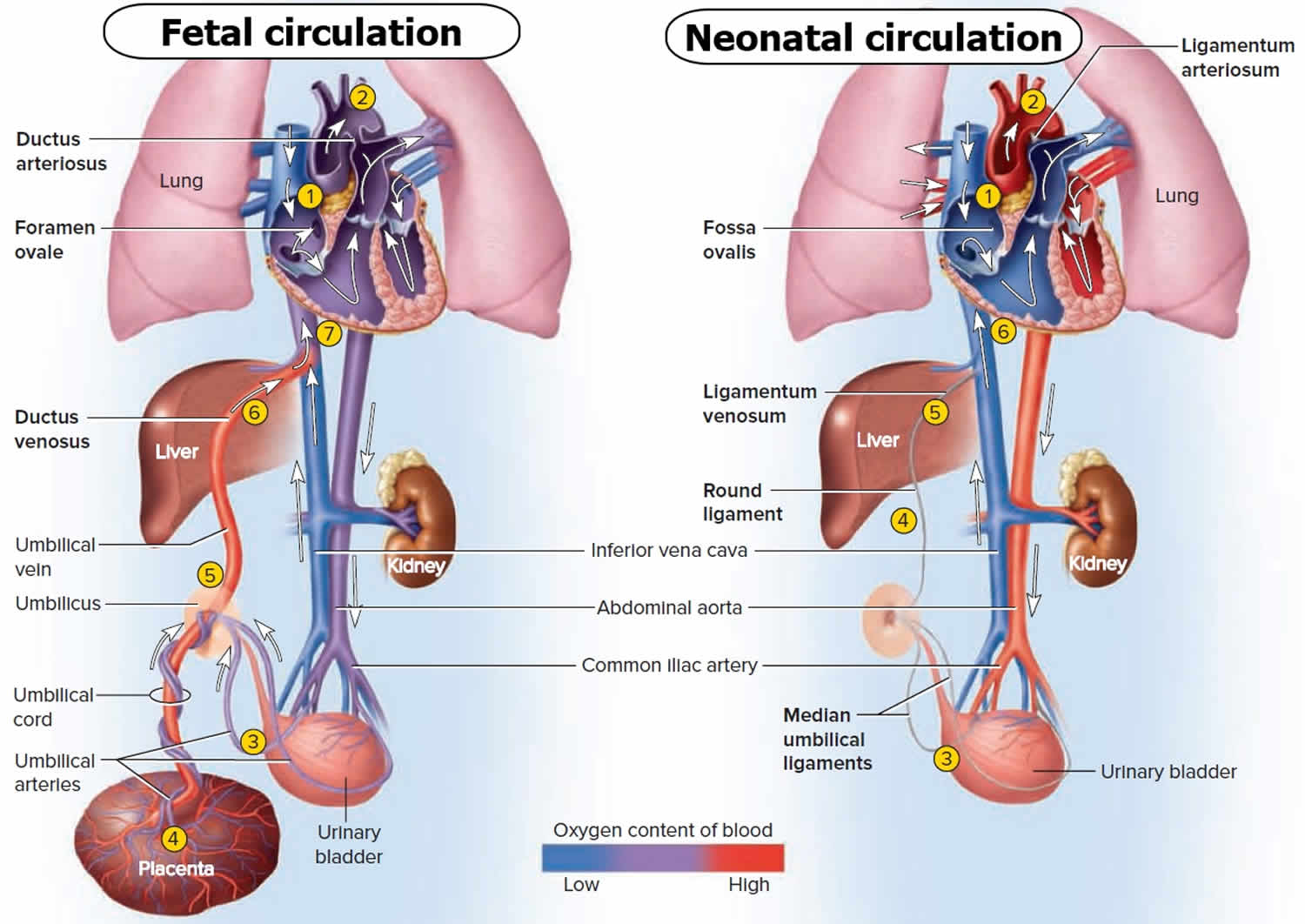
Fetal circulation
The circulatory system of a fetus called the fetal circulation, exists only in the fetus and contains special structures that allow the developing fetus to exchange materials with its mother (Figure 1). Fetal circulation differs from the neonatal (after birth) circulation because the lungs, kidneys, and gastrointestinal organs do not begin to function until birth. The fetus obtains oxygen (O2) and nutrients from the maternal blood and eliminates carbon dioxide (CO2) and other wastes into it.
The exchange of materials between fetal and maternal circulations occurs through the placenta, which forms inside the mother’s uterus and attaches to the umbilicus (navel) of the fetus by the umbilical cord. The placenta communicates with the mother’s cardiovascular system through many small blood vessels that emerge from the uterine wall. The umbilical cord contains blood vessels that branch into capillaries in the placenta. Wastes from the fetal blood diffuse out of the capillaries, into spaces containing maternal blood (intervillous spaces) in the placenta, and finally into
the mother’s uterine veins. Nutrients travel the opposite route, from the maternal blood vessels to the intervillous spaces to the fetal capillaries. Normally, there is no direct mixing of maternal and fetal blood because all exchanges occur by diffusion through capillary walls.
