Contents
Perineal tears
Perineal tear is a spontaneous (unintended) tear in the perineum, which is the area between the vagina and the rectum. Your perineum may tear naturally during vaginal childbirth, which strains the perineum. More than 8 in 10 women who give birth vaginally experience ‘perineal trauma’ or a perineal tear or surgical cut (also known as episiotomy) to the area between the vagina and anus. A perineal tear is distinct from an episiotomy, in which the perineum is intentionally lacerated to facilitate delivery. Over 85% of women having a vaginal birth sustain some form of perineal trauma, and 60-70% receive stitches 1). A retrospective study of 8603 vaginal deliveries found a third degree tear had been clinically diagnosed in only 50 women (0.6%) 2). However, when the same authors used anal endosonography in a consecutive group of 202 deliveries, there was evidence of third degree tears in 35% of first-time mothers and 44% of mothers with previous children 3). These numbers are confirmed by other researchers 4).
The perineum is the wall between the vagina and anus and everything that is in it (Figure 1). The female perineum is the diamond-shaped inferior outlet of the pelvis 5). This structure is at risk of trauma during labor because of spontaneous perineal tears of varying degrees or iatrogenic episiotomies. These injuries can result in disabling immediate and long-term complications in the woman.
Perineal trauma involves any type of damage to the female genitalia during labor, which can occur spontaneously or iatrogenically (medically caused) via episiotomy or instrumental delivery 6). Anterior perineal trauma can affect the anterior vaginal wall, urethra, clitoris and labia. Posterior perineal trauma can affect the posterior vaginal wall, perineal muscle, perineal body, external and internal anal sphincters, and anal canal. During labor, the majority of perineal tears occur along the posterior vaginal wall, extending towards the anus.
Perineal tears vary widely in severity. The majority are superficial and require no treatment, but severe perineal tears can cause significant bleeding, long-term pain or dysfunction.
Figure 1. Perineum
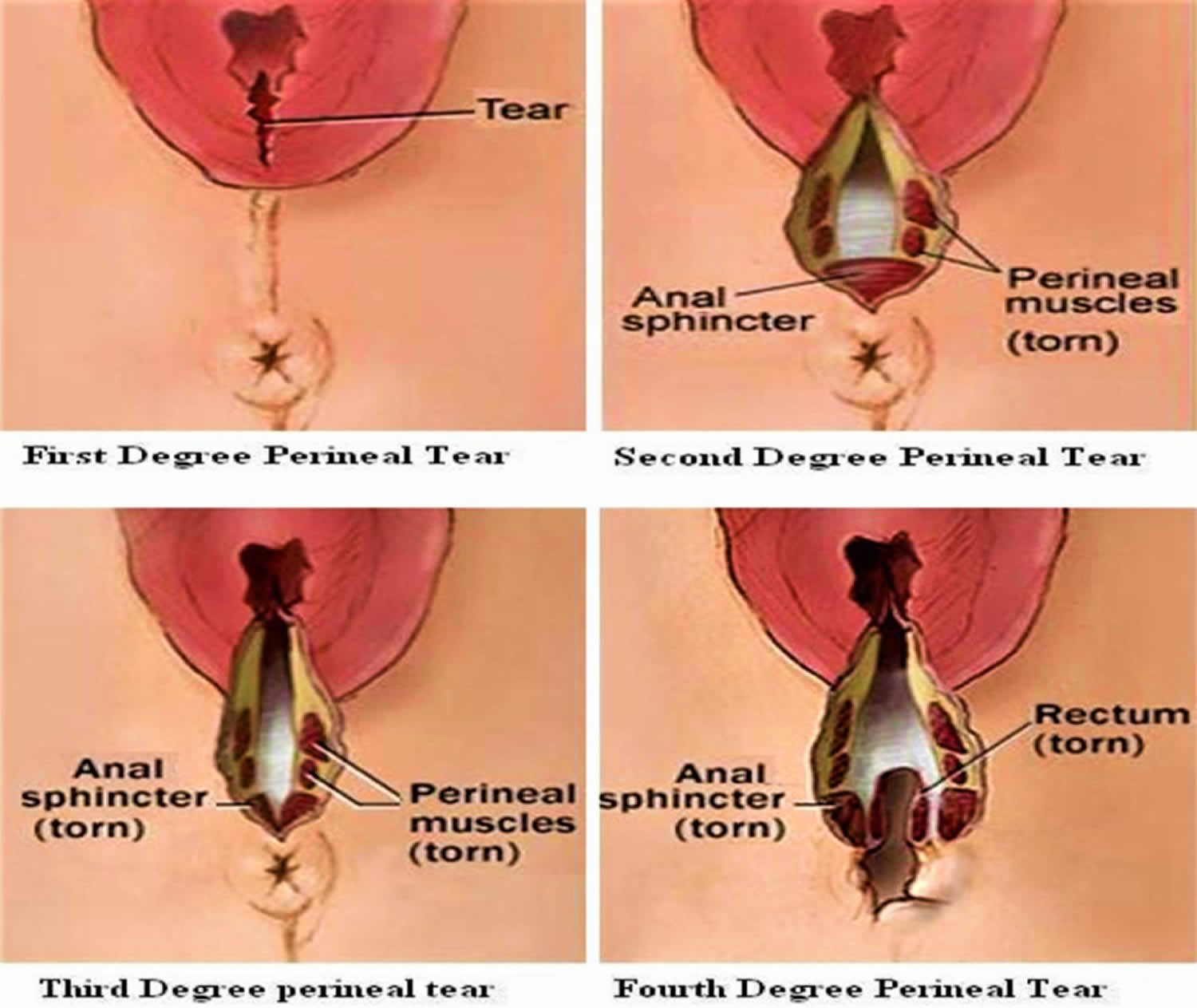
Figure 2. Perineal tears
Perineum anatomy
In a woman, the anus and the vaginal opening lie within the anatomical region known as the perineum. Each opening is surrounded by a wall, and the anal wall is separated from the vaginal wall by a mass of soft tissue including:
- The muscles of the anus (corrugator cutis ani, the internal anal sphincter and the external anal sphincter)
- The medial muscles of the urogenital region (the superficial transverse perineal muscle, the deep transverse perineal muscle and bulbocavernosus)
- The medial levator ani muscles (puborectalis and pubococcygeus)
- The fascia of perineum, which covers these muscles
- The overlying skin and subcutaneous tissue 7)
