Contents
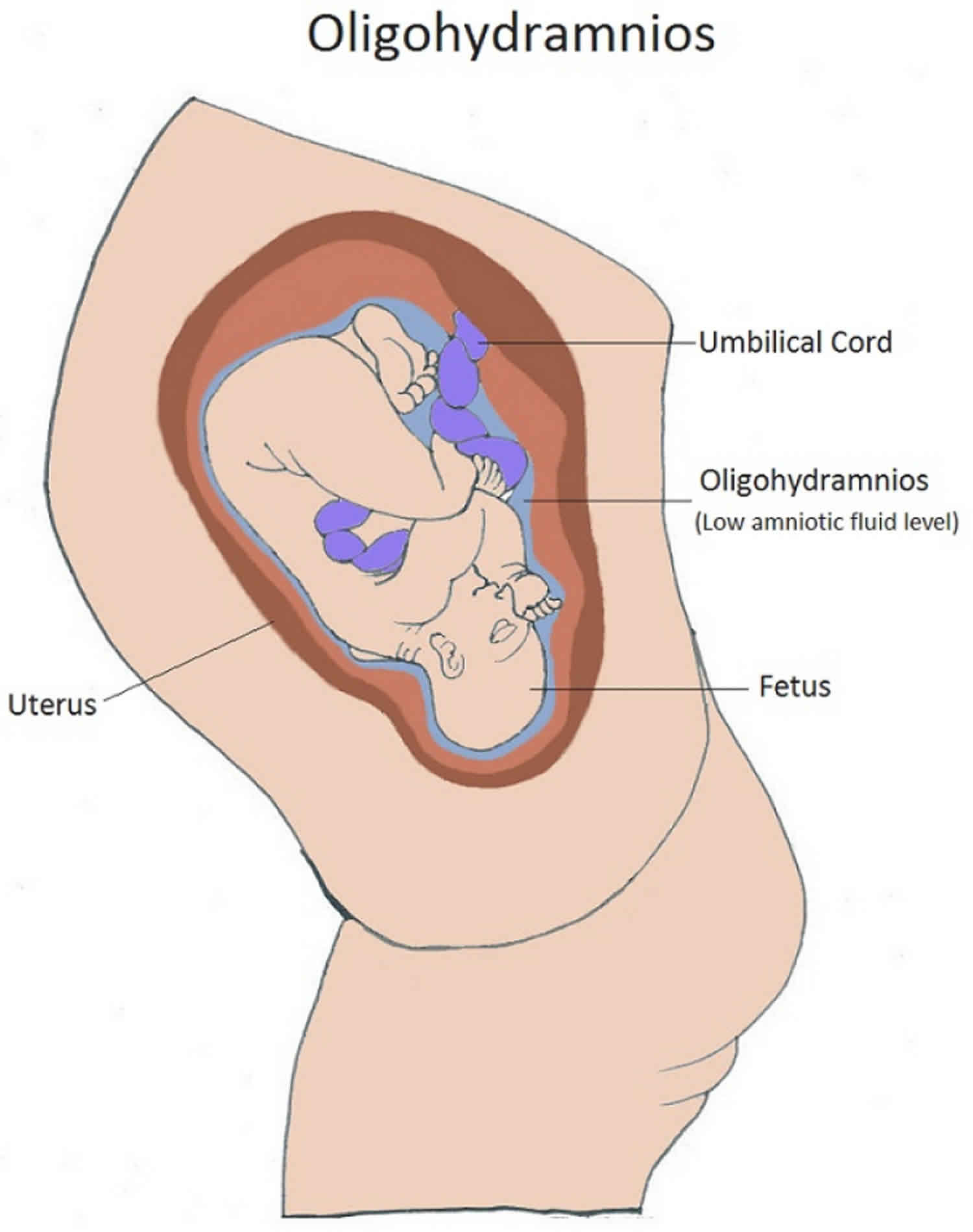
What is oligohydramnios
Oligohydramnios is a condition when you have too little amniotic fluid. Amniotic fluid is the fluid that is contained in the amniotic sac and it surrounds your baby in your uterus (womb). Amniotic fluid is very important for your baby’s development. Oligohydramnios may occur with late pregnancies, ruptured membranes, placental dysfunction, or fetal abnormalities.
