the chance types of birth defects change throughout pregnancy?
Yes, the risk depends on what body part is developing at the time of exposure. Once a body part has formed, it is no longer at risk to develop major birth defects, but some exposures could still affect its growth and function.
The chart above (Figure 2) shows the critical periods of development for different parts of the body. The chart starts from the time of conception when the egg and sperm join. The weeks listed on the chart are the “embryonic age” or “fetal age” of a pregnancy. Note that this is different from a common way of dating a pregnancy called “gestational age.” Gestational age begins with the first day of a woman’s last menstrual period. This day is usually two weeks before a baby is conceived. This means that you can change gestational age to embryonic/fetal age by subtracting two weeks. For example, 12 gestational weeks (since the day of your last period) is the same as 10 fetal weeks (since the first day of conception).
The dark bars on the chart show when each part is most sensitive to harmful exposures and at risk for major birth defects. Birth defects are typically classified as “major” if they cause significant medical problems and need surgery or other treatment to repair. Heart defects, spina bifida, and clubfeet are examples of major birth defects.
The lightly shaded bars show periods when the body parts are still at risk to develop minor birth defects and functional defects. “Minor” birth defects by themselves do not cause significant medical problems and usually do not require treatment or surgery. Minor birth defects can also be variations of normal development. Wide-set eyes and large ears are examples of minor birth defects.
Both major and minor birth defects are physical or structural changes. However, “functional” defects change how a part of the body works without changing its physical structure. Intellectual disability and hearing loss are both examples of functional defects.
The chart also shows the location of the most common birth defects that can occur during each week. In general, major defects of the body and internal organs are more likely to occur between 3 to 12 embryo / fetal weeks. This is the same as 5 to 14 gestational weeks (weeks since the first day of your last period). This is also referred to as the first trimester. Minor defects and functional defects including twhose affecting the brain are also able to occur later in pregnancy.
What is the greatest risk from a harmful exposure during very early pregnancy?
Harmful exposures during very early pregnancy have the greatest risk of causing miscarriage. A fertilized egg divides and attaches to the inside of the uterus during the first two weeks of embryo development. Very harmful exposures during this period (first four weeks after the first day of your last period) may interfere with the attachment of the embryo to the uterus. Harmful exposures during this time can also damage all or most of the cells of the growing embryo. Problems with uterine attachment and severe cell damage can both result in a miscarriage. Sometimes this miscarriage is before a woman even realizes that she is pregnant.
Less severe exposures during this time may only damage a few of the embryo’s cells. The cells of the embryo have a greater ability to recover at this early stage than they do later on in pregnancy. If a woman does not have a miscarriage, we believe that the exposures during this time are not likely to cause a birth defect.
Doctors call the first four weeks of gestation the “all or none period”. “All” refers to high exposures damaging all of the embryo’s cells. This damage causes early miscarriage. “None” refers to exposures that are not high enough to have a significant effect on the pregnancy. Doctors can use the rule of the “all or none period” to determine the risk of many different types of exposures. However, there are some important exceptions to this rule.
What are the greatest risks from harmful exposures during the first trimester of pregnancy?
The first trimester of pregnancy is defined as up to the 14th week of pregnancy (13 weeks and 6 days) counting since the first day of your last menstrual period. Harmful exposures during the first trimester have the greatest risk of causing major birth defects. This is because many important developmental changes take place during this time. The major structures of the body form in the first trimester. These include the spine, head, arms and legs. The baby’s organs also begin to develop. Some examples of these organs are the heart, stomach and lungs. While the heart and stomach completely forms during the first trimester, the lungs continue to develop past the first trimester.
What are the greatest risks from harmful exposures during the second and third trimesters of pregnancy?
Harmful exposures during the second and third trimesters can cause growth problems and minor birth defects. Growth is an important part of the second and third trimester. The structures and organs that developed during the first trimester grow larger. Babies with growth problems may be much smaller or much larger than average. This size difference can put babies at risk for certain health problems.
Harmful exposures during the second and third trimesters can also cause functional defects like learning problems. The brain is part of the central nervous system and it develops during the entire pregnancy. Major, structural brain development lasts until about 16 fetal weeks (18 gestational weeks). However, the brain continues to develop for the rest of the pregnancy, after birth and through young adulthood.
While usually less well studied, some exposures in the second or third trimester might cause other pregnancy complications, such as premature delivery or low levels of amniotic fluid (the fluid that surrounds the developing baby in the uterus).
Finally, the use of certain medications and drugs at the end of pregnancy can cause withdrawal in some newborns. You should always tell your health care provider about all of the medications, supplements and/or drugs that you take.
Does this mean that an exposure might be harmful at certain times during pregnancy but not at other times?
Yes. Imagine your doctor gives you a new medication to take during your third trimester. We will call this “Medication A.” You read that Medication A increases the chance for heart defects. This means that babies may have a higher chance for major heart defects if their mothers’ take this medication during the heart’s critical period of development. We know that the heart’s critical period of development is from 3 to 6 embryonic weeks (5 to 8 gestational weeks). This means that using this medication in the third trimester cannot cause a major heart defect. Always talk to your health care provider before starting or stopping any medication.
References [ + ]