Contents
Linear scleroderma
Linear scleroderma represents a unique form of localized scleroderma that primarily affects children, with 67% of patients diagnosed before 18 years of age 1). Linear scleroderma manifests as thickened and hardened skin bands, which are most often on the face or extremities. Linear scleroderma is the most common form of scleroderma in children. Women are affected about four times more than men.
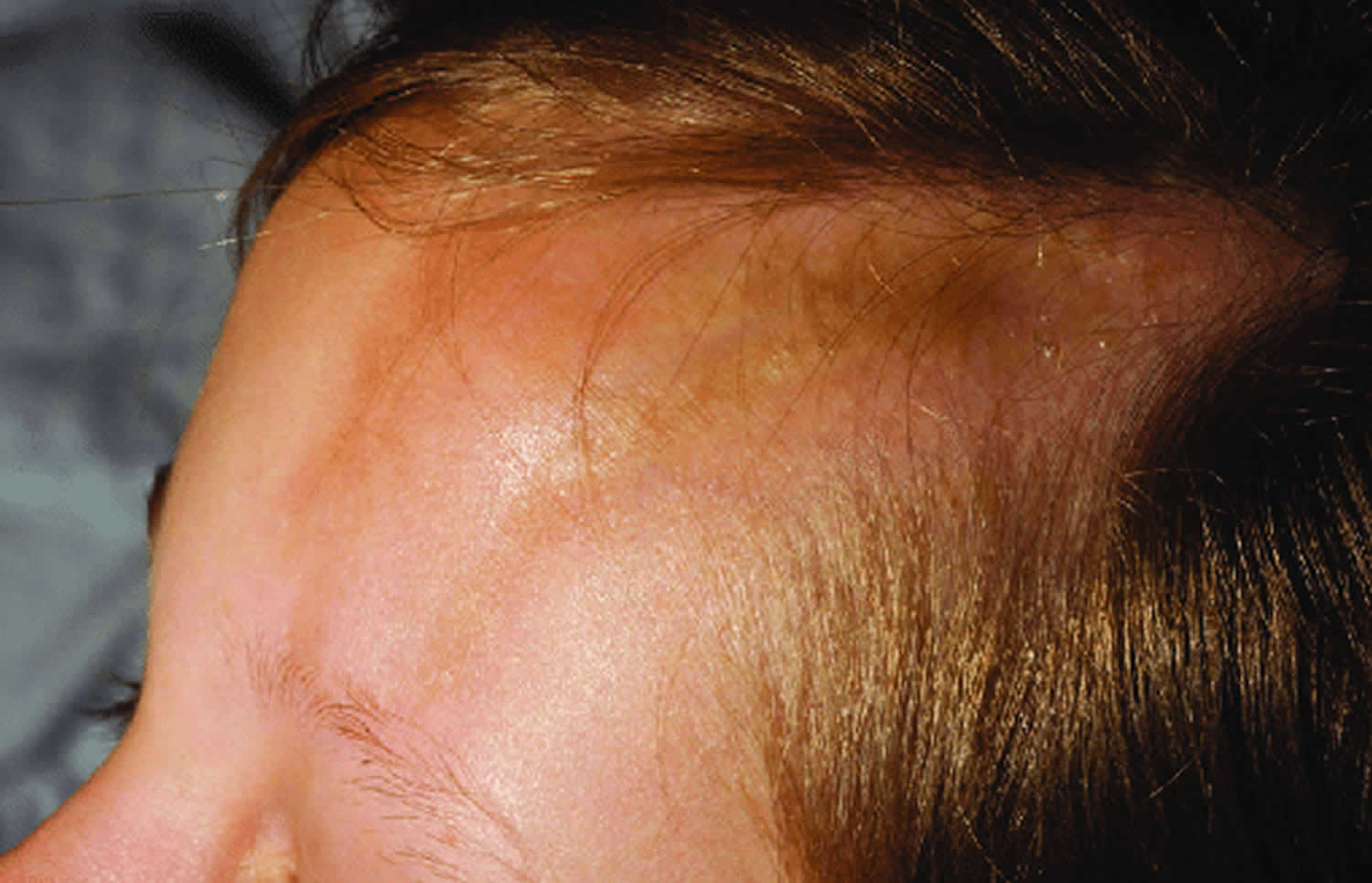
When linear scleroderma occurs on the scalp or face, it is referred to as linear scleroderma “en coup de sabre” (a French expression meaning “cut from a sword”), given the resemblance of the skin lesions to the stroke of a sabre. The sclerotic band is generally located on the forehead but can extend to the scalp (causing scarring alopecia), and to the nose as well as the upper lip. The skin is hypo or hyperpigmented, atrophic and adheres to the underlying bone. This form of scleroderma can sometimes be associated with ipsilateral hemiatrophy of the face and is therefore hardly individualizable from Parry-Romberg syndrome.
