Contents
- What is neutropenia
- What are neutrophils
- Neutropenia causes
- Neutropenia prevention
- Neutropenia symptoms
- Neutropenia complications
- Neutropenia diagnosis
- Neutropenia treatment
- Neutropenia prognosis
- Febrile neutropenia
- Autoimmune neutropenia
- Congenital neutropenia
- Cyclic neutropenia
What is neutropenia
Neutropenia is when you have a lower than normal number of neutrophils (a type of white blood cells) in your blood. While all white blood cells help your body fight infections, neutrophils play an essential role in immune defenses because they ingest, kill and digest invading microorganisms, including fungi and bacteria 1). Failure to carry out this role leads to immunodeficiency that is mainly characterized by the presence of recurrent infections 2). You probably won’t know that you have neutropenia. People often only find out when they’ve had blood tests done for other reasons.
A single blood test showing low levels of neutrophils doesn’t necessarily mean you have neutropenia. These levels can vary from day to day, so if a blood test shows you have neutropenia, it needs to be repeated for confirmation.
Neutropenia can make you more vulnerable to infections. When neutropenia is severe, even the normal bacteria from your mouth and digestive tract can cause serious illness. You need to take special care to avoid infections when have neutropenia.
The normal count of neutrophils in the blood is between 1,500 and 5,500 neutrophils per microliter (1.5 x 109/L and 5.5 x 109/L) of blood. For children, the cell count indicating neutropenia varies with age. A neutrophil count below 1,000 neutrophils per microliter of blood (1.0 x 109/L) is called neutropenia.
This degree of neutropenia can be “mild” (1.0 – 1.8 x 109/L), “moderate” (0.5 – 1.0 x 109/L), or “severe” (less than 0.5 x 109/L). It should be emphasized, however, that the duration of neutropenia, the function of neutrophils and other host defenses, and the capacity of the bone marrow to respond also contribute considerably to the relative susceptibility of a patient to infection.
Some people have lower-than-average neutrophil counts, but not an increased risk of infection. In these situations their neutropenia isn’t a concern. Neutrophil counts less than 1,000 neutrophils per microliter (1.0 x 109/L) — and especially counts of less than 500 neutrophils per microliter (0.5 – 1.0 x 109/L) — are always considered to be neutropenia, where even the normal bacteria from your mouth and digestive tract can cause serious infections.
If you have neutropenia, you might have no symptoms at all. Some people get bacterial infections on different parts of the body like their skin, mouth area and gums, sinuses or internal organs such as their lungs. Such patients frequently demonstrate mucosal inflammation, particularly of the gingival and perirectal areas and often manifest cellulitis, abscesses, furunculosis, pneumonia or septicemia. Unlike normal individuals, infections in these individuals often lack the fluctuance, induration, and exudate that typically accompany a normal inflammatory response. While superficial infections cause substantial morbidity in these patients, deep-tissue infections of the sinuses, lungs, liver and blood pose the greatest risk. Resistant organisms caused by the repeated use of broad spectrum antibiotics often complicate treatment.
Acquired non-malignant neutropenia occurs much more commonly than chronic neutropenia. In children, the acute forms are most frequently seen in association with viral infection. Neutropenia in this setting usually develops over one to two days and can persist for up to a week without serious sequelae. Since concomitant diminution of other cell lines in this setting is unusual, evaluation for malignancy should be considered if the red cell or platelet compartment are also significantly decreased. In the seriously ill patient – particularly the neonate – sepsis can cause acute Neutropenia. Since such patients can deplete their neutrophil reserves during an overwhelming infection, granulocyte transfusions may be life-saving.
Neutropenia is usually found when your doctor orders tests for a condition you’re already experiencing. It’s rare for neutropenia to be discovered unexpectedly or by chance.
Talk to your doctor about what your test results mean. Neutropenia and results from other tests might indicate the cause of your illness. Or, your doctor may suggest other tests to further check your condition.
Because neutropenia makes you vulnerable to bacterial and fungal infections, your doctor will probably advise certain precautions. These often include wearing a face mask, avoiding anyone with a cold, and washing your hands regularly and thoroughly.
Neutropenia with decreased production with marrow hypoplasia can be primary and due to chronic benign neutropenia, cyclical neutropenia and other congenital and familial neutropenias. It can be secondary to cytotoxic drugs, aplastic anemia, leukemia, drug reactions, and infections. Neutropenia with increased destruction with marrow hyperplasia is due to hypersplenism and immune neutropenia. Secondary causes are the commonest, for example, neutropenia caused as a side effect of chemotherapy for malignancies. Congenital forms are rare and vary in severity, some of them are life-threatening conditions including leukocyte adhesion deficiency, Chediak-Higashi syndrome, hyper-IgE, recurrent infection syndrome, and chronic granulomatous disease 3).
Neutropenia doesn’t cause obvious symptoms, so it alone probably won’t prompt you to go to your doctor. Neutropenia is usually discovered when blood tests are done for other reasons.
Talk to your doctor about what your test results mean. A finding of neutropenia combined with the results from other tests might indicate the cause of your condition. Your doctor also may need to repeat the blood test to confirm your results or order additional tests to find out what’s causing your neutropenia.
If you’ve been diagnosed with neutropenia, call your doctor right away if you develop signs of an infection, which may include:
- Fever above 100.4 degrees F (38 degrees C)
- Chills and sweats
- A new or worsening cough
- Shortness of breath
- A mouth sore
- A sore throat
- Any changes in urination
- A stiff neck
- Diarrhea
- Vomiting
- Redness or swelling around any area where skin is broken or cut
- New vaginal discharge
- New pain
If you have neutropenia, your doctor may recommend measures to lessen your risk of infection, such as staying up to date on vaccinations, washing your hands regularly and thoroughly, wearing a face mask, and avoiding large crowds and anyone with a cold or other contagious illness.