A perineal tear may involve some or all of these structures, which normally aid in supporting the pelvic organs and maintaining fecal continence 8).
Perineal tear classification
Perineal tears are classified into four categories 9):
- 1st degree tear, the laceration is limited to the fourchette and superifcial perineal skin or vaginal mucosa. 1st degree doesn’t involve the perineal muscles.
- 2nd degree tear, the laceration extends beyond fourchette, perineal skin and vaginal mucosa – to perineal muscles and fascia, but not the anal sphincter. 2nd degree doesn’t involve the anal muscles.
- 3rd degree tear, where the fourchette, perineal skin, vaginal mucosa, muscles, and anal sphincter are torn. 3rd degree doesn’t involve the anal mucosa. They can be subdivided into:
- 3a: Partial tear of the external anal sphincter involving <50% thickness
- 3b: Where >50% tear of the external anal sphincter is torn
- 3c: Where the external and internal anal sphincters are torn
- 4th degree tear, where the fourchette, perineal skin, vaginal mucosa, muscles, anal sphincter, and rectal mucosa are torn (resulting with a communication of the vagina epithelium and anal epithelium).
Perineal tear causes
Perineal tear mainly occurs in women as a result of vaginal childbirth, which strains the perineum. In humans, the head of the fetus is so large in comparison to the size of the birth canal, term delivery is rarely possible without some degree of trauma. As the head passes through the pelvis, the soft tissues are stretched and compressed
Risk factors for perineal tear
Maternal risk factors
- Nulliparity (mother has not given birth before)
- Asian ethnicity
- Vaginal birth after caesarean section
- ≤20 years of age
- Shortened perineal length (<25 mm)
Fetal risk factors
- Large fetal weight (>4000 g)
- Shoulder dystocia
- Fetal head is oriented OP (occiput posterior, i.e. face forward)
Intrapartum risk factors
- Instrumental delivery (eg forceps, vacuum)
- Prolonged second stage of labour (>60 minutes)
- Epidural use
- Oxytocin use
- Midline episiotomy
- Delivery in lithotomy or deep squatting position
Can you prevent perineal tears?
It’s not uncommon for the perineum to tear during childbirth. But there are steps you can take to help prevent perineal tear 10):
- Pay attention to your position during labor. Different positions may put less pressure on your perineum. You may feel more comfortable sitting upright, lying on your side, or getting down on your hands and knees, for example.
- Talk to your birthing coach ahead of time so you agree on when and how hard you should push.
- Have someone provide perineal support. This means pushing against the perineum to protect it from tearing as the baby’s head stretches it. This is sometimes done with a hot, moist cloth.
- Practice perineal massage. This type of massage may help make the tissue around the vagina more flexible and reduce the chance of having a perineal tear or an episiotomy.
