Contents
Acne in children
Acne also known as pimples or zits is a totally normal part of growing up. Kids get acne because of changes that occur during puberty, the time when kids’ bodies begin the many changes that turn them into adults. Acne occurs on the face, neck, chest, back, shoulders, and even the upper arms. The most common type of acne is acne vulgaris.
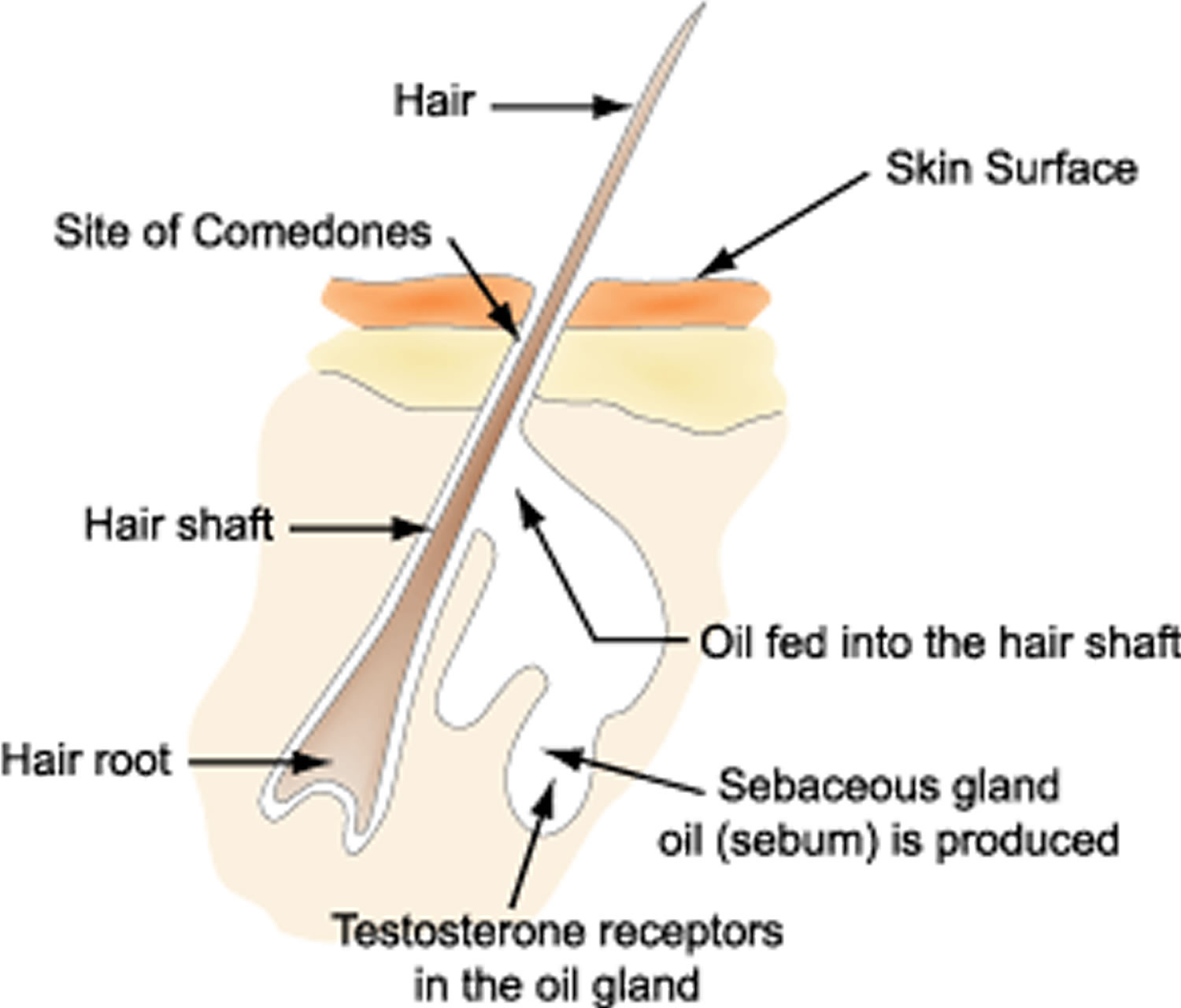
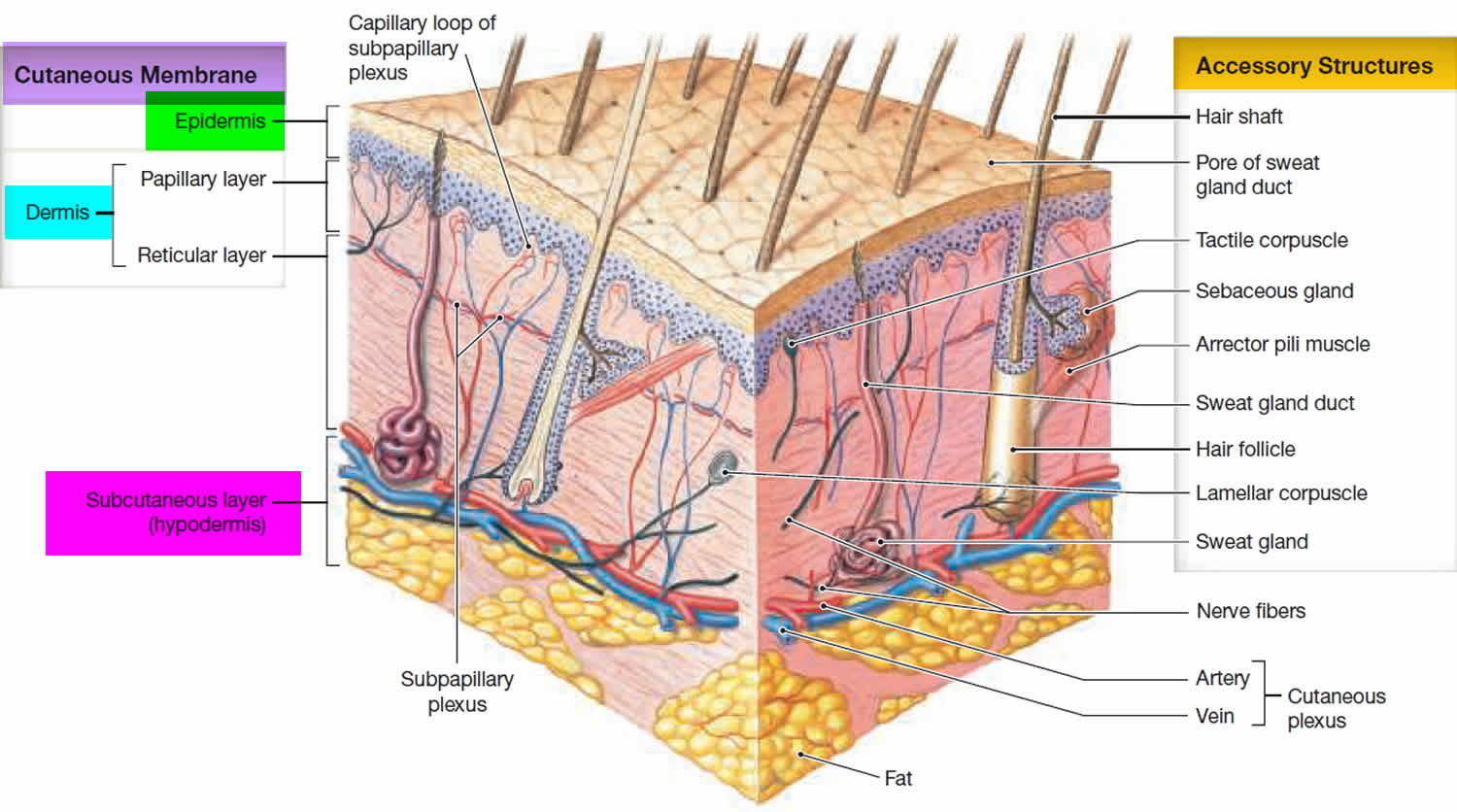
Acne is a disorder of the hair follicles and sebaceous glands. Hair follicles are the areas around the base or root of each hair. Sebaceous glands are the tiny glands that release oil (sebum) into the hair follicles. The sebum moistens the skin and hair. The sebum and hair get to the skin surface through tiny holes called pores.
Acne is very common. Most children and young adults between ages 11 and 30 will have acne at some point. Acne most often begins in puberty. But it can happen at any age. There are different types of acne that affect newborns, infants, younger children, and adults.
Acne may occur when the pores gets clogged with dead skin cells and oil. Bacteria that are normally on the skin may also get into the clogged pore. Acne comes in several types. One type is a comedone. This is a plug of sebum in the hair follicle. They are either closed whiteheads, or open blackheads. These are not inflamed or infected.