What are neutrophils
Neutrophils also known as neutrophilic granulocytes or polymorphonuclear leukocytes are a type of white blood cells (leukocytes) that normally make up the largest number of circulating white blood cells 4). Neutrophils are considered to be the first line of defense during inflammation and infections. Neutrophils play a crucial role in the immune defense against bacterial and fungal pathogens, and they also participate in the development of the inflammatory reaction 5). Neutrophils move into an area of damaged or infected tissue, where they engulf and destroy bacteria or sometimes fungi. Although neutrophils are mostly viewed as playing a beneficial role to the host, their improper activation may also lead to tissue damage during an autoimmune or exaggerated inflammatory reaction 6).
Neutrophils participate in antimicrobial host defense both as the first line of innate immune defense and as effectors of adaptive immunity. Neutrophils are short-lived cells that usually die while performing their antimicrobial function.
A major wave of discoveries during the 1990s and early 2000s made immunologists begin to appreciate the amazing complexity and sophistication of neutrophil functions 7). It became evident that neutrophils release cytokines and contribute to orchestrating the immune/inflammatory response 8). A highly sophisticated machinery directing neutrophil migration 9) and a surprising complexity of neutrophil granules 10) also begun to emerge. Novel but controversial concepts about how neutrophils may fight microbes, including possible regulation of granule enzyme function by ion fluxes 11) and formation of neutrophil extracellular traps (NETs) 12) were also proposed during that period. Both mechanisms have been subject to intense debate. Nevertheless, all those studies indicated that neutrophils use highly sophisticated and complex mechanisms to perform their role in immune defense and inflammation and led to improved and refined models of neutrophil biology 13) (Figure 1).
Key points
- The neutrophil is one of the body’s main cellular mediators of the destruction of microorganisms, and inevitably damages cells and tissues of the host. Neutrophil-mediated tissue destruction is most often a life-saving process, and the host relies on tissue injury as one of the main sources of information that launches inflammation and immunity.
- Large numbers of immature forms of neutrophils, called neutrophilic band cells, are produced by the bone marrow when the demand is high.
- Neutrophils make important contributions to the recruitment, activation and programming of dendritic cells and macrophages. In turn, the adaptive immune system controls the rate of neutrophil production in the bone marrow.
- Neutrophils have important roles in healing wounds, including sterilization of microorganisms, generation of signals that slow the rate of accumulation of more neutrophils, and instigation of a macrophage-based programme that switches the state of damaged epithelium from pro-inflammatory and nonreplicative, to anti-inflammatory and replicative.
- Neutrophil production is coordinated through cytokine production by adaptive immune cells.
- Neutrophil recruitment to sites of infection involves unique molecular interactions in different tissues.
- Recognition of pathogens by neutrophils involves coordination between a repertoire of cellular receptors.
- Killing of pathogens is achieved through the production of toxic metabolites and the release of nuclear contents.
- Heritable disorders of neutrophils provide key insights into molecular mechanisms of neutrophil function.
- Neutrophils play a central role in coordinating the response of other immune effector cells.
- Pathologic interactions between adaptive immune cells and neutrophils are a major contributor to many autoimmune and inflammatory disease states.
- Neutrophils play both positive and negative roles in cancer progression.
- Neutrophils are short-lived cells that die within a limited time after entering the circulation 14). In the absence of infection or inflammation, they die by a spontaneous apoptosis program 15), likely within 1 day (although some investigators propose this time to be up to 5 days) 16). Inflammatory signals are capable of prolonging the lifespan of the cells by several days, during which they release inflammatory mediators and contribute to the orchestration of the inflammatory response 17).
- Accumulating data showed that neutrophils had a variety of important biological functions in both innate and adaptive immunities, far beyond cytotoxicity against pathogens. Neutrophils can differentially switch phenotypes and display distinct subpopulations under different microenvironments. Neutrophils can produce a large variety of cytokines and chemokines upon stimulation. Furthermore, neutrophils directly interact with dendritic cells (DCs), macrophages, natural killer cells, T cells, and B cells so as to either potentiate or down-modulate both innate and adaptive immunity. In the present review, we summarize the recent progress on the functional plasticity and the regulatory ability on immunity of neutrophils in physiological and pathological situations.
- New pathways of tumor-necrosis factor (TNF) signal transduction in neutrophils are being characterized that open up a new way to think of anti-inflammatory therapy, for example, pathways involving tumor-necrosis factor (TNF)-induced increases in intracellular Ca2+ and the ensuing activation of a non-transmembrane form of adenylyl cyclase, termed soluble adenylyl cyclase.
In addition, neutrophils are also found infiltrating many types of tumors 18). Tumor-associated neutrophils have relevant roles in malignant disease. Indeed neutrophils may be potent antitumor effector cells. However, increasing clinical evidence shows tumor-associated neutrophils correlate with poor prognosis. The tumor microenvironment controls neutrophil recruitment and in turn tumor-associated neutrophils help tumor progression. Hence, tumor-associated neutrophils can be beneficial or detrimental to the host 19).
