Contents
What is peritonsillar abscess
Peritonsillar abscess, also known as quinsy, is the localized collection of pus in peritonsillar space at the back of the mouth, next to one of the tonsils (between the tonsillar capsule and superior constrictor muscle) 1). Peritonsillar abscess can be very painful and can make it difficult to open your mouth. Peritonsillar abscess can also cause swelling that can push the tonsil toward the uvula (the dangling fleshy object at the back of the mouth). This can block the throat, making it hard to swallow, speak, and sometimes even breathe. Peritonsillar abscess is usually caused by a complication of tonsillitis. Peritonsillar abscess most often occurs in older children, adolescents, and young adults. But this infection can occur in all age groups, with the highest incidence occurring in adults 20 to 40 years of age 2). Peritonsillar abscess is rare below five years of age 3). Peritonsillar abscess is rare now that antibiotics are used to treat tonsillitis.
The symptoms of a peritonsillar abscess include:
- Severe sore throat that is worse on one side
- Fever and chills
- Swollen lymph glands
- Trouble swallowing
- Pain when you speak
Peritonsillar abscess is a common infection of the head and neck region. With an incidence of approximately 1 in 10,000, it is the most common deep head and neck space infection that presents in the emergency department 4). There is no sexual or racial predilection. In the United States, the incidence is 30 per 100,000 among patients who are 5 to 59 years of age.