Inflamed acne causes red, painful bumps or sores. The sores may be infected with bacteria. This type of acne includes:
- Pustule: Bacteria cause the hair follicle to be inflamed. Pustules are closer to the skin surface.
- Papule: The wall of the hair follicle gets irritated. Papules are deeper in the skin.
- Nodule: These are larger, deeper, and more solid.
- Cyst: This is a nodule with pus.
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is. The goal of acne treatment is to improve the skins appearance and to lessen the chance of scarring. Treatment for acne will include gentle, regular skin care. Your child’s healthcare provider may advise:
- Non-prescription cleansers and creams, lotions, gels, or other products
- Prescriptions that are put on the skin (topical) or taken by mouth (oral)
- Other therapies or procedures, such as laser therapy, light therapy, or chemical peels
- Draining of a cyst, or injecting it with medicine
Topical medicines are often prescribed to treat acne. These can be in the form of a cream, gel, lotion, or liquid. These may include:
- Benzoyl peroxide: This kills bacteria.
- Antibiotics: These help stop or slow down the growth of bacteria. They also reduce inflammation.
- Tretinoin: This stops new comedones from forming. It also encourages new skin cell growth and unplugs pimples.
- Adapalene: This helps stop new comedones from forming.
Medicines to take by mouth may be prescribed, such as:
- Antibiotic medicines: These may include tetracycline, doxycycline, or erythromycin. They are used to treat moderate to severe acne.
- Isotretinoin: This may be prescribed for severe acne that can’t be treated by other methods. It helps to prevent new acne and scarring.
Acne in children key points
- Acne is a disorder of the hair follicles and sebaceous glands.
- Acne may happen when the pores gets clogged with dead skin cells and oil. Bacteria that are normally on the skin may also get into the clogged pore.
- Most teens and young adults between 11 and 30 years old will have acne at some point.
- Both over-the-counter and prescription medicines are available to treat acne.
- Acne can have an emotional effect. This can lead to depression, anxiety, and even suicidal thoughts.
- Scarring can result from severe or long-term acne.
Figure 1. Acne formation
Figure 2. Skin structure
See your child’s healthcare provider if:
- Your child is upset by his or her acne
- The acne is getting worse
- Over-the-counter treatments are not working
Why is acne often most severe during teenage years?
The precise reasons that acne is most severe during the teenage years are being studied. There are several theories.
There are higher levels of sex hormones after puberty than in younger children.
- Sex hormones are converted in the skin to dihydrotestosterone (DHT), which stimulates sebaceous (oil) glands at the base of hair follicles to enlarge.
- The sebaceous glands produce sebum. Changes in sebum composition may lead to acne lesions.
- The activated sebaceous gland cells (sebocytes) also produce pro-inflammatory factors, including lipid peroxides, cytokines, peptidases and neuropeptides.
- Hair follicles are tiny canals that open into skin pores (tiny holes) on the skin surface. The follicles normally carry sebum and keratin (scale) from dead skin cells to the surface. Inflammation and debris leads to blockage of the skin pores — forming comedones.
- The wall of the follicle may then rupture, increasing an inflammatory response.
- Bacteria within the hair follicle may enhance inflammatory lesions.
While acne is most common in adolescents, acne can affect people of all ages and all races. It usually becomes less of a problem after the age of 25 years, although about 15% of women and 5% of men continue to have acne as adults. It may also start in adult life.
Why is acne worse in some people?
Some people have particularly severe acne. This may be because of:
- Genetic factors (family members have bad acne)
- Hormonal factors (higher levels of male/androgenic hormones) due to:
- Polycystic ovaries (common). Hyperinsulinaemia and insulin resistance are characteristically found in women with polycystic ovarian syndrome, who are prone to acne among other problems
- Psychological stress and depression
- Excessive corticosteroids eg Cushing disease (rare)
- Enzyme deficiency eg sterol hydroxylase deficiency (very rare)
- Environmental factors such as:
- High humidity causing swelling of the skin
- Cosmetics especially certain moisturisers, foundation and pomades. Watch out for products that contain lanolin, petrolatum, vegetable oils, butyl stearate, lauryl alcohol and oleic acid.
- Pressure from headbands and chin straps (eg “fiddler’s neck”, a condition seen in violin or viola players, where continual pressure from the violin against the neck causes skin irritation)
- Excessive dairy products, meat protein and sugars in the diet. Diets low in zinc or high in iodine can worsen pustular acne.