Linear scleroderma of the limbs is called “monomelic” and often begins in childhood. Sclero-atrophic bands appear gradually and then extend to the muscles and tendons; this may lead to an extreme aspect of pansclerotic morphea with joint and bone deformities sometimes associated with a stop or growth retardation of the limb.
Localized scleroderma typically only affects the skin, although in some cases the underlying muscle and tissue may be involved (subcutaneous morphea). Localized scleroderma is not a fatal disease, but quality of life is often adversely affected because of changes in the appearance of the skin, the occurrence of joint contractures that affect movement, and, rarely, serious deformities of the face and extremities.
Linear scleroderma treatments may include medications, which may include nonsteroidal anti-inflammatories (NSAIDs) or corticosteroids, penicillamine and/or immunosuppressive drugs and therapies to protect the skin, physiotherapy and exercise, and/or surgery as indicated.
Figure 1. Linear morphea scleroderma
Figure 2. Localized scleroderma face (en coup de sabre)
Figure 3. Linear scleroderma forehead (en coup de sabre)
What is scleroderma?
Scleroderma means “hard skin”, which is a rare autoimmune connective tissue disorder of unknown cause in which an overproduction of abnormal collagen causes normal tissues to be replaced with thick, dense scar tissue that can affect underlying bones and muscles if left untreated 2).
- Although any age can be affected, the peak incidence is 20-40 years of age, and 15% of cases occur before the age of 10 years
- The female to male ratio is 3:1
- Scleroderma is less common in black people
- The onset of scleroderma is generally insidious, and although asymptomatic, affected skin often ceases to sweat
- The severity and outcome of scleroderma are variable 3).
There are two forms of scleroderma:
- Localized scleroderma primarily affects the skin and may have an impact on the muscles and bones. Localized scleroderma is the most common form found in children.
- Systemic sclerosis a chronic, degenerative disease rarely seen in children. In systemic scleroderma, there is an involvement of the internal organs, such as the digestive tract, heart, lungs, and kidneys, among others.
It is important to understand that localized scleroderma is different from the form of scleroderma which affects internal organs, called systemic sclerosis, often incorrectly stated, as systemic scleroderma.
Scleroderma has been associated with:
- Drugs eg bleomycin, carbidopa, penicillamine
- Chemicals eg polyvinyl chloride, solvents used in dry cleaning, pesticides
- Graft-versus-host disease following bone marrow transplantation
What is localized scleroderma?
Localized scleroderma is a type of scleroderma that typically only affects the skin, although in some cases the underlying muscle and tissue may be involved (subcutaneous morphea).
Localized scleroderma is characterized by inflammation and thickening of the skin from excessive collagen deposition. Collagen is a protein normally present in our skin. It provides structural support. However, when too much collagen is made, the skin becomes stiff and hard. Some patients with localized scleroderma, an estimated 10 to 20 percent, develop joint pain.
Localized scleroderma is not infectious and cannot be spread by touch or contact with the patient. Localized scleroderma is not hereditary; however, in rare instances similar problems may be present in relatives. Localized scleroderma is thought to be an autoimmune disease but, other than the presence of blood autoantibodies (confusingly similar to those with some internal diseases), patients have no other known or profound defect in the immune system.
Localized scleroderma types
Names and terminology are widely varied and cause a great deal of confusion in localized scleroderma. Patients are often told they have “scleroderma,” which may frighten them. A newly diagnosed patient may think they have systemic sclerosis and will develop internal organ involvement. This is not true.
There are four main types of localized scleroderma. Each type is characterized by the shape and amount of affected skin.
The four types are:
- Morphea – This is the most common type of localized scleroderma. It presents as one or a few (3-4) patches of skin thickening with different degrees of pigment changes. Some areas are dark while others are lighter than the surrounding normal skin. Often, the skin lesion is not quite hard to the touch. It is generally painless, but pruritus (itching) may be present. A violet-colored border may be seen when the lesions are still very active and extending. Sometimes, doctors will classify morphea further into other sub-types, according to the shape or depth of the lesions. For example, “guttate” morphea refers to “drop-like” shaped areas of skin involvement, whereas “subcutaneous” morphea indicates a substantial involvement of deeper tissues with relative sparing of the overlying skin. The subcutaneous type may extend deep into muscle tissues in very rare instances, but this does not indicate internal organ involvement.