The prognosis of peritonsillar abscess in most patients is excellent. However, if there are airway compromise and delay in treatment, death can occur.
If you think you have an abscess in the back of your throat, you need to see a doctor. A peritonsillar abscess that isn’t treated can lead to more serious health problems.
The usual treatment for a peritonsillar abscess involves having a doctor drain the abscess. The doctor does this either by withdrawing the pus with a needle (called aspiration) or making a small cut in the abscess with a scalpel so the pus can drain out.
If this doesn’t work, a patient’s tonsils might have to be removed in a procedure called a tonsillectomy. This is especially true for people who have had tonsillitis a lot or who have had a peritonsillar abscess in the past.
If it’s hard to eat or drink, patients may need IV (intravenous, given into a vein) fluids for hydration. A doctor also will prescribe painkillers and antibiotics. Whenever you take antibiotics, always finish the full course of the medicine as prescribed, even if you feel better after a few days. Otherwise, the infection could come back.
People who have a tonsillectomy may need a brief stay in the hospital. That way, doctors can keep an eye on them to make sure everything went as planned.
See your doctor right away if you have had tonsillitis and you develop symptoms of peritonsillar abscess. Call your doctor right away if you have trouble breathing, swallowing, talking, or if you start to drool. These are symptoms of a more serious abscess and need immediate medical attention.
See your doctor if you have:
- Breathing problems