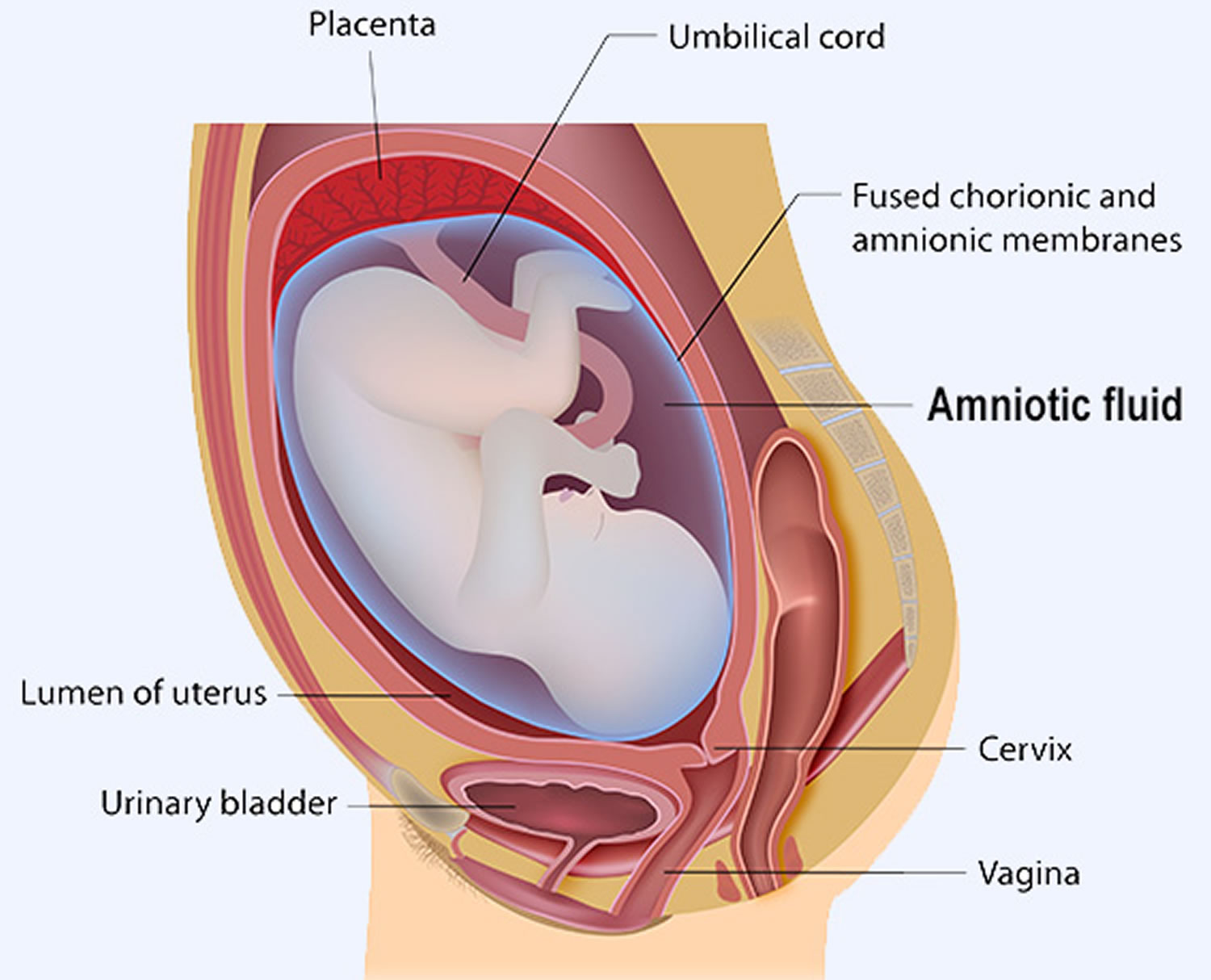
While in the womb, your baby floats in the amniotic fluid. The amount of amniotic fluid is greatest at about 34 weeks (gestation) into the pregnancy, when it averages 800 mL. About 600 mL of amniotic fluid surrounds the baby at full term (40 weeks gestation).
The amniotic fluid constantly moves (circulates) as the baby swallows and “inhales” the fluid, and then releases it.
During pregnancy, amniotic fluid provides a cushion that protects the baby from injury and allows room for growth, movement and development. Amniotic fluid also keeps the umbilical cord from being compressed between the baby and the uterine wall. In addition, the amount of amniotic fluid reflects the baby’s urine output — a measure of a baby’s well-being.