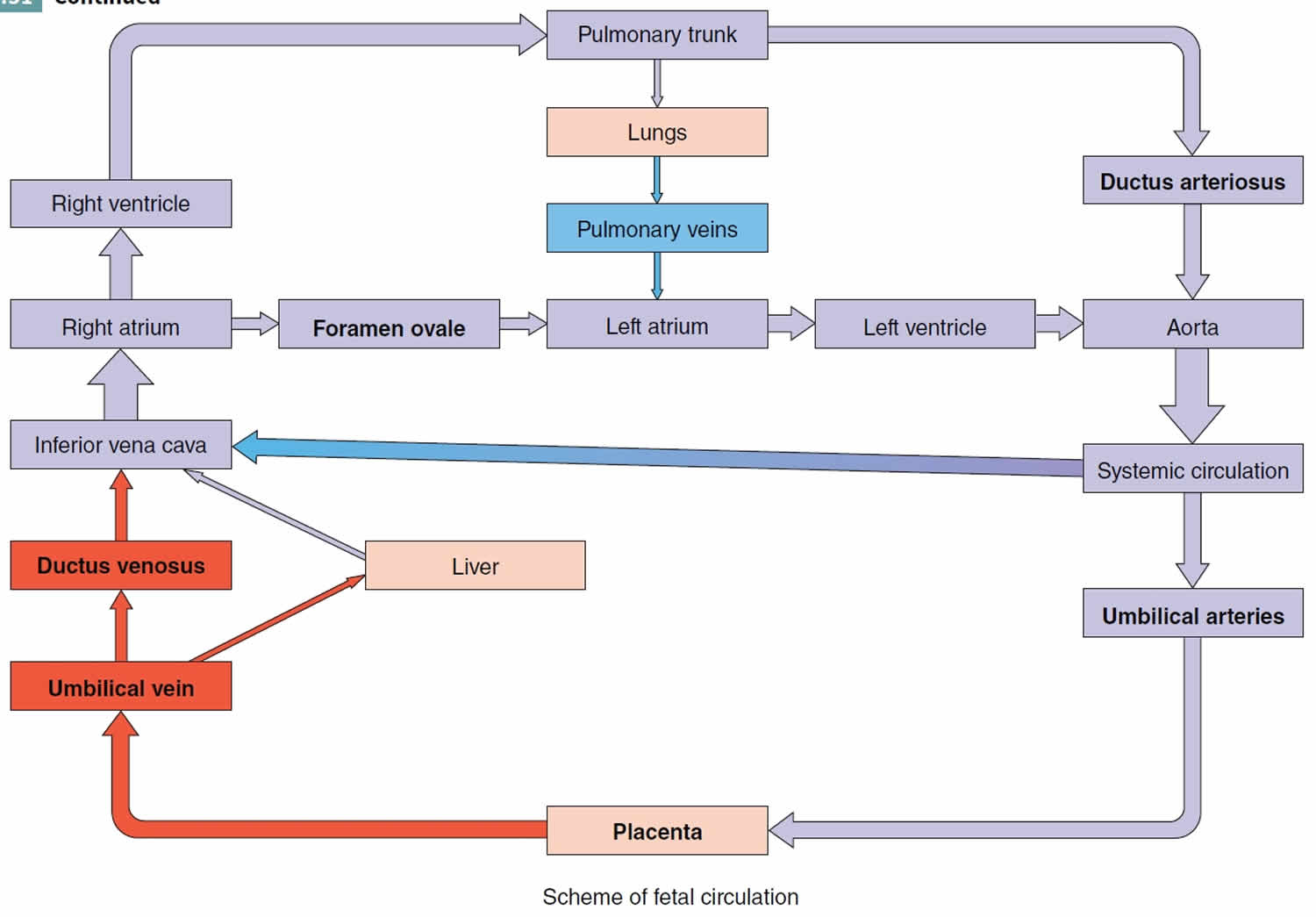
Blood passes from the fetus to the placenta via two umbilical arteries in the umbilical cord (Figure 1). These branches of the internal iliac (hypogastric) arteries are within the umbilical cord. At the placenta, fetal blood picks up O2 and nutrients and eliminates CO2 and wastes. The oxygenated blood returns from the placenta via a single umbilical vein in the umbilical cord. This vein ascends to the liver of the fetus, where it divides into two branches. Some blood flows through the branch that joins the hepatic portal vein and enters the liver, but most of the blood flows into the second branch, the ductus venosus, which drains into the inferior vena cava (IVC).