- Trouble swallowing
- Pain in the chest
- Persistent fever
- Symptoms that get worse
Peritonsillar abscess complications
Rare complications of peritonsillar abscess include:
- Parapharyngeal abscess
- Retropharyngeal abscess
- Laryngeal edema leading to airway compromise
- Rarely pneumonia or lung abscess following aspiration of a ruptured abscess.
- Sepsis (infection in the blood) 5)
- Airway obstruction
- Extension of infection into the deep tissues of the neck or superior mediastinum with cellulitis of the jaw, neck, or chest
- Endocarditis (rare)
- Fluid around the lungs (pleural effusion)
- Inflammation around the heart (pericarditis)
- Life-threatening hemorrhage secondary to erosion or septic necrosis into carotid sheath
- Poststreptococcal complications, such as glomerulonephritis and rheumatic fever, when infection is caused by group A Streptococcus
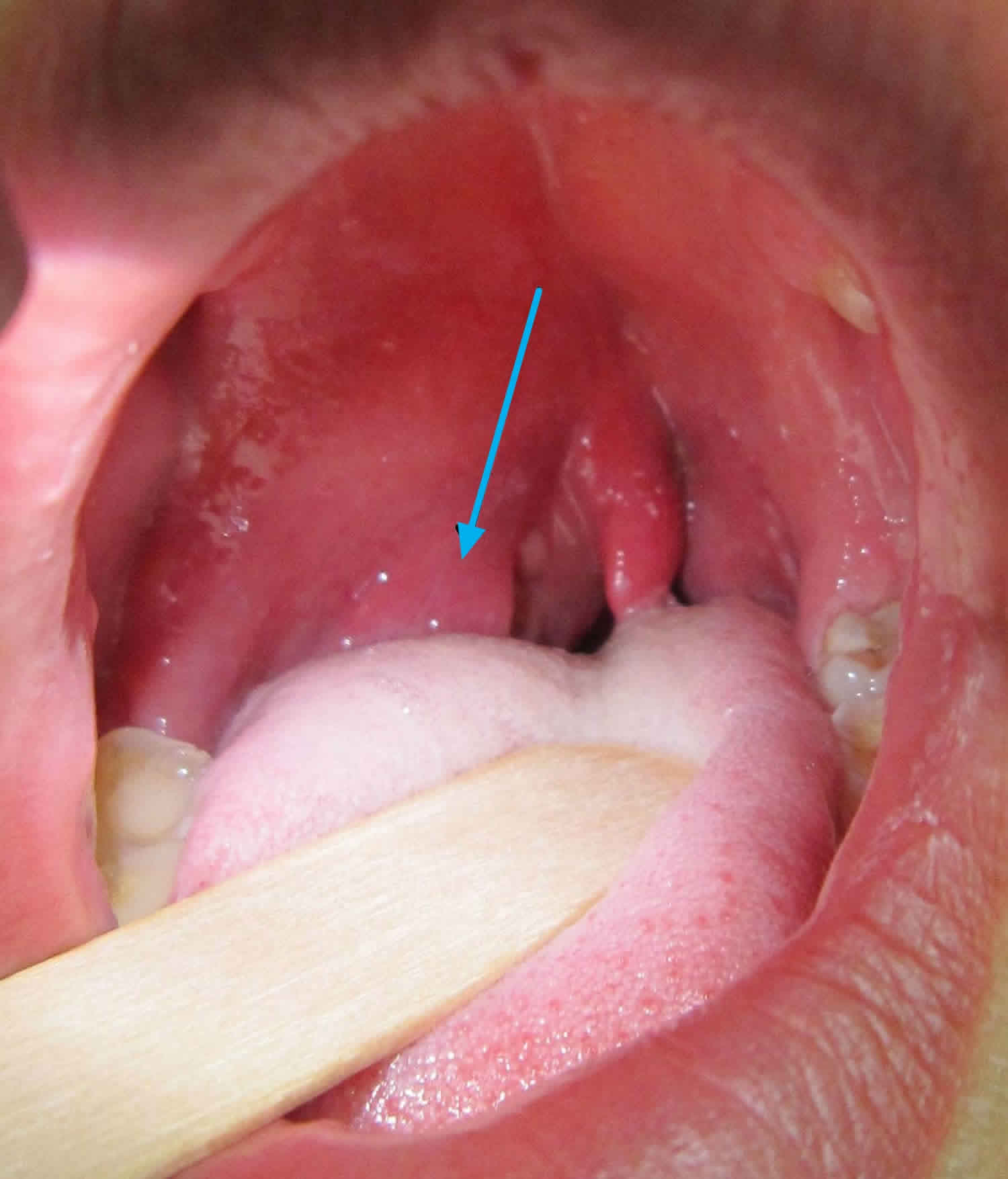
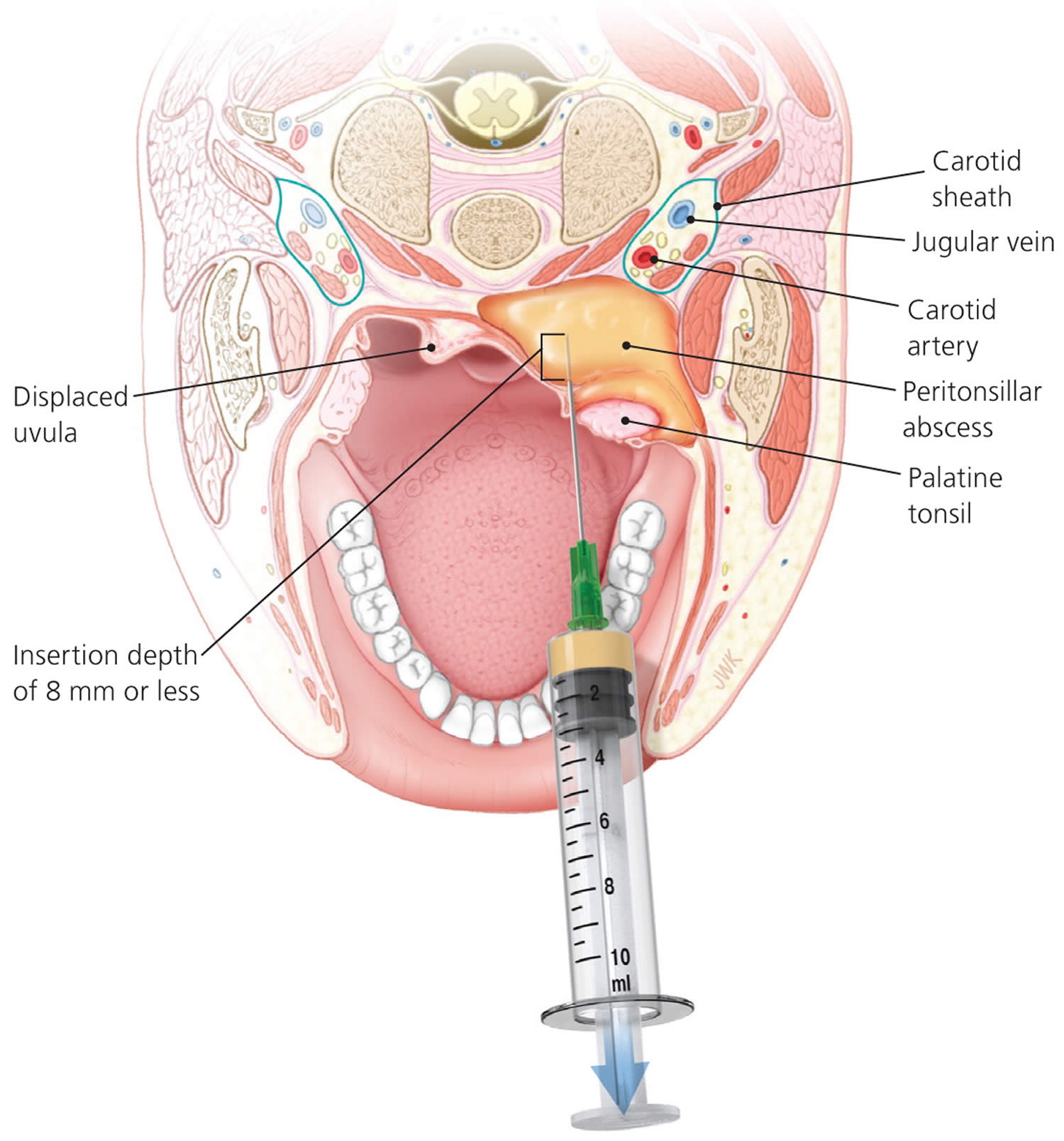
Figure 1. Peritonsillar abscess
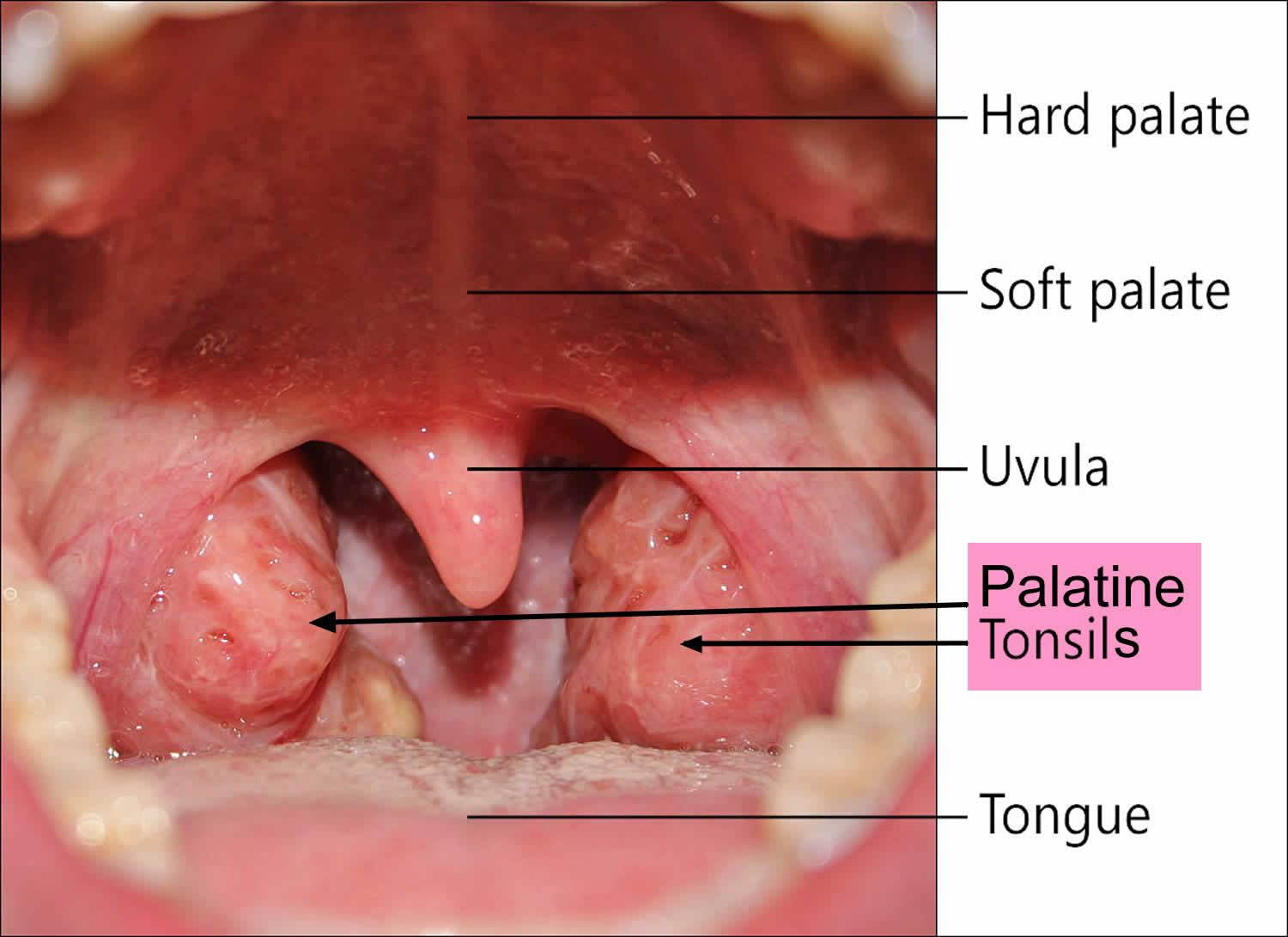
Tonsils anatomy
The two palatine tonsils are the oval-shaped areas of pink tissue on each side at the back of your throat. The tonsils are formed during the last months of gestation and grow irregularly, reaching their largest size by the time a child is six to seven years of age 6). The tonsils typically begin to involute gradually at puberty, and after 65 years of age, little tonsillar tissue remains 7). Each tonsil has a number of crypts on its surface and is surrounded by a capsule between it and the adjacent constrictor muscle through which blood vessels and nerves pass.