- Generalized morphea – Generalized morphea involves larger skin patches than morphea, often including more of the body surface. Rarely, most of the body may be involved. Some patients with generalized morphea also have a band of thickening on an arm or leg as seen in linear scleroderma, another type of localized scleroderma. Moreover, individual patches of morphea are common in linear scleroderma. Therefore, although one type of localized scleroderma usually predominates, patients may have a combination of different types of skin involvement. Patients with generalized morphea, because of the extensive surface area involved, may encounter considerable cosmetic disability resulting from the appearance of the problem (many dark and light areas of skin). Also, because of skin thickening over the joints, patients may have limited joint function.
- Linear scleroderma as the name implies, shows a band or line of skin thickening. It may extend deep into the skin and even involve the underlying muscle. The band of skin thickening is more common on the legs and arms and, when crossing the joints, may prevent proper joint motion. On rare occasions linear scleroderma can be a serious problem in children, especially when it extends deep into the skin. Sometimes, for reasons we do not yet understand, linear scleroderma delays growth of the underlying bones in children who are still in an active growth phase.
- En coup de sabre – An unusual form of linear scleroderma on the face or scalp may appear as a white line referred to as “en coup de sabre.” This is a French term meaning “cut from a sword,” because of the way it looks. Some people think it may be completely different from linear scleroderma. En coup de sabre can be very destructive, as when it results in atrophy (loss of tissue) of the face in children; this process may involve the tongue and mouth. Rarely, the condition is associated with abnormalities in the growth of facial bones, which can potentially lead to considerable deformities. There may be some overlap between en coup de sabre and a rare atrophy in the face, known as Parry-Romberg syndrome.
Does localized scleroderma go away?
As a general rule, localized scleroderma is a self-limiting problem, at least in terms of activity of the process; the color changes are likely to remain. Sometimes, new lesions may appear for a few years, but eventually, the process of developing new areas of involvement will subside. The one possible exception to this statement is en coup de sabre, which may run an unpredictable course and become active again, even many years or decades after it first appeared.
Linear scleroderma causes
Scleroderma occurs as a result of the overproduction of collagen by the body. Why exactly this occurs, however, is unknown. There is some evidence that genetic and environmental factors play a role in the genesis of scleroderma. Silica and certain organic solvents are recognized as risk factors of occurrence of systemic scleroderma. The result is an activation of the immune system, causing blood vessel damage and injury to tissues that result in scar tissue formation and the accumulation of excess collagen.
Genetic factors play at least a limited role. According to three US cohorts, the prevalence of the disease was 13 times higher in first-degree relatives of scleroderma patients than in the general population. OX40L gene polymorphism correlates with systemic scleroderma. IRF5 gene was found to correlate with systemic scleroderma as well as with the occurrence of interstitial lung disease during scleroderma 4).
Scleroderma has been associated with:
- Drugs eg bleomycin, carbidopa, penicillamine
- Chemicals eg polyvinyl chloride, solvents used in dry cleaning, pesticides
- Graft-versus-host disease following bone marrow transplantation
Linear scleroderma symptoms
Linear scleroderma is a progressive loss of subcutaneous fat with pigment changes in the skin. Linear scleroderma is a type of localized scleroderma in which the area of skin affected appears in a band. It typically first appears in young children on one side of the body. A shiny, thickened streak of tough darker (or lighter) looking skin that may involve a leg or arm and may spread along a line to feet or hand (sometimes on head, face, scalp, and forehead). This often affects deeper layers of skin, spreads over joints and may limit the movement of the joint, or if extensive may not allow the limb to grow normally.
Symptoms of localized scleroderma may include:
- Shiny, thickened patches of skin
- Discolored (lighter or darker) skin
- Joint tightness
Up to 30% of patients with more severe types of linear scleroderma or generalized scleroderma can have extracutaneous non-specific inflammatory symptoms. These include:
- Fatigue, lethargy
- Non-specific joint pain and/or inflammation (arthralgia, arthritis)
- Muscle pain
- Reflux/heartburn
- Raynaud phenomenon (cold hands with red/white/blue colour changes)
- Eye dryness, irritation or blurred vision due to ocular involvement (most commonly episcleritis, anterior uveitis, keratitis) – related or unrelated to the site of morphoea
These extracutaneous manifestations imply that localized scleroderma is a systemic inflammatory condition. In contrast, systemic sclerosis results in direct damage and fibrosis of the lungs, heart, kidneys and/or gastrointestinal tract — which do not occur in localized scleroderma.
Scleroderma can result in cosmetic problems, scarring, growth abnormalities and limited motion if joints are affected. Symptoms may resemble other medical conditions, so always consult your child’s physician to confirm her diagnosis before pursuing treatment.