The amniotic fluid helps:
- The developing baby to move in the womb, which allows for proper bone growth
- The lungs to develop properly
- Prevents pressure on the umbilical cord
- Keep a constant temperature around the baby, protecting from heat loss
- Protect the baby from outside injury by cushioning sudden blows or movements
If you have oligohydramnios (low amniotic fluid), what happens next will depend on the cause, severity, your baby’s gestational age, your health and your baby’s health.
Various factors can contribute to oligohydramnios in pregnancy, including:
- Your water breaking
- The placenta peeling away from the inner wall of the uterus — either partially or completely — before delivery (placental abruption)
- Certain health conditions in the mother, such as chronic high blood pressure
- Use of certain medications, such as angiotensin-converting enzyme (ACE) inhibitors
- Certain health conditions in the baby, such as restricted growth or a genetic disorder
If you have oligohydramnios (low amniotic fluid) and you’re 36 to 37 weeks pregnant, the safest treatment might be delivery. If you’re less than 36 weeks pregnant, your doctor will review your baby’s health, discuss why you might have oligohydramnios (low amniotic fluid) and recommend monitoring your pregnancy with fetal ultrasounds. He or she also might recommend drinking more fluids — especially if you’re dehydrated.
If you have oligohydramnios (low amniotic fluid) during labor, your doctor might consider a procedure in which fluid is placed in the amniotic sac (amnioinfusion). This is typically done during labor if there are fetal heart rate abnormalities. Amnioinfusion is done by introducing saline into the amniotic sac through a catheter placed in the cervix during labor.
Oligohydramnios (low amniotic fluid) during pregnancy is a serious condition. If you have any concerns about the amount of fluid around your baby, talk with your health care provider.
Figure 1. Amniotic fluid
How do you know if you have oligohydramnios?
If you notice that you are leaking fluid from your vagina, tell your health care provider. It may be a sign of oligohydramnios. Your provider watches out for other signs, such as if you’re not gaining enough weight or if the baby isn’t growing as fast as he should.
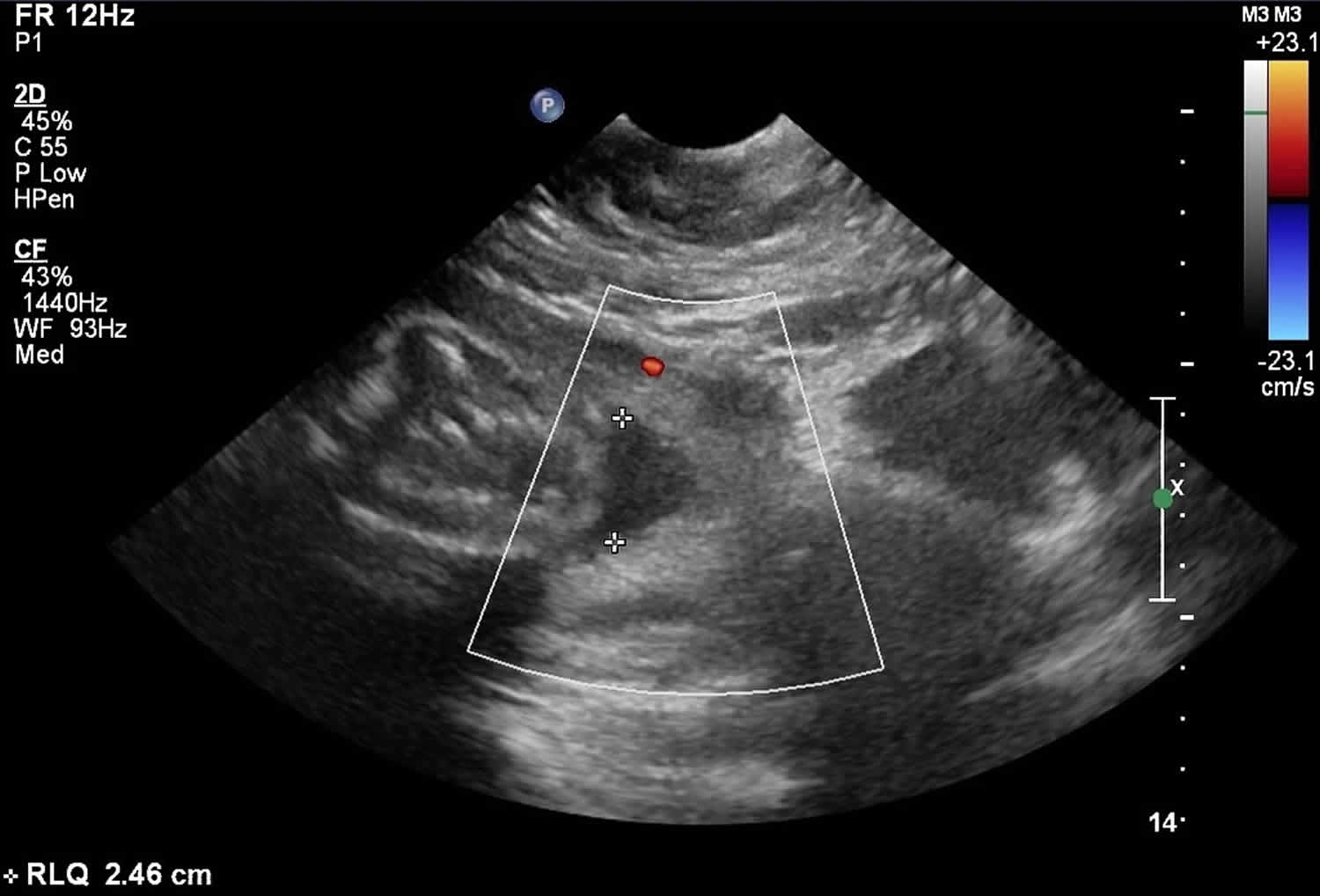
Your health care provider uses ultrasound to measure the amount of amniotic fluid. There are two ways to measure the fluid: amniotic fluid index (AFI) and maximum vertical pocket (MPV).