Peritonsillar space consists of loose connective tissue between the fibrous capsule of palatine tonsils medially and superior constrictor muscle laterally. The anterior tonsillar pillar (palatoglossal arch) and the posterior tonsillar pillar (palatopharyngeal arch) contribute to anterior and posterior limits, respectively. Superiorly, this space is related to torus tubarius, while pyriform sinus forms the inferior limit. Since this space is composed of loose connective tissue, it is highly susceptible to abscess formation following infection 8).
Peritonsillar abscess is a localized infection where pus accumulates between the fibrous capsule of the tonsil and the superior pharyngeal constrictor muscle 9).
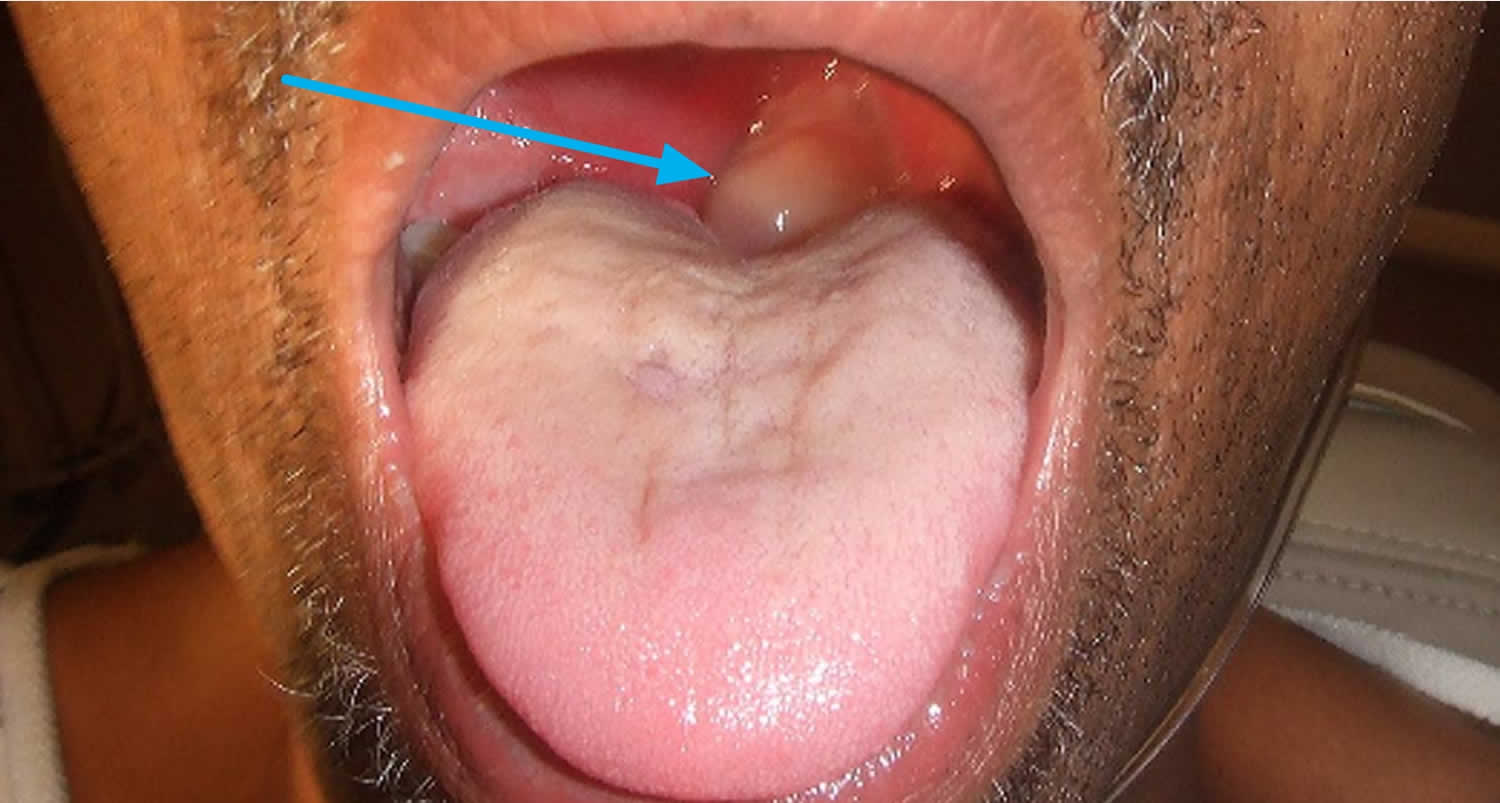
Figure 2. Normal palatine tonsils
Peritonsillar abscess causes
Most peritonsillar abscesses are caused by the same bacteria that cause Strep throat (group A beta-hemolytic streptococcus). Sometimes, other types of bacteria are involved. Peritonsillar abscess usually occurs as a complication of acute tonsillitis. Infectious mononucleosis can also result in abscess formation. Rarely, it may occur de novo without any prior history of a sore throat. If the infection breaks out of a tonsil and gets into the space around it, an abscess can form. Luckily, peritonsillar abscesses aren’t that common these days because doctors use antibiotics to treat tonsillitis.
Tooth and gum disease can increase the chances of a peritonsillar abscess, as can smoking — more good reasons to brush your teeth and not smoke 10).
Cultures most commonly reveal Group A beta-hemolytic streptococcus. The next most commonly found organisms include staphylococcal, pneumococcal, and hemophilic organisms. Rarely, Lactobacillus and filamentous forms like Actinomyces and Micrococcus may be present. Most of the time, the growth is mixed, with both aerobic and anaerobic organisms.