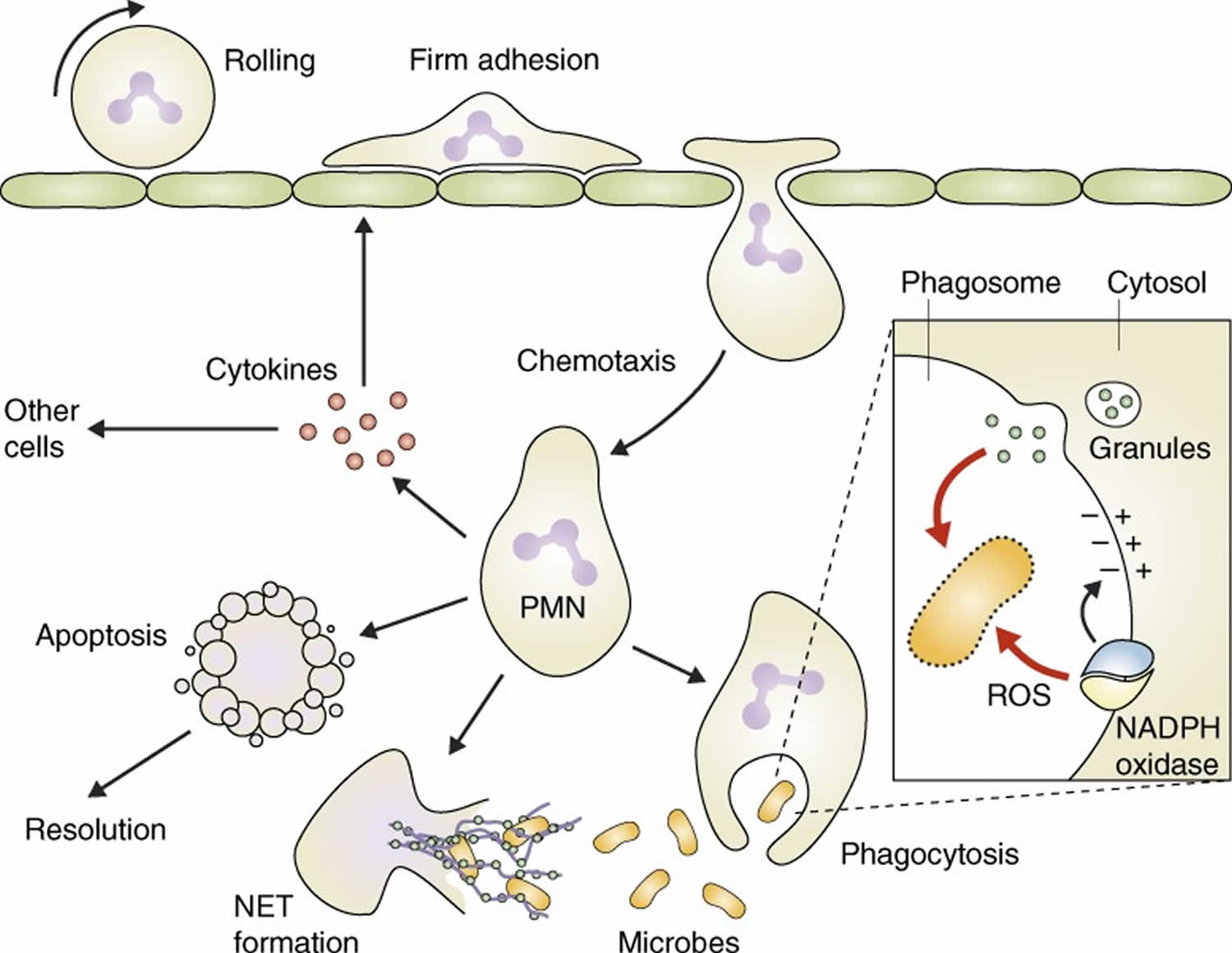
Neutrophils functions
Neutrophils are terminally differentiated cells that develop in the bone marrow where they are also stored for release into the circulation. During their maturation, neutrophils develop several intracellular compartments (secretory granules and vesicles) that store proteins critical for the antimicrobial and proinflammatory missions of the cell 20). Once released into the circulation, neutrophils begin to seek signs of infection and inflammation which lead to a series of events culminating in the migration of neutrophils through the vessel wall and inside the tissue to the site of microbial invasion 21) (see Figure 1).
When encountering infectious particles, neutrophils begin a professional antimicrobial killing program. The infectious particle will be phagocytosed 22) and various noxious agents, including reactive oxygen species generated through the activity of the NADPH oxidase 23), and the contents of intracellular granules 24) are then released into the phagosome, resulting in killing and digestion of the microorganisms (see Figure 1). In cell biology, phagocytosis is the process by which a cell – for example a neutrophil – engulfs a solid particle to form an internal compartment known as a phagosome.
Besides the well-established role of phagocytosis, two additional mechanisms contributing to neutrophil-mediated antimicrobial responses have been proposed during the early 2000s, both of them triggering intensive scrutiny and debate from the scientific community. Segal et al. 25) proposed an interesting molecular interplay whereby ion fluxes triggered by the NADPH oxidase would promote the antimicrobial function of granule proteins. Though many components of the proposed mechanism (such as the electrogenicity of the NADPH oxidase [see Figure 1 inset] providing driving force for other ion currents) are generally accepted, it is still debated whether and to what extent ion fluxes that compensate for the activity of the NADPH oxidase contribute to the antibacterial effects of granule enzymes 26). Another interesting and similarly provocative idea was that, in addition to intraphagosomal killing, neutrophils may also be able to expel their nuclear content (including DNA) complexed with granule proteins into the extracellular space and that this complex, neutrophil extracellular traps (NETs), may inhibit microbial growth without phagocytosis of the pathogen 27). Though neutrophil-derived extracellular DNA has long been known to be present at the site of infection (in part as a component of pus formation) and neutrophil extracellular trap (NET) formation has recently been directly visualized during bacterial infection in vivo 28), the contribution of neutrophil extracellular trap (NET) formation to antibacterial host defense and killing is still under intensive debate 29).