The amniotic fluid index (AFI) checks how deep the amniotic fluid is in four areas of your uterus. The amniotic fluid index (AFI) is an estimate of the amniotic fluid volume in a pregnant uterus. It is part of the fetal biophysical profile. These amounts are then added up. If your amniotic fluid index (AFI) is less than 5 centimeters, you have oligohydramnios.
The maximum vertical pocket (MPV) measures the deepest area of your uterus to check the amniotic fluid level. If your maximum vertical pocket (MPV) is less than 2 centimeters, you have oligohydramnios.
The deepest (maximal) vertical pocket (MPV) depth is considered a reliable method for assessing amniotic fluid volume on ultrasound 1). It is performed by assessing a pocket of a maximal depth of amniotic fluid which is free of an umbilical cord and fetal parts.
The usually accepted MPV values are:
- MPV <2 cm: indicative of oligohydramnios
- MPV 2-8 cm: normal but should be taken in the context of subjective volume
- MPV >8 cm: indicative of polyhydramnios (although some centers, particularly in Australia, New Zealand and the United Kingdom, use a cut off of >10 cm)
Ask your health provider if you have questions about these measurements.
Figure 2. Oligohydramnios ultrasound
Footnote: Gestation 23+6/40, transverse lie. Estimation of fetal weight <5th percentile and abdominal circumference (AC) on 15th percentile. Amniotic fluid index (AFI) is reduced at 2.5. An AFI < 5-8 is indicative of oligohydramnios. In this case there is also reduced amniotic fluid volume subjectively. The cause in this case was preterm premature rupture of membranes (PPROM).
What causes oligohydramnios
Sometimes the causes of oligohydramnios are not known. Some known causes are:
- Health problems, such as high blood pressure or preexisting diabetes (having too much sugar in the blood before pregnancy)
- Certain medications, like those used to treat high blood pressure – If you have high blood pressure, talk to your provider before getting pregnant to make sure your blood pressure is under control.
- Post-term pregnancy – A pregnancy that goes 2 or more weeks past the due date. A full-term pregnancy is one that lasts 39 to 41 weeks.
- Birth defects, especially ones that affect the baby’s kidneys and urinary tract.
- Premature rupture of the membranes (PROM) – When the amniotic sac breaks after 37 weeks of pregnancy but before labor starts.
A helpful mnemonic for remembering some causes of oligohydramnios is DRIPPC 2):
- D: Demise and drugs (e.g. prostaglandin inhibitors [indomethacin])
- R: Renal abnormalities (decreased urine output)
- renal agenesis
- renal dysplasia
- posterior urethral valves
- polycystic kidneys
- multicystic dysplastic kidney
- urethral atresia
- I: Intrauterine Growth Restriction (IUGR), 80% may occur from decreased renal perfusion due to sparing effect
- P: Premature rupture of membranes
- premature rupture of membranes (PROM)
- preterm premature rupture of membranes (PPROM)
- P: Post-dates. Post dates fetus is when there is prolonged gestation when the fetus remains in-utero beyond 2 weeks beyond expected date of delivery (>42 weeks gestation).