The exact pathophysiology of peritonsillar abscess formation remains unknown to date. The most accepted theory is that an infection develops in crypta magna that then spreads beyond the confines of the tonsillar capsule, initially causing peritonsillitis and then developing into a peritonsillar abscess 11).
Another proposed mechanism is necrosis and pus formation in the capsular area which then obstructs the Webers glands 12), resulting in abscess formation. These are minor salivary glands in peritonsillar space, located in the space just superior to the tonsil in the soft palate and is connected by a duct to the surface of the tonsil, which are responsible for clearing debris from the tonsillar area and assist with digesting food particles trapped in the tonsillar crypts 13). If Weber glands become inflamed, local cellulitis can develop. As the infection progresses, the duct to the surface of the tonsil becomes obstructed from surrounding inflammation. The resulting tissue necrosis and pus formation produces the classic signs and symptoms of peritonsillar abscess 14). These abscesses are generally formed within the soft palate, just above the superior pole of the tonsil, which coincides with the typical location of a peritonsillar abscess 15) The lack of these abscesses in patients who have undergone tonsillectomy supports the theory that Weber glands may contribute to the pathogenesis of peritonsillar abscesses 16).
Other clinical variables associated with the formation of peritonsillar abscesses include significant periodontal disease and smoking 17).
Is peritonsillar abscess contagious?
Yes. The germs that cause viral and bacterial peritonsillar abscess are contagious.
To prevent the spread of a bacterial or viral infection to others:
- Stay at home when you are ill
- Ask your doctor when it’s all right for you to return to work or school
- Cough or sneeze into a tissue.
- Wash your hands after sneezing or coughing
Peritonsillar abscess prevention
You can take a few precautions to lower your risk of getting an abscess in your tonsils — like not smoking and making sure you keep your teeth and mouth clean.
But sometimes a peritonsillar abscess is beyond your control. If you think you have an abscess, call your doctor right away. The earlier a doctor diagnoses it, the easier treatment is likely to be.
The best prevention is to practice good hygiene:
- Wash your hands thoroughly and frequently, especially after using the toilet and before eating
- Avoid sharing food, drinking glasses, water bottles or utensils
- Replace your toothbrush after being diagnosed with tonsillitis
Peritonsillar abscess signs and symptoms
One or both tonsils become infected. The infection most often spreads to behind the tonsil. It can then spread down into the neck and chest. Swollen tissues can block the airway. This is a life-threatening medical emergency.
The abscess can break open (rupture) into the throat. The content of the abscess can travel into the lungs and cause pneumonia.
Often, the first sign of a peritonsillar abscess is a sore throat. As the abscess develops, other symptoms start, such as:
- Red, swollen tonsils
- A tonsil that’s pushing against the uvula
- Tender, swollen glands (lymph nodes) on one side of the neck
- Severe pain on one side of the throat
- Difficulty and pain when swallowing (odynophagia) or opening the mouth
- Fever and chills
- Severe throat pain that is usually on one side
- Ear pain on the side of the abscess
- Difficulty opening the mouth, and pain with opening the mouth
- Swallowing problems
- Drooling or inability to swallow saliva
- Facial or neck swelling
- Earache
- Headache
- Muffled or hoarse voice
- Tender glands of the jaw and throat
Patients with peritonsillar abscess appear ill and report malaise, fever, progressively worsening throat pain, and dysphagia 18). The associated sore throat is markedly more severe on the affected side and is often referred to the ear on the same side as the peritonsillar abscess. Physical examination usually reveals trismus (reduced opening of the mouth), with difficulty opening the mouth secondary to inflammation and spasm of masticator muscles 19). Swallowing can be difficult and painful 20). The combination of painful swallowing (odynophagia) and difficulty in swallowing (dysphagia) often leads to the pooling of saliva and subsequent drooling. Patients often speak in a muffled or “hot potato” voice. Marked tender cervical lymphadenitis may be palpated on the affected side. Inspection of the oropharynx reveals tense swelling and erythema of the anterior tonsillar pillar and soft palate overlying the infected tonsil. The tonsil is generally displaced inferiorly and medially with deviation of the uvula to the opposite side (see Figure 1).
An peritonsillar abscess that’s not treated quickly can lead to serious problems — for example, the infection may go into the jaw and neck. If the abscess pops, the infection may spread to the chest and lead to pneumonia.
Peritonsillar abscess diagnosis
See your doctor if you have a sore throat with a fever or any of the other problems that can be caused by a peritonsillar abscess. It’s rare that an abscess will get in the way of your breathing, but if it does, you may need to go to the emergency room right away.
The doctor will examine your mouth, throat, and neck. He or she also may take a throat culture and a blood test. On rare occasions, a doctor may order a CT scan or ultrasound.
The most common history and physical examination findings in patients with peritonsillar abscess are:
- Cervical lymphadenitis
- Drooling
- Erythematous, swollen soft palate with uvula deviation to contralateral side and enlarged tonsil
- Muffled voice (“hot potato” voice)
- Rancid or foul-smelling breath (fetor)
- Trismus
In several retrospective studies, infectious mononucleosis has been reported as a coinfection in 1.5% to 6% of peritonsillar abscess cases 21), making it a possible alternative diagnosis and comorbidity. This is particularly true in adolescents and young adults. Testing for infectious mononucleosis should be based on the patient history, examination findings (e.g., splenomegaly, lymphadenopathy, bilateral tonsillar infection), and clinical suspicion. If infectious mononucleosis is confirmed, amoxicillin use should be avoided secondary to the associated drug-induced rash 22).