The unique aspects of fetal circulation are the umbilical–placental circuit and the presence of three circulatory shortcuts called shunts. The internal iliac arteries give rise to the umbilical arteries, which pass on either side of the bladder into the umbilical cord. The blood in these arteries is low in oxygen (O2) and high in carbon dioxide (CO2) and other fetal wastes; thus, they are depicted in blue in figure 1. The arterial blood discharges its wastes in the placenta, loads oxygen and nutrients, and returns to the fetus by way of a single umbilical vein, which leads toward the liver. The umbilical vein is depicted in red because of its well-oxygenated blood. Some of this venous blood filters through the liver to nourish it. However, the immature liver is not capable of performing many of its postpartum functions, so it doesn’t require a great deal of perfusion before birth. Most of the venous blood therefore bypasses it by way of a shunt called the ductus venosus, which leads directly to the inferior vena cava (IVC).
Deoxygenated blood returning from lower body regions of the fetus mingles with oxygenated blood from the ductus venosus in the inferior vena cava (IVC). This mixed blood then enters the right atrium of the heart. Deoxygenated blood returning from upper body regions of the fetus enters the superior vena cava (SVC) and also passes into the right atrium of the heart.
In the inferior vena cava (IVC), placental blood mixes with venous blood from the fetus’s body and flows to the right atrium of the heart. Most of the fetal blood does not pass from the right ventricle to the lungs, as it does in postnatal circulation, because an opening called the foramen ovale exists in the septum between the right and left atria. Most of the blood that enters the right
atrium passes through the foramen ovale into the left atrium and joins the systemic circulation. The blood that does pass into the right ventricle is pumped into the pulmonary trunk, but little of this blood reaches the nonfunctioning fetal lungs. Instead, most is sent through the ductus arteriosus, a vessel that connects the pulmonary trunk with the aorta. The blood in the aorta is carried to all fetal tissues through the systemic circulation. When the common iliac arteries branch into the external and internal iliacs, part of the blood flows into the internal iliacs, into the umbilical arteries, and back to the placenta for another exchange of materials.
This circulatory pattern changes dramatically at birth, when the neonate is cut off from the placenta and the lungs expand with air (see neonatal circulation). After birth, when pulmonary (lung), renal (kidney), and digestive functions begin, the following vascular changes occur (Figure 1 – Neonatal circulation):
Neonatal circulation
- When the umbilical cord is tied off, blood no longer flows through the umbilical arteries, they fill with connective tissue, and the distal portions of the umbilical arteries become fibrous cords called the medial umbilical ligaments. Although the arteries are closed functionally only a few minutes after birth, complete obliteration of the lumens may take 2 to 3 months.
- The umbilical vein collapses but remains as the ligamentum teres (round ligament), a structure that attaches the umbilicus to the liver.
- The ductus venosus collapses but remains as the ligamentum venosum, a fibrous cord on the inferior surface of the liver.
- The placenta is expelled as the after birth.
- The foramen ovale normally closes shortly aft er birth to become the fossa ovalis, a depression in the interatrial septum. When an infant takes its first breath, the lungs expand and blood flow to the lungs increases. Blood returning from the lungs to the heart increases pressure in the left atrium. This closes the foramen ovale by pushing the valve that guards it against the interatrial septum. Permanent closure occurs in about a year.
- The ductus arteriosus closes by vasoconstriction almost immediately aft er birth and becomes the ligamentum arteriosum. Complete anatomical obliteration of the lumen takes 1 to 3 months.
Figure 1. Fetal blood circulation (fetal and neonatal circulation)
Footnotes: Boldface terms in part (a) indicate the three shunts in the fetal circulation, which allow most blood to bypass the liver and lungs. Boldface terms in part (b) indicate the postpartum vestiges of fetal structures.
(a) Fetal circulation
- 1) Blood bypasses the lungs by flowing directly from the right atrium through the foramen ovale into the left atrium.
- 2) Blood also bypasses the lungs by flowing from the pulmonary trunk through the ductus arteriosus into the aorta.
- 3) Oxygen-poor, waste-laden blood flows through two umbilical arteries to the placenta.
- 4) The placenta disposes of CO2 and other wastes and reoxygenates the blood.
- 5) Oxygenated blood returns to the fetus through the umbilical vein.
- 6) Placental blood bypasses the liver by flowing through the ductus venosus into the inferior vena cava (IVC).
- 7) Placental blood from the umbilical vein mixes with fetal blood from the inferior vena cava (IVC) and returns to the heart.
(b) Neonatal circulation
- 1) Foramen ovale closes and becomes fossa ovalis.
- 2) Ductus arteriosus constricts and becomes ligamentum arteriosum.
- 3) Umbilical arteries degenerate and become median umbilical ligaments.
- 4) Umbilical vein constricts and becomes round ligament of liver.
- 5) Ductus venosus degenerates and becomes ligamentum venosum of liver.
- 6) Blood returning to the heart is now oxygen-poor, systemic blood only.
Figure 2. Scheme of fetal blood circulation