The risk of perineal tear is reduced by the use of medio-lateral episiotomy, although this procedure is also traumatic. Epidural anesthesia and induction of labor also reduce the risk. Instrumentation (the use of forceps or ventouse) reduces the risk if the fetus is in the occiput anterior (normal) position 11).
Perineal tear diagnosis
The perineum should always be thoroughly assessed after a vaginal birth to determine the presence of any lacerations. This examination should include a digital rectal examination to evaluate the tone of the anal sphincter 12). From here, the midwife or obstetrician can decide if conservative or surgical management is required.
Although not a routine practice, if there is difficulty in diagnosing perineal trauma during the puerperium period, ultrasound investigation of the perineum has been shown to be an effective diagnostic tool 13).
Perineum tear treatment
If you had a perineal tear in the area between your vagina and anus (perineum) during delivery, your doctor or midwife will repair it with stitches, using a local anesthetic. An ice pack will be placed against your perineum to ease pain and swelling.
Regardless of the severity of the perineal tear, the following principles should be applied during the repair 14):
- The repair should be completed by an experienced clinician, ideally one trained in obstetrics.
- Good lighting and access are important – ideally, the procedure should be conducted in an operating theatre with the patient in lithotomy.
- Adequate anaesthesia should be used.
- Each layer should be repaired independently to restore function.
- The repair should be conducted in a cephalocaudal (or top-down) direction as this ensures access to superior sites is not restricted.
- Resorbable sutures should be used, with the knots of each layer buried as this reduces the risk of dyspareunia and vaginal discomfort following the recovery.
Recovery from a perineal tear can be uncomfortable or quite painful, depending on how deep and long the incision or tear is. Pain typically affects sitting, walking, urinating, and bowel movements for at least a week. Your first bowel movement may be quite painful. A perineal tear is usually healed in about 4 to 6 weeks.
To reduce pain and promote healing:
- Keep an ice pack on your perineal area. Ask your nurse to apply ice packs right after the birth. Using ice packs in the first 24 hours after birth decreases the swelling and helps with pain.
- Try an anesthetic spray.
- Have regular sitz baths (sit in water that covers your vulvar area) in a tub of warm, shallow water, but wait until 24 hours after you have given birth. Make sure that the bathtub is cleaned with a disinfectant before every bath.
- Take pain medicine. Take medicine like ibuprofen to relieve pain. Some pain medicines can be constipating, so ask your health professional for a formulation that includes a stool softener.
- Take stool softeners and drink lots of fluids to help soften stools and ease pain.
- Use warm water from a squeeze bottle to keep the perineal area clean. Pat it dry with gauze or a sanitary wipe. Only wipe your perineal area from front to back.
Your stitches DO NOT need to be removed. Your body will absorb them. You can return to normal activities when you feel ready, such as light office work or house cleaning. Wait 6 weeks before you:
- Use tampons
- Have sex
- Do any other activity that might rupture (break) the stitches
Self-care
You can do many other things to help speed up the healing process, such as:
- Use sitz baths a few times a day. Wait until 24 hours after you have given birth to take a sitz bath as well. You can buy tubs in any drug store that will fit on the rim of the toilet. If you prefer, you can sit in this kind of tub instead of climbing into the bathtub.
- Change your pads every 2 to 4 hours.
- Keep the area around the stitches clean and dry. Pat the area dry with a clean towel after you bathe.
- After you urinate or have a bowel movement, spray warm water over the area and pat dry with a clean towel or baby wipe. DO NOT use toilet paper.
Take stool softeners and drink lots of water. This will prevent constipation. Eating lots of fiber will also help. Your health care provider can suggest foods with plenty of fiber.
Do Kegel exercises. Squeeze the muscles that you use to hold in urine for 5 minutes. Do this 10 times a day throughout the day.
See your doctor if:
- Your pain gets worse.
- You go for 4 or more days without a bowel movement.
- You pass a blood clot larger than a walnut.
- You have a discharge with a bad odor.
- The wound seems to break open.
Postoperative management
Antibiotics
Broad-spectrum antibiotics are recommended in the immediate postoperative period to reduce the risk of infections and the wound reopened (dehiscence) 15).
Analgesia
Cold packs should be used topically in 10–20 minute intervals in the first 24–72 hours after surgery.26 Paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs) can be used 16). However, limit the use of opioids to reduce the risk of constipation. A urinary alkalinizer can assist in reducing discomfort during toileting 17).