The following tests may be done:
- Aspiration of the abscess using a needle
- CT scan
- Fiber optic endoscopy to check if the airway is blocked
Patients with peritonsillar cellulitis often present with symptoms similar to peritonsillar abscess, making it difficult to differentiate between the conditions. In peritonsillar cellulitis, the area between the tonsil and its capsule is erythematous and edematous, without an obvious area of fluctuance or pus formation. Often, these two conditions are distinguished by the absence of pus on needle aspiration, which indicates cellulitis. If the presence of an abscess remains uncertain after needle aspiration, radiologic testing may be helpful. Computed tomography (CT) with contrast media enhancement can be used to demonstrate the presence and extent of an abscess. Alternatively, several small studies have shown that intraoral ultrasonography, if available, can accurately identify and distinguish abscess from cellulitis 23).
If there is suspicion that infection has spread beyond the peritonsillar space or if there are complications involving the lateral neck space, CT or magnetic resonance imaging (MRI) is required 24). Lateral neck infections should be suspected if there is swelling or induration below the angle of the mandible or medial bulging of the pharyngeal wall. Besides accurately diagnosing peritonsillar abscess, CT can detect potential airway compromise and demonstrate the spread of infection to the contiguous deep neck spaces. MRI is superior to CT for soft-tissue definition and is therefore better at detecting complications from deep neck infections, such as internal jugular vein thrombosis or erosion of the abscess into the carotid sheath 25). Disadvantages of MRI include longer scanning times, higher cost, and the potential for claustrophobia 26).
Peritonsillar abscess treatment
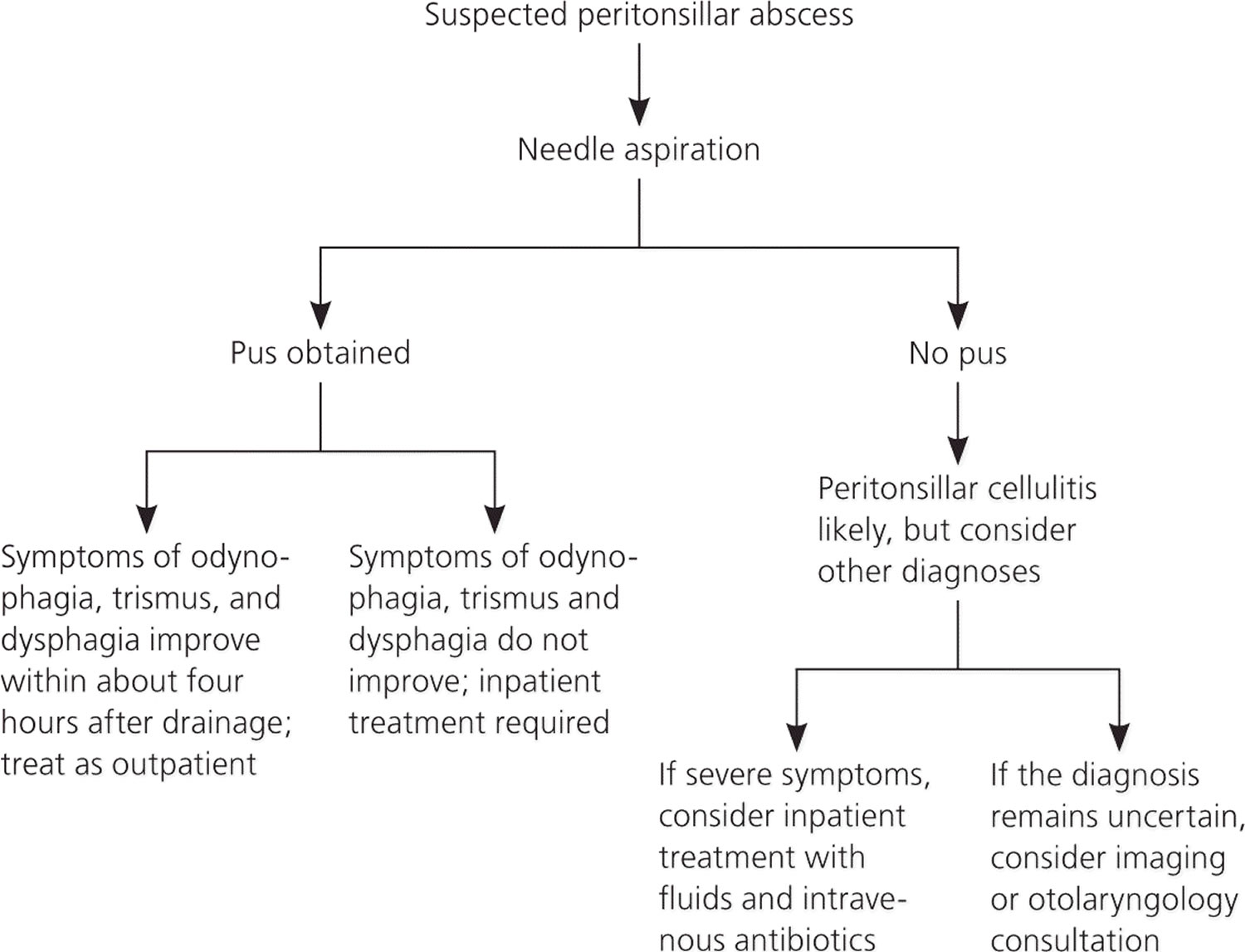
Drainage, antibiotic therapy, and supportive therapy for maintaining hydration and pain control are the cornerstones of treatment for peritonsillar abscess 27). Figure 3 outlines the basic treatment approach to patients presenting with a peritonsillar abscess.