- Certain medications may provoke acne.
- Much of the individual variation in acne severity is due to variation in the innate immune system and the production of inflammatory mediators such as cytokines, defensins, peptidases, sebum lipids, and neuropeptides. Evidence has emerged that inflammation leads to distension and occlusion of the hair follicle, which then ruptures.
Do certain foods cause acne?
Some studies suggest there is a link between the food we eat and acne. It is very difficult to study the role of diet and acne.
Acne is reported to be less common in people that have a diet with lower glycaemic index, eg, natives from Kitava and Papua New Guinea, the Ache people of Paraguay, Inuits and rural residents of Kenya, Zambia and Bantu. These people tend to become sexually mature at a later age than in the cities where higher glycaemic index foods are consumed. Early puberty is associated with earlier onset and more severe acne that tends to peak at the time of full maturity (age 16 to 18).
Several studies, criticised for their quality, have shown benefits in acne from a low-glycaemic, low-protein, low-fat and low-dairy diet. The reasons for these benefits are thought to relate to the effects of these foods on insulin and insulin-like growth factor-1 (IGF-1).
Insulin induces male hormones (androgens), glucocorticoids and growth factors. These provoke keratinisation (scaling) of the hair follicle and sebum production. An increase in sebum production and keratinisation is a factor in the appearance of acne.
On the other hand, a large prevalence study of acne in military recruits showed a lower prevalence in severely obese adolescents than in those of normal weight.
Foods that increase insulin production
Foods that increase insulin levels have a high glycemic index. The glycemic index is a measurement of how carbohydrates have an effect on your blood sugar levels. When you eat foods with a high glycemic index, such as white bread and baked goods, your blood sugar level rises. This increases the amount of insulin produced in your body.
Although cow’s milk has a low glycemic index, it contains androgens, estrogen, progesterone and glucocorticoids, which also provoke keratinization and sebum production. Milk also contains amino acids (eg arginine, leucine, and phenylalanine) that produce insulin when combined with carbohydrates. Other components of milk that might induce comedones include whey proteins and iodine.
Caffeine, theobromine, and serotonin found in chocolate may also increase insulin production.
Food containing fatty acids
Fatty acids are needed to form sebum. Studies show that some monounsaturated fatty acids, such as sapienic acid and some vegetable oils, can increase sebum production. However, the essential fatty acids linoleic, linolenic and gamma-linolenic acid can unblock the follicles and reduce sebum production.
Why does acne eventually clear up?
We do not understand why acne eventually clears up. It does not always coincide with a reduction in sebum production or with a reduction in the number of bacteria. It may relate to changes in the sebaceous glands themselves or to the activity of the immune system.
Classification of acne in children
Prepubertal acne has been classified into the following age groups by a panel convened by the American Acne and Rosacea Society 1):
- Neonatal acne: Neonatal acne — birth to 6 weeks of age.
- Infantile acne: Infantile acne — 6 weeks to 1 year of age.
- Mid-childhood acne: Mid-childhood acne — 1–6 years of age
- Preadolescent acne: Preadolescent acne — 7–12 years (or up to menarche if female)
- Adolescent acne: Adolescent acne ≥12 to ≤19 years or after menarche if female.
Neonatal acne
Neonatal acne — birth to 6 weeks of age. Neonatal acne is estimated to affect 20% of newborns. Neonatal acne takes the form of comedones (whiteheads and blackheads) that extend from the scalp, upper chest, and back, and inflammatory lesions (erythematous papules and pustules) on the cheeks, chin, and forehead. Neonatal acne can be mistaken for neonatal cephalic pustulosis (shown above).
Neonatal acne does not usually result in scarring. It is more likely to affect boys more than girls, at a rate of 5:1.
Infantile acne
Infantile acne — 6 weeks to 1 year of age. Infantile acne is rare. It occurs in infants up to 16 months of age and presents as comedones, papules, pustules, and occasional nodules. It predominantly affects the cheeks. Occasionally, it leaves scarring.
Infantile acne can rarely persist until puberty, but it is not associated with underlying endocrine abnormalities. Male infants are affected more often than girls, at a rate of 3:1.
Mid-childhood acne
Mid-childhood acne — 1–6 years of age. Acne in this age group is very rare. An endocrinologist should be consulted to exclude possible hyperandrogenism.