- C: Chromosomal anomalies (especially if other anomalies are found)
- Trisomy 18. Edwards syndrome, also known as trisomy 18 fetuses can have multiple anomalies in multiple systems
- Trisomy 13. Patau syndrome (also known as trisomy 13) is considered the 3rd commonest autosomal trisomy.
- Triploidy. Triploidy is a rare lethal chromosomal (aneupliodic) abnormality caused by the presence of an entire extra chromosomal set.
Associations
- Potter sequence
- Underlying fetal hypoxia and fetal cardiovascular compromise: from preferential flow to the fetal brain at the expense of diminished renal blood flow
- Twin pregnancy-related complications: twin to twin transfusion syndrome: in pump twin
- Maternal dehydration
About 4 out of 100 (4 percent) pregnant women have oligohydramnios. It can happen at any time during pregnancy, but it’s most common in the last trimester (last 3 months). It happens in about 12 out of 100 (12 percent) women whose pregnancies last about 2 weeks past their due dates. This is because the amount of amniotic fluid usually decreases by that time.
Oligohydramnios symptoms
Some of oligohydramnios symptoms may include:
- Fluid leaking from your vagina.
- Your uterus not growing as expected.
- Your baby’s movements slowing down.
Oligohydramnios complications
If oligohydramnios happens in the first 2 trimesters (first 6 months) of pregnancy, it is more likely to cause serious problems than if it happens in the last trimester. These problems can be:
- Birth defects – Problems with a baby’s body that are present at birth
- Miscarriage – When a baby dies in the womb before 20 weeks of pregnancy
- Premature birth – Birth before 37 weeks of pregnancy
- Stillbirth – When a baby dies in the womb after 20 weeks of pregnancy
If oligohydramnios happens in the third trimester of pregnancy, it can cause:
- The baby to grow slowly
- Problems during labor and birth, such as the umbilical cord being squeezed. The umbilical cord carries food and oxygen from the placenta to the baby. If it’s squeezed, the baby doesn’t get enough food and oxygen.
- A greater chance of needing a cesarean section (when your baby is born through a cut the doctor makes in your belly and uterus)
Oligohydramnios diagnosis
Oligohydramnios may be discovered incidentally during routine ultrasonography and noted during antepartum surveillance for other conditions. The diagnosis may be prompted by a lag in sequential fundal height measurements (size less than that expected for the dates) or by fetal parts that are easily palpated through the maternal abdomen 3).
During ultrasonography of the fetal anatomy, normal-appearing fetal kidneys and fluid-filled bladder may be observed to rule out renal agenesis, cystic dysplasia, and ureteral obstruction. Check fetal growth to rule out intrauterine growth restriction (IUGR) leading to oliguria.
Other examinations
MRI and 3-dimensional (3D) ultrasonography are newer (and more expensive) modalities for accurately assessing the amniotic fluid volume 4).
Fetal MRI can complement ultrasonography by providing better visualization in the fetus when ultrasound may be limited, in cases such as severe maternal obesity. Although MRI may offer a larger field of view and better tissue contrast and not be limited by shadowing from osseous structures, it has a limited resolution when compared with ultrasonography and is less readily available and is more expensive 5).
In 35 women with healthy singleton pregnancies, rapid MRI-based projection hydrography measurement was found to be a better predictor of amniotic fluid volume than ultrasonography (in utero at 28-32 weeks’ gestation). For the ultrasound measurements, single deepest vertical pocket (SDVP) measurement related most closely to amniotic fluid volume, with amniotic fluid index (AFI) demonstrating a weaker relationship. Manual multisection planimetry (MSP)-based measurement of amniotic fluid volume was used as a proxy reference standard 6).
Oligohydramnios treatment
If you have a healthy pregnancy and get oligohydramnios near the end of your pregnancy, you probably don’t need treatment. Your provider may want to see you more often. She may want to do ultrasounds weekly or more often to check the amount of amniotic fluid.
Sometimes amnioinfusion can help prevent problems in the baby. Amnioinfusion is when the provider puts a saline solution (salty water) into the uterus through your cervix (the opening to the uterus that sits at the top of your vagina). This treatment can help prevent some problems, such as the umbilical cord being squeezed. If the umbilical cord is squeezed, the baby doesn’t get enough food and oxygen.
If the fluid gets too low or if your baby is having trouble staying healthy, your provider may recommend starting labor early to help prevent problems during labor and birth. However, with regular prenatal care, chances are that your baby will be born healthy.
Drinking lots of water may help increase the amount of amniotic fluid. Your doctor may recommend less physical activity or going on bed rest.
References [ + ]