Your doctor will need to remove the pus from the abscess. Your doctor will numb the skin around the abscess. He or she will either take the pus out with a needle or make a small cut in the abscess so the pus can drain out. Surgery to remove your tonsils (called a tonsillectomy) is also an option. You will probably only need surgery if you have had many tonsil infections or abscesses before.
- Aspiration with a wide-bore needle serves both diagnostic and therapeutic purposes. The aspirated pus can be sent for culture sensitivity, and in some cases, further incision and drainage may not be required.
- Intraoral incision and drainage are carried out in a sitting position to prevent aspiration of pus. Oral and laryngeal mucosa is anesthetized with lidocaine 10% spray. The incision is given at the point of the maximum bulge above the upper pole of the tonsil. Another alternative site for incision is lateral to the point of junction of the anterior pillar with a line drawn through the base of the uvula. Quinsy forceps or No. 11 guarded blade and then sinus forceps are inserted to break the loculi. The opening created is left open to drain, and the patient is asked to gargle with sodium chloride solution. This helps in self-drainage of accumulated material.
- In uncooperative, young patients or those affected in an unusual location, the procedure might have to be done under general anesthesia.
Your pain and symptoms should get better after the pus is drained. Your doctor will likely prescribe antibiotics to make sure the infection goes away completely. He or she may also give you medicine to help relieve the pain.
Although no longer routinely performed, immediate tonsillectomy should be considered in patients who have strong indications for it, especially those with a history of recurrent tonsillitis, because there is a recurrence rate up to 40% in these patients compared with 10% to 15% for the average patient 28). Tonsillectomy may also be favored in children because they are likely to have recurrent episodes of tonsillitis and may be intolerant of drainage procedures under local anesthesia 29).
Figure 3. Peritonsillar abscess treatment algorithm
[Source 30) ]Drainage
Some type of drainage procedure is appropriate for most patients who present with a peritonsillar abscess 31). Exceptions include small abscesses (less than 1 cm) without muffled voice, drooling, or trismus. The main procedures include needle aspiration, incision and drainage, or immediate tonsillectomy (at time of presentation or shortly thereafter). Most studies comparing different surgical methods have found that all were equally effective for the treatment of peritonsillar abscess, and there were no statistically significant differences in patient outcomes 32). The acute surgical management of peritonsillar abscess has evolved from immediate tonsillectomy to primarily incision and drainage or needle aspiration 33). Peritonsillar aspiration is a technique well suited for family physicians with proper training. Drainage or aspiration should be performed in a setting where possible airway complications can be managed and the patient can be observed for a few hours afterward to ensure adequate oral fluid intake 34). Table 1 describes the technique for needle aspiration of a peritonsillar abscess 35). Physicians must be aware of important anatomic relationships when performing needle aspiration (Figure 4). If a physician is not comfortable aspirating the abscess, appropriate antibiotics and intravenous fluids should be administered while awaiting otolaryngology consultation.
Table 1. Technique for Needle Aspiration of Peritonsillar Abscess
| Make sure the setting is suitable for managing airway complications. |
| Check that adequate lighting and suction are available. |
| Ask the patient to sit slightly forward and at eye level to the clinician. |
| Gently palpate soft palate to localize fluctuant area. |
| Apply topical anesthetic using Cetacaine spray. |
| Wait a few minutes for topical anesthetic to take effect, then draw up 6 to 10 mL of 1% to 2% lidocaine with epinephrine. |
| Use a 25-gauge 1 ½-inch needle to inject local anesthesia into the mucosa overlying the fluctuant area. |
| Retract the tongue using a tongue depressor. |
| Insert an 18-gauge spinal needle attached to a 10-mL syringe into area of maximum fluctuance and aspirate. |
| Do not insert the needle more than 8 mm. |
| If positive for pus, aspirate until no pus returns. |
| If negative for pus, withdraw needle and redirect slightly inferior; be aware that the carotid artery is 2 cm posterior and lateral to tonsillar pillar, and the risk of puncture increases the more inferior the needle is directed. |
| If aspiration is unsuccessful, perform imaging to confirm the presence of abscess; arrange otolaryngology consultation for possible incision and drainage as appropriate. |
Figure 4. Peritonsillar abscess needle aspiration important anatomic relationships
Footnote: When performing needle aspiration for peritonsillar abscess, the physician should be aware of important anatomic relationships, particularly the carotid artery, which lies posterior and lateral to the tonsil. To avoid this structure, the insertion should be at the superior pole of tonsil, not too lateral, and at a depth of 8 mm or less.