Linear scleroderma complications
Linear scleroderma of the limbs may cause functional disabilities, particularly if the disease affects the underlying bone. Linear scleroderma “en coup de sabre” may induce esthetic and/or functional concerns.
Linear scleroderma diagnosis
Doctors who are familiar with scleroderma, or who are experts at examining the skin, can arrive at the diagnosis without much difficulty after a careful examination. In some cases, further tests may be needed to confirm the diagnosis. These tests may include taking a small sample of the skin (a biopsy) and some blood samples. It’s important that the entire skin surface be examined, so that a complete record is made of what is present at first (baseline record). Photographic documentation is also valuable.
Diagnosis of linear scleroderma is usually based on the changes in the skin and internal organs. Because linear scleroderma is often associated with a positive antinuclear antibody, an antibody test may help distinguish the type of scleroderma present.
In addition to a complete medical history and physical examination, your child may undergo additional diagnostic testing, including an echocardiogram, electrocardiogram (EKG or ECG) or X-ray. An EKG can detect abnormal heart rhythms which may be caused by changes in the heart muscle tissue due to scleroderma. X-rays may detect changes in bone and soft tissues, the gastrointestinal tract, and the lungs caused by scleroderma
Linear scleroderma is sometimes confused with Parry-Romberg syndrome because both conditions are characterized by the same progressive loss of subcutaneous fat. Like Parry-Romberg disease, the onset of linear scleroderma occurs is in childhood and may involve the facial region. Unlike Parry-Romberg disease, there is no optic nerve dysfunction, burnout phase and generally no muscle or bone atrophy.
Medical professionals who are experienced in diagnosing and treating children with linear scleroderma and Parry-Romberg syndrome will be able to distinguish between the two and provide an accurate diagnosis.
Linear scleroderma treatment
Treatment for scleroderma depends on your child’s overall health and the severity of the condition. Treatment may include:
- Medication — Your child’s medical team may recommend medications such as nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids to relieve pain; penicillamine to slow the thickening process and delay damage to internal organs; or immunosuppressive medications. Linear scleroderma of the face or limbs generally requires the combination of systemic corticosteroids and methotrexate to avoid functional and/or esthetic disabilities 5).
- Skin protection — Sunblock or protective padding can be used to protect the affected area.
- Physical therapy — Physical therapy and exercise can be used to maintain muscle strength.
- Surgery — Surgical treatment may involve fat transferred by injection or excision of isolated patches of abnormal tissue. In the fat transfer technique, fat is aspirated from elsewhere in the body, cleaned, and reinjected into the tissue under the skin to add volume, contour and shape. This is a minimally invasive procedure and usually can be done on an outpatient basis.
If large areas of discolored, irregular skin are involved, the preferred treatment option may be direct excision of the abnormal tissue with closure of the adjacent normal skin. While this procedure may leave a scar, the scar is typically less noticeable than the existing deformity. This procedure is also typically done on an outpatient basis, and your child can return home the same day.
In severe atrophy, large amounts of tissue may be transferred to the affected area using microsurgical techniques. This transferred tissue often comes from the trunk or legs. The tissue may be placed deeply to add volume, closer to the surface of the skin to replace damaged skin, or both.
Linear scleroderma prognosis
In localized scleroderma, the hardening of the skin generally ceases in the two years after the onset of the disease, and the lesions do not extend to other parts from the body 6). However, the disease can sometimes last several years, and some plaques may become more marked even after the end of inflammation.
Linear scleroderma has the potential to cause serious complications. The linear areas of the skin thickening may extend to the underlying tissue and muscle in children, which may impair growth in the affected leg or arm.
Extensive lesions of linear scleroderma, when cross joint lines, can impair motion of that particular joint. Unless continued efforts are made to maintain a full range of motion to the affected joint with physical therapy, this complication may be permanent and result in the affected area (for example, the elbow, arm, finger, etc.) being in a fixed position (contracture). Many patients with linear scleroderma, especially if older at the age of onset of the disease, will have only minor skin changes and minimal skin thickening. Linear scleroderma remains active for two to five years, but can last longer in some cases. Sometimes patients develop recurrences after a period of what was thought to be inactive disease. This “recurrence” is more frequent in patients with “en coup de sabre.”
En coup de sabre is potentially the most disfiguring form of localized scleroderma, because it affects the face and scalp. It can be mild, with only slight atrophy of the skin. However, depending on its locations on the face, it can lead to considerable problems, especially in children. It is possible that it is an entity by itself, and not truly a type of linear scleroderma. If located on the scalp, it can cause varied degrees of hair loss. When involving the face, it can lead to indentations or depressions of the skin surface, especially on the forehead. The process can extend to the underlying bone. Recurrences can occur, even when it seems the disease has gone into remission.
References [ + ]