Preadolescent acne
Preadolescent acne — 7–12 years (or up to menarche if female). Acne can be the first sign of puberty, and it is common to find acne in this age group.
It often presents as comedones in the ‘T-zone’, the region of the face covering the central forehead and the central part of the face (eg, the brow, nose, and lips).
Baby acne
Babies can develop blemishes on their face that looks exactly like acne commonly seen in teens. Although the cause of baby acne is unknown, it may be the result of maternal or infant hormones (androgens) stimulating glands in the face to produce oil, or sebum.
Baby acne can essentially be divided into 2 groups:
- Neonatal acne, which affects babies in their first month of life. Neonatal acne occurs in about 20% of newborns.
- Infantile acne, which typically affects babies 3–16 months of age. Infantile acne appears to be less common.
Neonatal acne that is confined to the face is called benign cephalic pustulosis, while infantile acne is usually more severe than neonatal acne and consists of more lesions. Infantile acne may last a few weeks to a few months, but most cases usually resolve by age 3. Males tend to be more affected than females, although this reason is unknown.
In general, baby acne is harmless and does not require urgent care. If you have any questions or feel that the acne on your baby’s skin is worsening despite using daily cleansing with a gentle soap, it is best to see your pediatrician. Additionally, if your baby is prone to scratching or picking at these lesions, there is a risk the affected areas could develop a bacterial skin infection, and it is best to seek further medical care.
Figure 3. Baby acne
Baby acne signs and symptoms
Baby acne consists of multiple red, raised pimples and pus-filled bumps, commonly found on the baby’s face, neck or trunk. Skin can have blackheads and whiteheads present as well. Pitting and scarring of the affected areas can occur in approximately 10–15% of affected infants.
Baby acne treatment
In mild cases of baby acne, using a daily cleanser is usually the first step in treatment. Gentle, fragrance-free cleansers are best and should be applied to the affected area daily. Newborns and infants have very sensitive skin, so vigorous scrubbing should be avoided.
Treatments your doctor may prescribe
In mild cases, prescription therapy is generally unnecessary, and the lesions may resolve with gentle cleansing of the skin. The first-line treatment most physicians prescribe is 2.5% benzoyl peroxide. This is an gel that is applied to the skin; it is a commonly used acne product. It is generally well tolerated but may cause dryness. The next line of therapy, in severe cases, is to add an oral antibiotic. Most infants are able to stop oral antibiotics within 18 months. Rarely, cases of acne could be made worse by a fungus, which would require a topical antifungal applied to the skin for treatment. Your baby’s pediatrician may request the help of a pediatric dermatologist for severe cases of acne. Furthermore, in severe cases or those resistant to therapy, an investigation for an underlying hormonal (endocrine) disorder may be warranted.
How does acne develop?
Acne is caused by clogged sebaceous glands in the pores of the skin. The sebaceous glands produce oil (sebum), which normally travels via hair follicles to the skin surface. If skin cells plug the follicles, blocking the oil, skin bacteria called Cutibacterium acnes (formerly Propionibacterium acnes) grow inside the follicles, causing inflammation. Acne progresses in the following manner:
- Incomplete blockage of the hair follicle results in blackheads (a semisolid, black plug)
- Complete blockage of the hair follicle results in whiteheads (a semisolid, white plug)
- Infection and irritation cause whiteheads to form
- The plugged follicle bursts, spilling oil, skin cells, and the bacteria onto the skin surface. In turn, the skin becomes irritated and pimples or lesions develop
Acne can be superficial (pimples without abscesses) or deep (when the inflamed pimples push down into the skin, causing pus-filled cysts that rupture and result in larger abscesses).
What causes acne in children?
Neonatal acne is thought to be a result of hyperactive sebaceous glands responding to neonatal androgens and maternal androgens that have crossed through the placenta. Androgen levels wane after approximately 1 year. At around 7 years of age, androgen production restarts, with the onset of adrenarche.
From birth to around 12 months of age, luteinizing hormone (LH) levels are similar to those during puberty. In males, this results in increased testosterone production and may explain the higher incidence of acne in boys of this age compared to girls.
Sebum production leads to increased colonization of the hair follicles by the acne bacteria, Cutibacterium acnes (formerly Propionibacterium acnes) and, as in adult acne, this results in follicular obstruction by sebum and keratin debris, and to inflammation.
What are the symptoms of acne in children?