[Source 37) ]Peritonsillar abscess antibiotics
Peritonsillar abscesses are a polymicrobial mixture of aerobic and anaerobic bacteria. Group A streptococcus and Streptococcus milleri group (a subgroup of viridans streptococci) are the most commonly isolated aerobes recovered from culture, whereas Fusobacterium necrophorum is the predominant anaerobe 38). Common organisms associated with peritonsillar abscess are listed in Table 2. Initial empiric antibiotic therapy should include antimicrobials effective against streptococcus and oral anaerobes 39). There is almost universal sensitivity of streptococcus species to penicillin, and several studies show the clinical effectiveness of intravenous penicillin alone after adequate drainage of the abscess 40). However, there are growing concerns about the polymicrobial nature of peritonsillar abscesses. Culture reports demonstrate a greater than 50% penicillin-resistance rate among pathogens other than streptococcus found in peritonsillar abscess, which has led to the routine use of broad-spectrum antibiotics as first-line therapy 41). Macrolides should be avoided secondary to Fusobacterium resistance 42). Table 3 lists suggested antimicrobial regimens 43).
Intravenous fluids are started, as the patient is usually dehydrated 44).
A suitable intravenous antibiotic is started. The antibacterial spectrum should include gram-positive, gram-negative, and anaerobes. Commonly used empirical antibiotics are penicillins like ampicillin/amoxicillin in combination with metronidazole or clindamycin. (Ideally, antibiotic therapy should be started as per culture sensitivity reports). A patient is shifted to oral antibiotics once he improves and can tolerate orally.
Analgesics and antipyretics are given to relieve pain and fever.
The role of steroids is controversial. A study 45) shows that a single dose of intravenous (IV) dexamethasone reduces the hospital stay and severity of symptoms.
These conservative measures can cure peritonsillitis; however, for peritonsillar abscess, drainage is a must along with medical management.
Table 2. Common Organisms Associated with Peritonsillar Abscess
| Aerobic bacteria |
| Corynebacterium |
| Group A streptococcus |
| Staphylococcus aureus |
| Streptococcus milleri group (Streptococcus intermedius, Streptococcus anginosus, Streptococcus constellatus) |
| Anaerobic bacteria |
| Bacteroides |
| Fusobacterium |
| Peptostreptococcus |
| Prevotella |
Table 3. Suggested Antimicrobial Regimens for the Treatment of Peritonsillar Abscess
| Intravenous antibiotic therapy |
| Penicillin G, 10 million units every 6 hours, plus metronidazole (Flagyl), 500 mg every 6 hours |
| Ampicillin/sulbactam (Unasyn), 3 g every 6 hours |
| Third-generation cephalosporin (e.g., ceftriaxone, 1 g every 12 hours) plus metronidazole, 500 mg every 6 hours |
| Piperacillin/tazobactam (Zosyn), 3.375 g every 6 hours (maximum daily dosage of 18 g) |
| If penicillin allergic, then clindamycin, 900 mg every 8 hours |
| If MRSA is a concern, then vancomycin, 1 g every 12 hours, plus metronidazole, 500 mg every 6 hours |
| Oral antibiotic therapy |
| Penicillin VK, 500 mg every 6 hours, plus metronidazole, 500 mg every 6 hours |
| Amoxicillin/clavulanate (Augmentin), 875 mg every 12 hours |
| Third-generation cephalosporin (e.g., cefdinir [Omnicef], 300 mg every 12 hours) plus metronidazole, 500 mg every 6 hours |
| Clindamycin, 300 to 450 mg every 8 hours |
| If MRSA is a concern, then linezolid (Zyvox), 600 mg every 12 hours, plus metronidazole, 500 mg every 6 hours |
Inpatient versus outpatient management
Patients with a peritonsillar abscess can be treated as outpatients, but a small percentage may require hospitalization 48). The most common reasons for admission are dehydration, inability to manage oral fluid intake, airway concerns (kissing tonsils), and failure of outpatient management 49). Other comorbid conditions that warrant inpatient management include diabetes mellitus, immunosuppressive disease, chronic immunosuppressive medication use (including prolonged corticosteroid use), or signs of sepsis 50). Complication rates are higher in patients 40 years or older compared with younger patients.24,25 Hospital stays averaged two to four days for all patients 51). If the decision is made to pursue outpatient management, patients should be observed for a few hours after drainage of the abscess to ensure they can tolerate oral fluids, antibiotics, and pain medications. Patients should continue to be monitored closely, with a follow-up appointment scheduled within 24 to 36 hours.
Adjuvant corticosteroid therapy
The acute symptoms of peritonsillar abscess result from inflammation and soft palate edema. Although corticosteroids have been used to treat edema and inflammation in other otolaryngologic diseases, their use as part of a treatment regimen for peritonsillar abscess has not been extensively studied. Two small studies investigated whether the addition of a single corticosteroid dose administered intramuscularly or intravenously (methylprednisolone, 2 to 3 mg per kg up to 250 mg, or dexamethasone, 10 mg) would speed recovery 52), 53). Patients who received the corticosteroids reported decreased pain and improved oral fluid intake within 12 to 24 hours compared with patients who did not receive corticosteroids. These differences seemed to disappear after 48 hours. The empiric use of corticosteroids for the treatment of peritonsillar abscess appears to speed recovery as demonstrated by shorter hospital stays and quicker resolution of pain. However, additional studies are needed before the routine use of corticosteroids is included in treatment protocols 54).
References [ + ]