Neutrophils are short-lived cells that die within a limited time after entering the circulation 30). In the absence of infection or inflammation, they die by a spontaneous apoptosis program 31), likely within 1 day (although some investigators propose this time to be up to 5 days) 32). Inflammatory signals are capable of prolonging the lifespan of the cells by several days, during which they release inflammatory mediators and contribute to the orchestration of the inflammatory response 33). However, even under those conditions, neutrophils will soon die by apoptosis (or, possibly, NETosis), contributing to pus formation inside infected tissues. Once neutrophils die, another program for removal of dead neutrophils by macrophages is initiated 34). Parallel to the inflammatory response, biochemical and transcriptional changes leading to the resolution of the inflammation begin 35), and this is further promoted by engulfment of the corpses of dead neutrophils by macrophages 36).
Figure 1. Neutrophils function
Footnotes: After migrating to the site of inflammation, neutrophils (PMN) phagocytose and digest the invading microbes; release neutrophil extracellular traps (NETs), which likely trap bacteria; and produce cytokines, which contribute to the inflammatory reaction. Once infection is cleared, neutrophils die by apoptosis and trigger an active program to resolve inflammation.
Inset: Cytotoxic functions of neutrophils.
Pathogen killing inside the phagosome occurs by reactive oxygen species (ROS) generated by the NADPH oxidase, as well as by granule enzymes released from intracellular granules. The NADPH oxidase also induces depolarization of the phagosomal membrane, which may be required for providing optimal environment inside the phagosome.
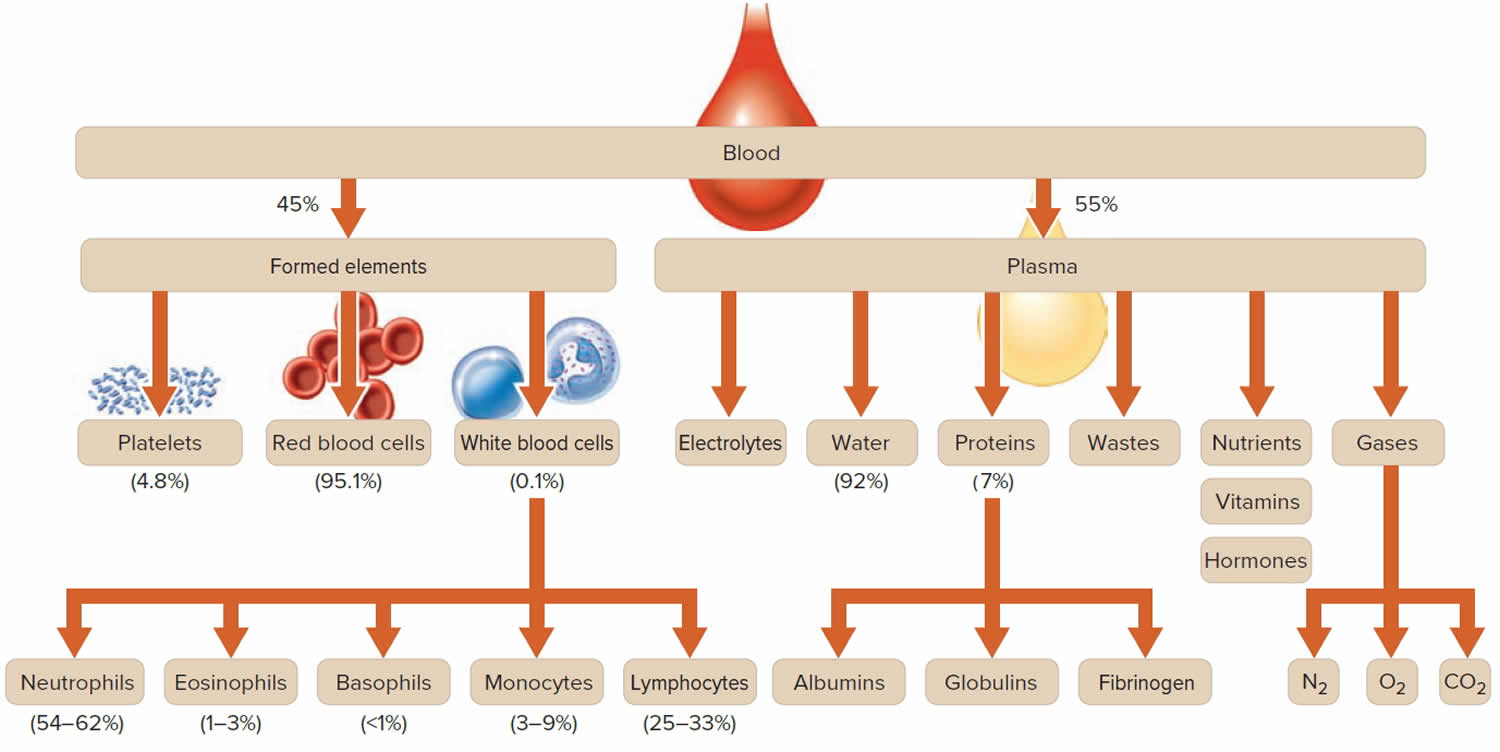
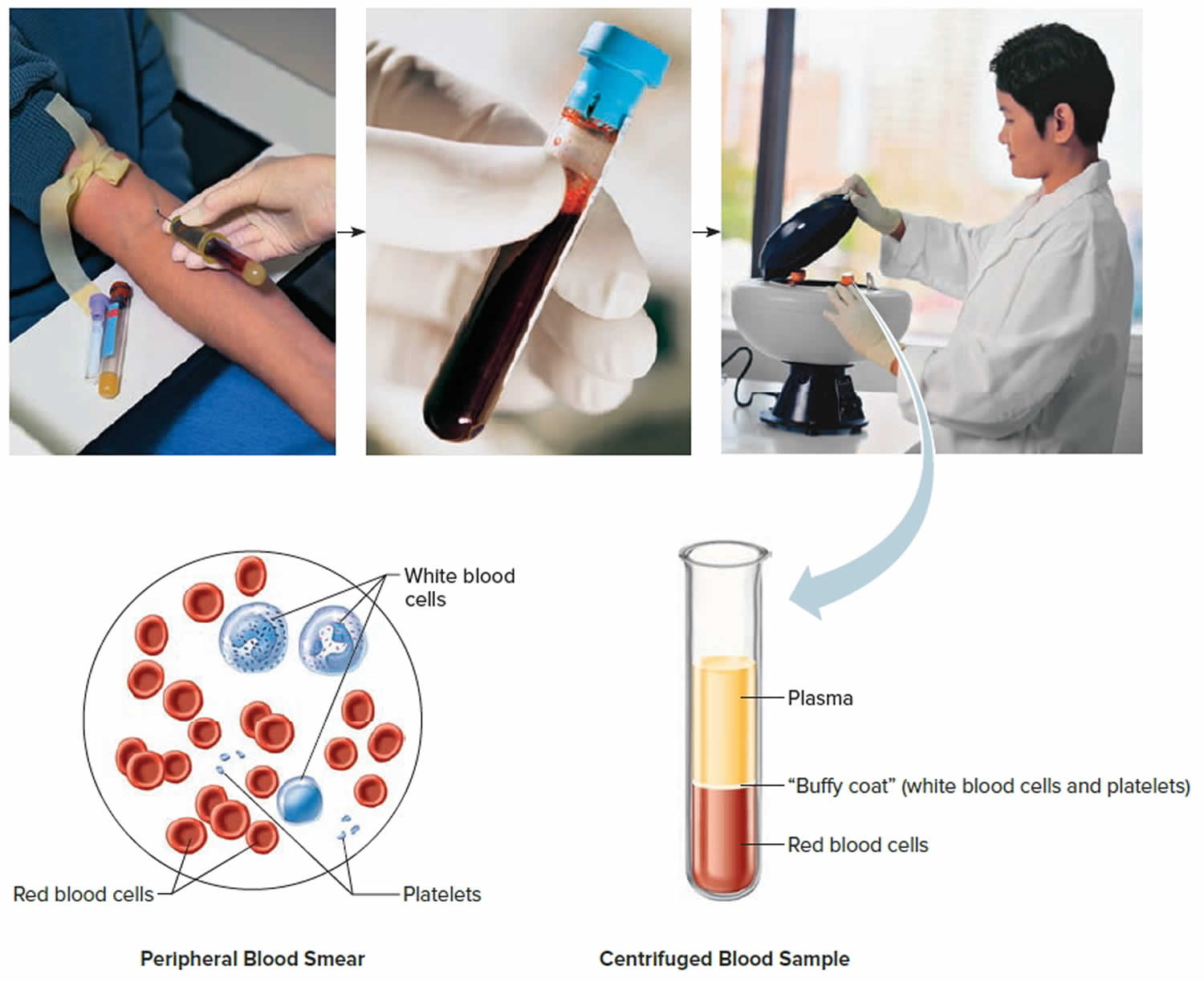
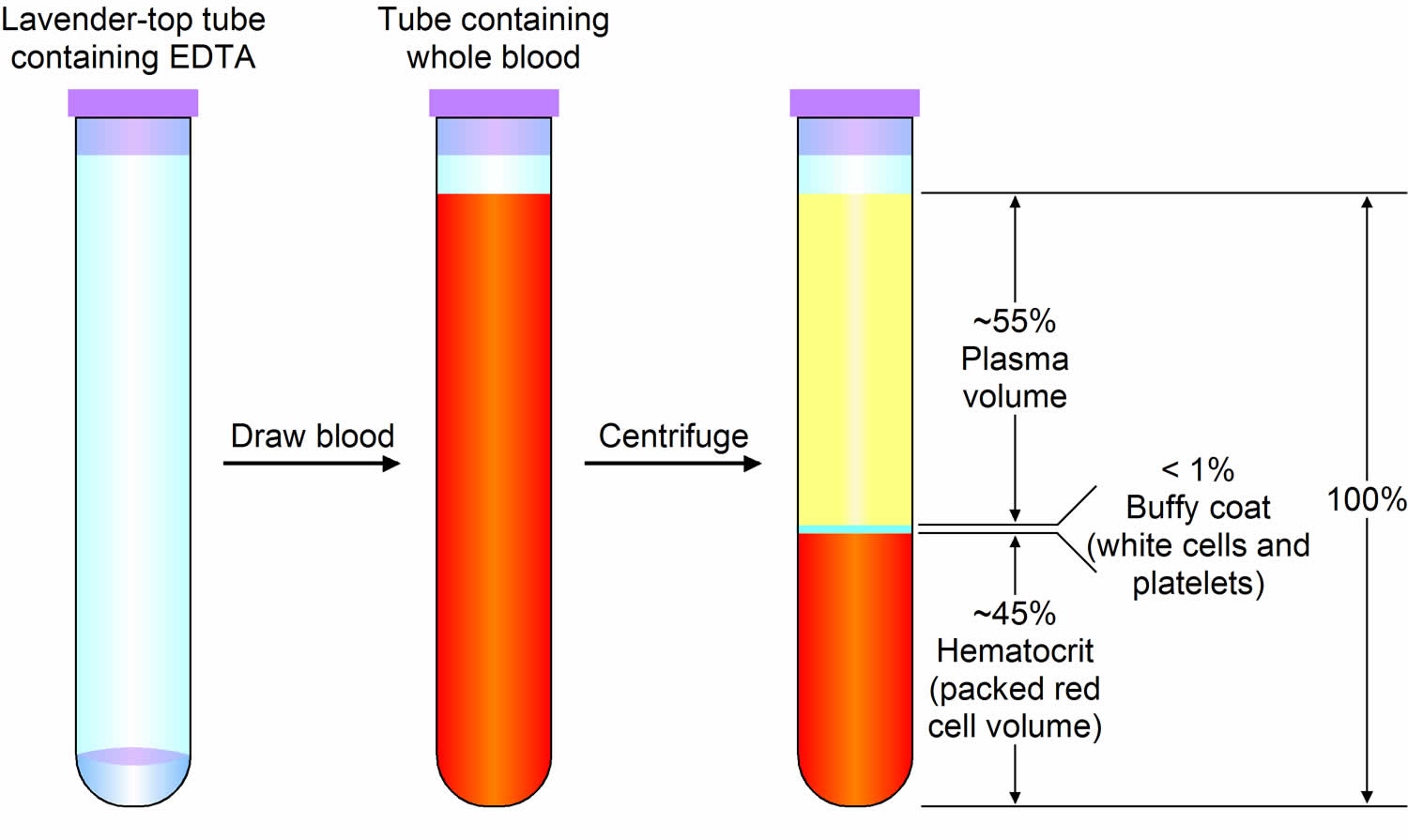
[Source 37)]Figure 2. Blood composition
Blood is a complex mixture of formed elements in a liquid extracellular matrix, called blood plasma. Note that water and proteins account for 99% of the blood plasma.