Acne can occur anywhere on the body. It is most common in areas where there are more sebaceous glands, such as:
- Face
- Chest
- Upper back
- Shoulders
- Neck
Symptoms can occur a bit differently in each child. They can include:
- Small bumps that are skin-colored or white (whiteheads)
- Small bumps that are dark in color (blackheads)
- Red, pus-filled pimples that may hurt
- Solid, raised bumps (nodules)
- Darker areas of skin
- Scarring
The symptoms of acne can be like other health conditions. Make sure your child sees his or her healthcare provider for a diagnosis.
Acne in children diagnosis
In pre-pubertal children with acne, a clinical history and examination may detect accelerated growth, early sexual development, and signs of hyperandrogenism, such as hirsutism. A bone-age X-ray of the left hand and a wrist X-ray should be considered for children with indications of accelerated growth.
The majority of children with acne will not require further investigations.
However, if the findings on a clinical history and examination in children aged 1–6 years old indicate that further investigation is required, or if the acne is severe or unresponsive to treatment, an endocrinology referral may be required. The levels of the following hormones should be measured:
- Free and total testosterone
- Dehydroepiandrosterone (DHEA)
- Luteinizing hormone (LH)
- Follicle-stimulating hormone (FSH)
- Prolactin
- 17-hydroxyprogesterone.
Acne treatment for kids
Treatment for children with acne is generally the same as for adults with acne, with the exception of restrictions by age for tetracyclines. All treatments take at least 1–2 months to result in significant improvement.
Treatment of mild acne
The general management of mild acne involves gently washing the skin twice daily and using oil-free moisturizers.
Avoid greasy emollients, hair pomades, and the use of comedogenic products on the affected area.
Benzoyl peroxide
Benzoyl peroxide is a topical antiseptic and is available as a wash, gel, or lotion that can be bought over the counter. It can be used alone for mild acne or in combination with oral therapy for more severe cases.
Benzoyl peroxide should be applied to all the areas affected by acne. If the skin is particularly sensitive, benzoyl peroxide treatment can be started at a low concentration of 2.5%, as higher concentrations are more likely to cause dryness and irritation.
Topical retinoids — tretinoin and adapalene
Topical retinoids are creams, lotions, and gels enriched with a derivative of vitamin A (eg, tretinoin and adapalene). If the skin is sensitive, an oil-free moisturiser or sunscreen can be added.
A topical retinoid should be applied to the whole of the affected skin. It is often initially used 2–3 times a week, and applications are increased to daily, as tolerated, if there is no improvement in the acne.
Topical retinoids are also available in combination with benzoyl peroxide or a topical antibiotic.
Treatment of moderate acne
The treatment for children with moderate acne is 250–500 mg of the oral antibiotic, erythromycin, in single or split dosing. Erythromycin is best used in combination with a topical regimen, such as benzoyl peroxide and/or a topical retinoid, to reduce Cutibacterium acnes (formerly Propionibacterium acnes) resistance.
Trimethoprim and combined trimethoprim and sulphamethoxazole, have both been used if there is bacterial resistance to erythromycin or if erythromycin is contraindicated due to adverse effects. Doxycycline and minocycline should be used only in children over 12 years of age.
Isotretinoin is sometimes used in moderate acne when antibiotics and topical therapy have been unsuccessful.
Treatment of severe acne
The treatment of severe acne is the same as for moderate acne. Isotretinoin can be prescribed if there is an inadequate response to oral antibiotics.
Doses of isotretinoin ranging from 0.2 to 1 mg/kg/day have been used safely in infants from 5 months of age and in children with severe acne. The isotretinoin capsules can be frozen to make it easier to divide them into halves or quarters, and freezing can help mask the unpleasant taste.
Premature epiphyseal closure is a theoretical concern with isotretinoin, but this has only been reported once when isotretinoin was used to treat acne in a 14-year-old boy at a dose of 0.75 mg/kg/day.
Deep nodules can be treated by injections with low-concentration intralesional triamcinolone acetonide at a dose of 2.5 mg/mL.
Suitable food if you have acne
Some people with acne have reported improvement in their skin when they follow a low-glycemic index diet and increase their consumption of whole grains, fresh fruits and vegetables, fish, olive oil, garlic, while keeping their wine consumption moderate.
It’s a good idea to drink less milk and eat less of high glycemic index foods such as sugar, biscuits, cakes, ice creams and bottled drinks. Reducing your intake of meat and amino acid supplements may also help.
Seek medical help if you are concerned about your skin, as changing diet does not always help.
References [ + ]