Laxatives or stool softeners
Laxatives are recommended following perineal repair as the passage of stool can result in wound dehiscence 18). Stool softeners (eg lactulose) are recommended for around 10 days postoperatively.29 Stool softeners should be titrated to keep the stools soft but not loose 19).
Positioning and movement
During the first 48 hours after surgery, the patient should use positions that will reduce perineal edema. This involves lying on a flatbed while resting, on their side when breastfeeding, and avoiding the overuse of seated positions 20). The patient should also avoid activities that may increase intra-abdominal pressure for the first six to 12 months after delivery 21).
Pelvic floor exercises
Pelvic floor exercises should be commenced two to three days postpartum, or when the patient feels comfortable 22). Patients with third‑degree or fourth-degree perineal tears should be referred to a physiotherapist who specializes in perineology, as it can reduce flatal, fecal and urinary stress incontinence 23).
Wound care
Ensure that the wound is washed and patted dry after toileting. The patient should inspect the wound daily with the use of a hand mirror for any signs of wound breakdown.
Follow-up
Obstetrician follow-up
Generally, women with obstetric anal sphincter injury repairs are reviewed by the obstetrician six to 12 weeks postpartum 24), when the repair site and anal sphincter tone are assessed.
Family physician follow-up
The role of the general practitioner in the postpartum period will be to titrate the analgaesia and laxative/stool softener requirements to facilitate the woman’s recovery, and to inspect the wound for signs of infection. The major indications for a referral to an obstetrician are:
- wound dehiscence
- severe dyspareunia (painful sex)
- constipation, including:
- excessive straining
- sensation of incomplete emptying
- sensation of anorectal obstruction
- digitation (manual disimpaction)
- faecal incontinence, including:
- urge faecal incontinence
- passive or post-defaecation incontinence.
Perineal tear complications
- Chronic perineal pain
- Dyspareunia (painful sex)
- Fecal incontinence
- Fecal urgency
First and second degree tears rarely cause long-term problems. Among women who experience a third or fourth degree tear, 60-80% are asymptomatic after 12 months 25). Fecal incontinence, faecal urgency, chronic perineal pain and dyspareunia occur in a minority of patients, but may be permanent 26). The symptoms associated with perineal tear are not always due to the tear itself, since there are often other injuries, such as avulsion of pelvic floor muscles, that are not evident on examination 27).
Perineal tear prognosis
- 1st and 2nd degree tears rarely cause long term problems
- In women who’ve experienced a 3rd or 4th degree tear, 70% are asymptomatic after 12 months
- Severe tears can cause significant bleeding, long-term pain, or dysfunction.
Fortunately, first-degree and second-degree perineal lacerations are minor and patients usually recover uneventfully. As third-degree and fourth-degree perineal tears are more extensive, there is an increased likelihood of residual defects resulting in ongoing symptoms that can have a significant impact on the woman’s quality of life. The most common long-term problems are dyspareunia, perineal pain, and flatal and fecal incontinence 28). In fact, obstetric anal sphincter injury are strong risk factors for postponed coital resumption after delivery and dyspareunia at one year postpartum 29). However, anal sphincter competence remains the biggest concern as flatal incontinence can be present even 10 years after obstetric anal sphincter injury 30).. Despite these concerning potential outcomes following obstetric anal sphincter injury, women should be reassured that 60–80% of women are asymptomatic 12 months after a delivery and an external anal sphincter repair 31).
Future deliveries
Women who have sustained obstetric anal sphincter injury in their previous pregnancy should be thoroughly counseled regarding their mode of delivery, with an elective caesarean section being one of the options 32). If the woman chooses a vaginal delivery, it is important to note that there is insufficient evidence for prophylactic episiotomies in the prevention of another obstetric anal sphincter injury, and should thus only be performed if clinically indicated 33).
Resumption of sexual activity
There is currently no evidenced-based research demonstrating the ideal time to resume sexual intercourse following a perineal injury. Thus, the abstinence period is typically determined by the woman during her recovery period. The median time of return to intercourse is six to eight weeks postpartum 34).
Dyspareunia
Dyspareunia or painful sexual intercourse is a common postpartum complaint that must be addressed early because of its impact on the woman’s quality of life (ie physical, relational, psychological wellbeing). The following recommendations can be made 35):
- Lubrication should be used generously during vaginal intercourse.
- The woman should be in control of the initiation of intercourse. If the woman is having difficulty obtaining control, consider having the discussion with the woman and her partner together.
- Experimenting with different sexual positions can facilitate the woman’s comfort.
- Refer to a physiotherapist with a special interest in dyspareunia, or an obstetrician or gynecologist.
References [ + ]