Note: Blood consists of a liquid portion called plasma and a solid portion (the formed elements) that includes red blood cells, white blood cells, and platelets. When blood components are separated by centrifugation, the white blood cells and platelets form a thin layer, called the “buffy coat,” between the plasma and the red blood cells, which accounts for about 1% of the total blood volume. Blood cells and platelets can be seen under a light microscope when a blood sample is smeared onto a glass slide.
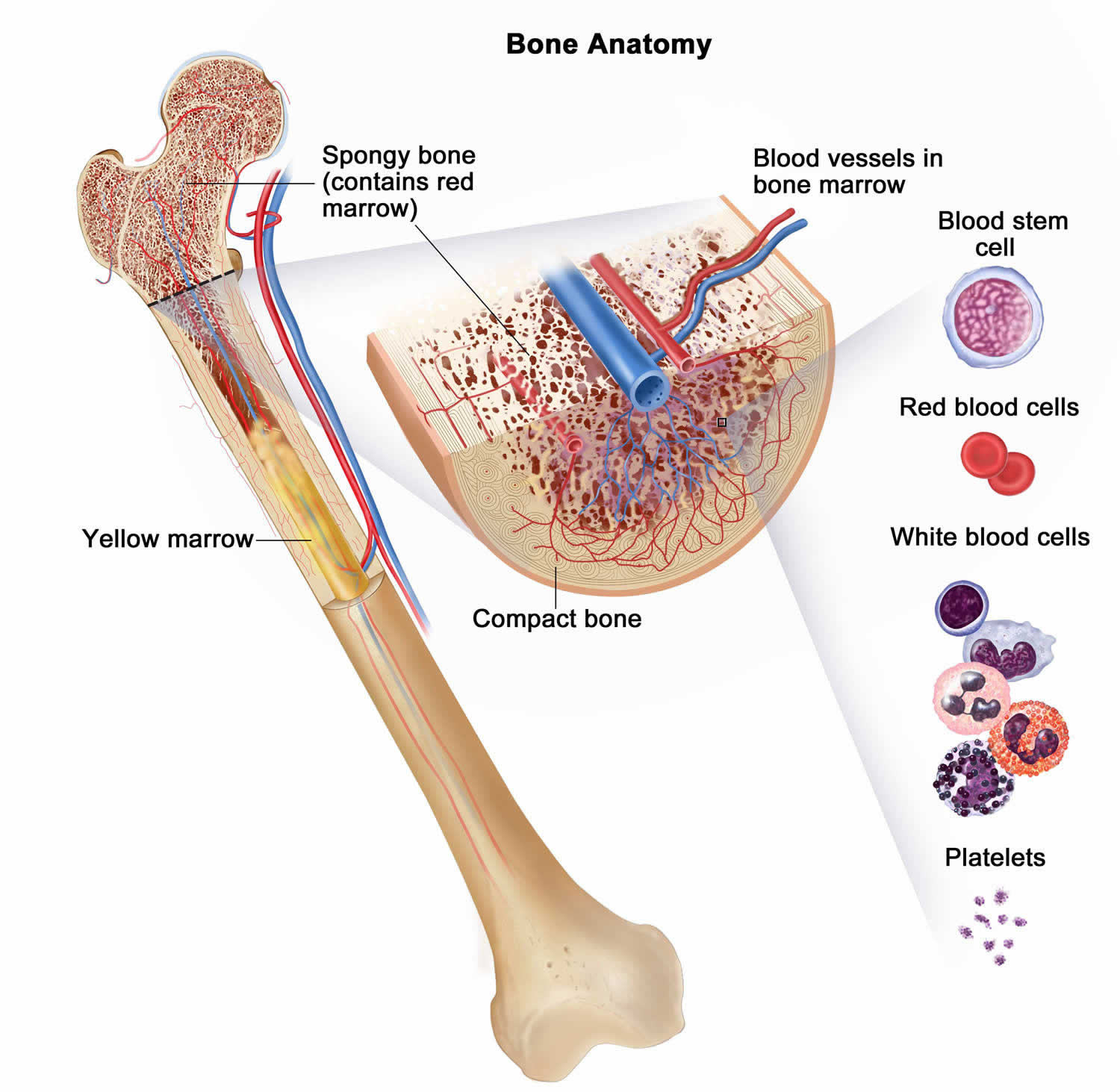
Figure 3. Bone marrow anatomy
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
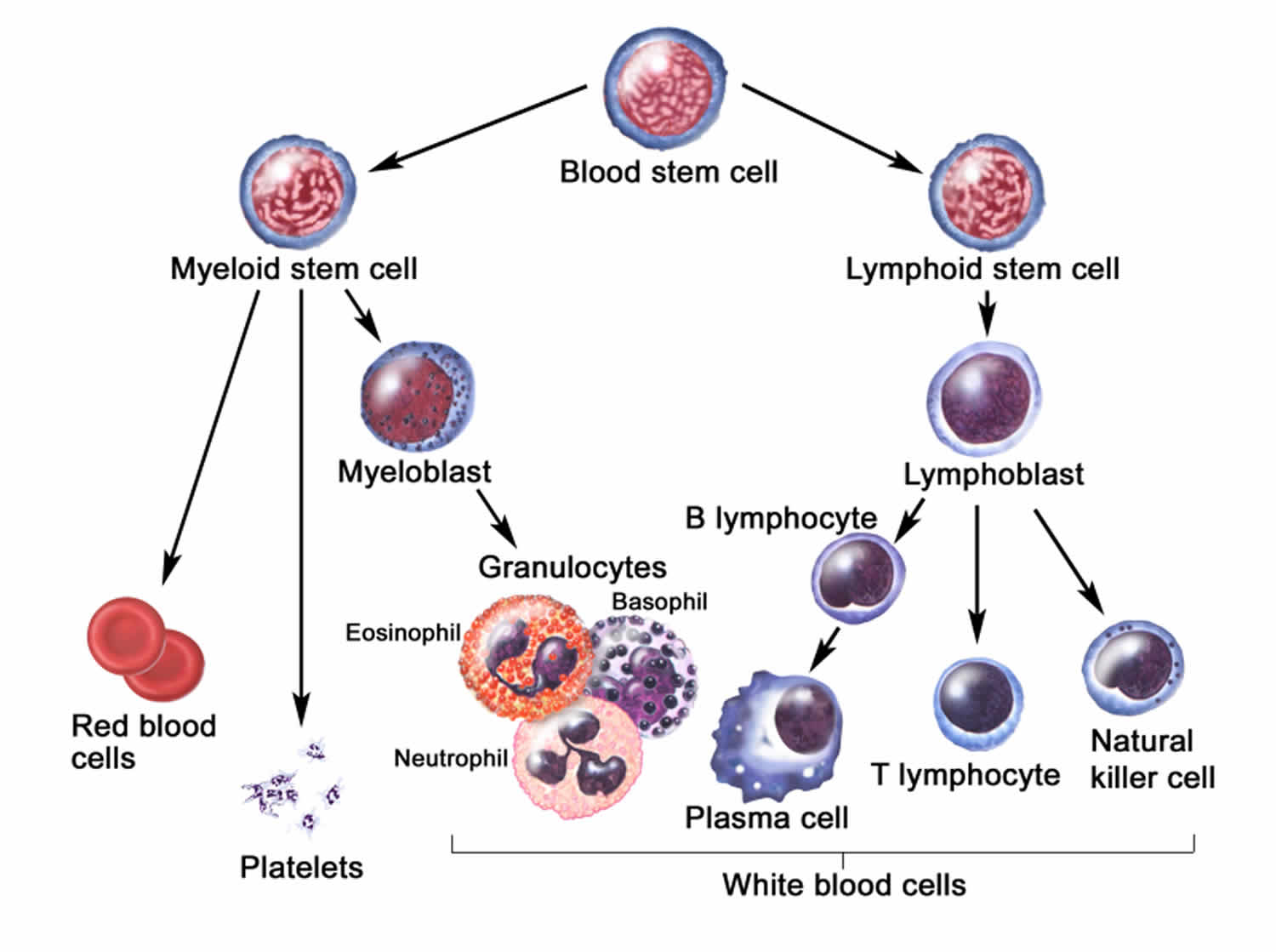
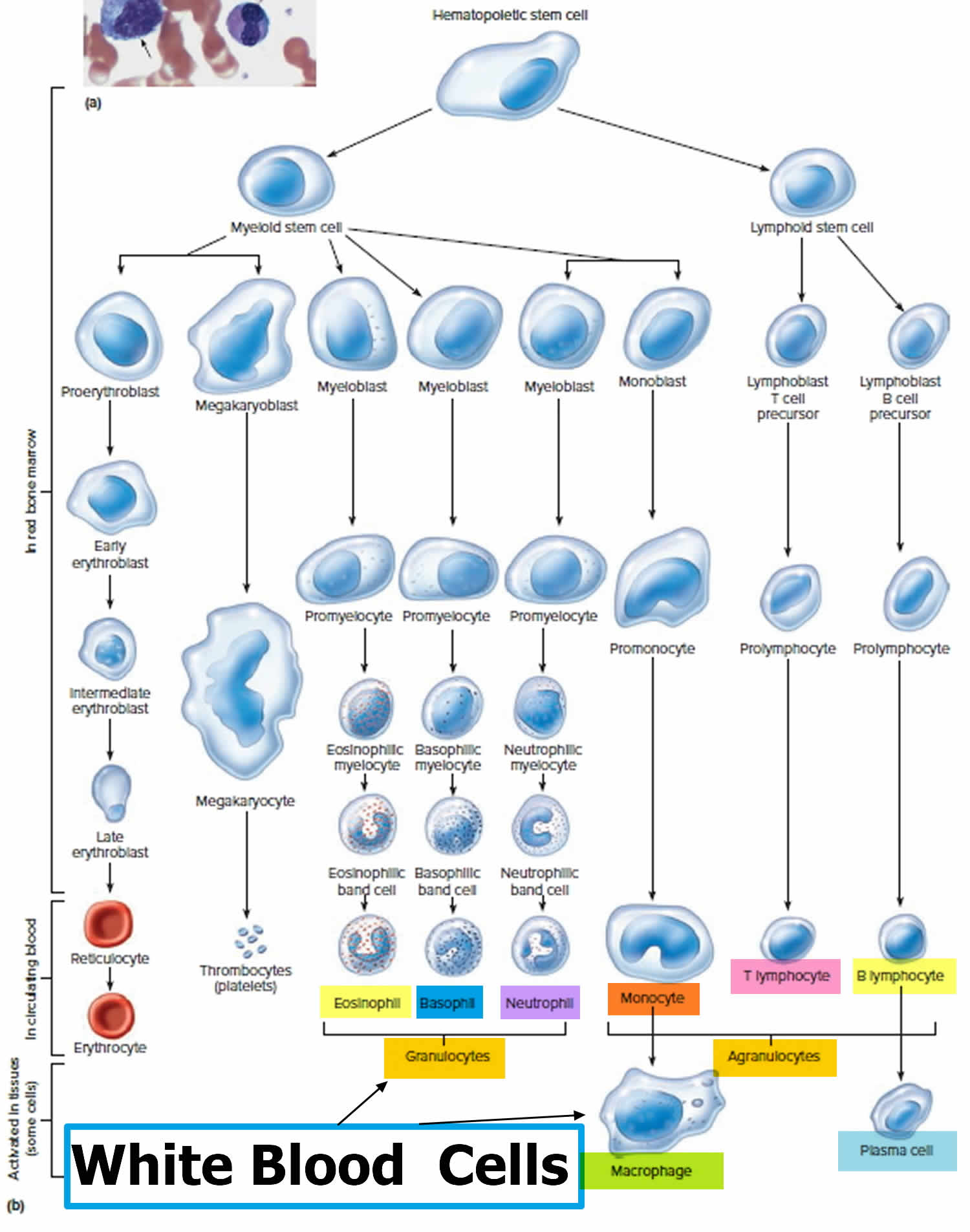
Figure 4. White blood cells development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell
Figure 5. White blood cells development
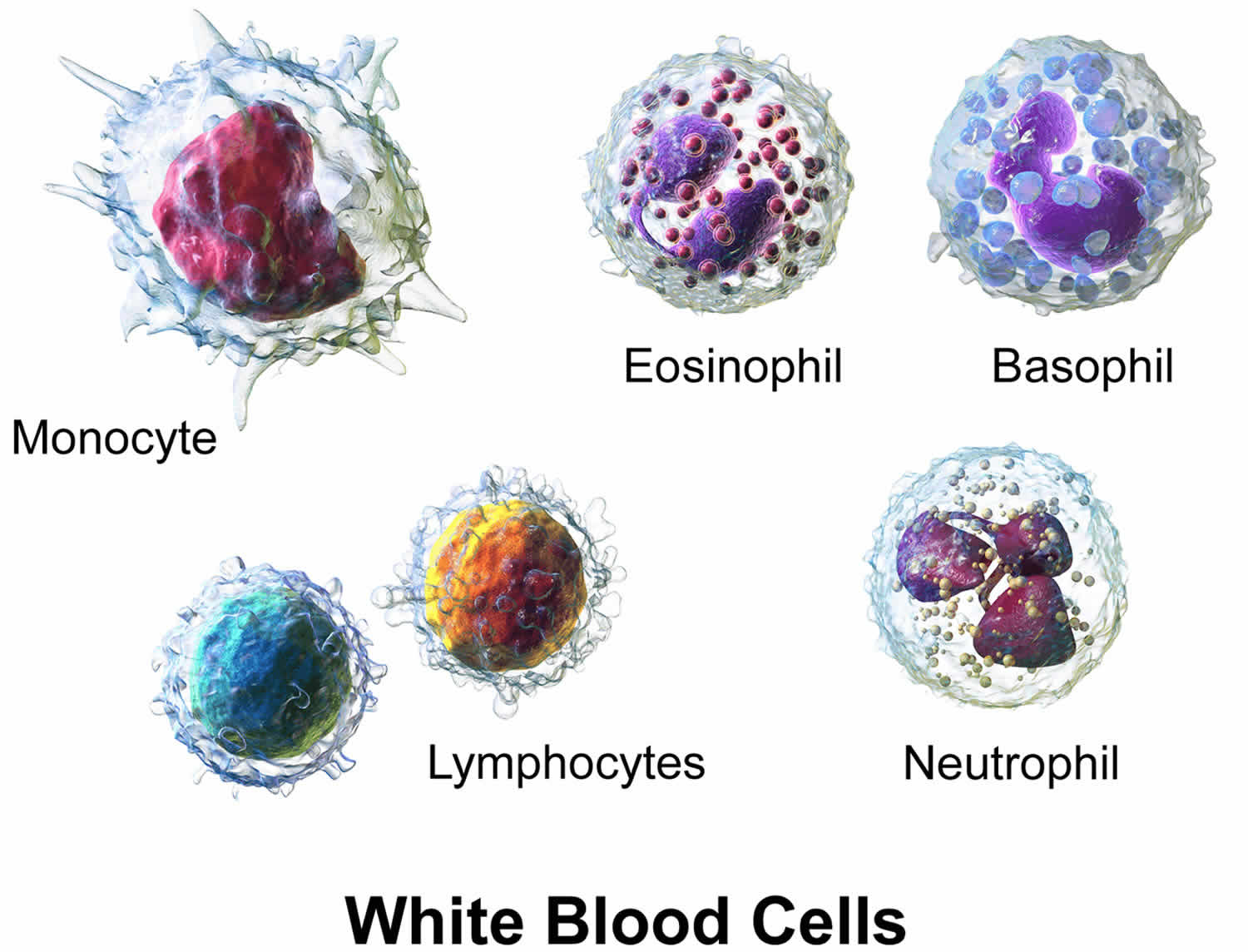
Figure 6. White blood cells
What is neutrophils absolute count
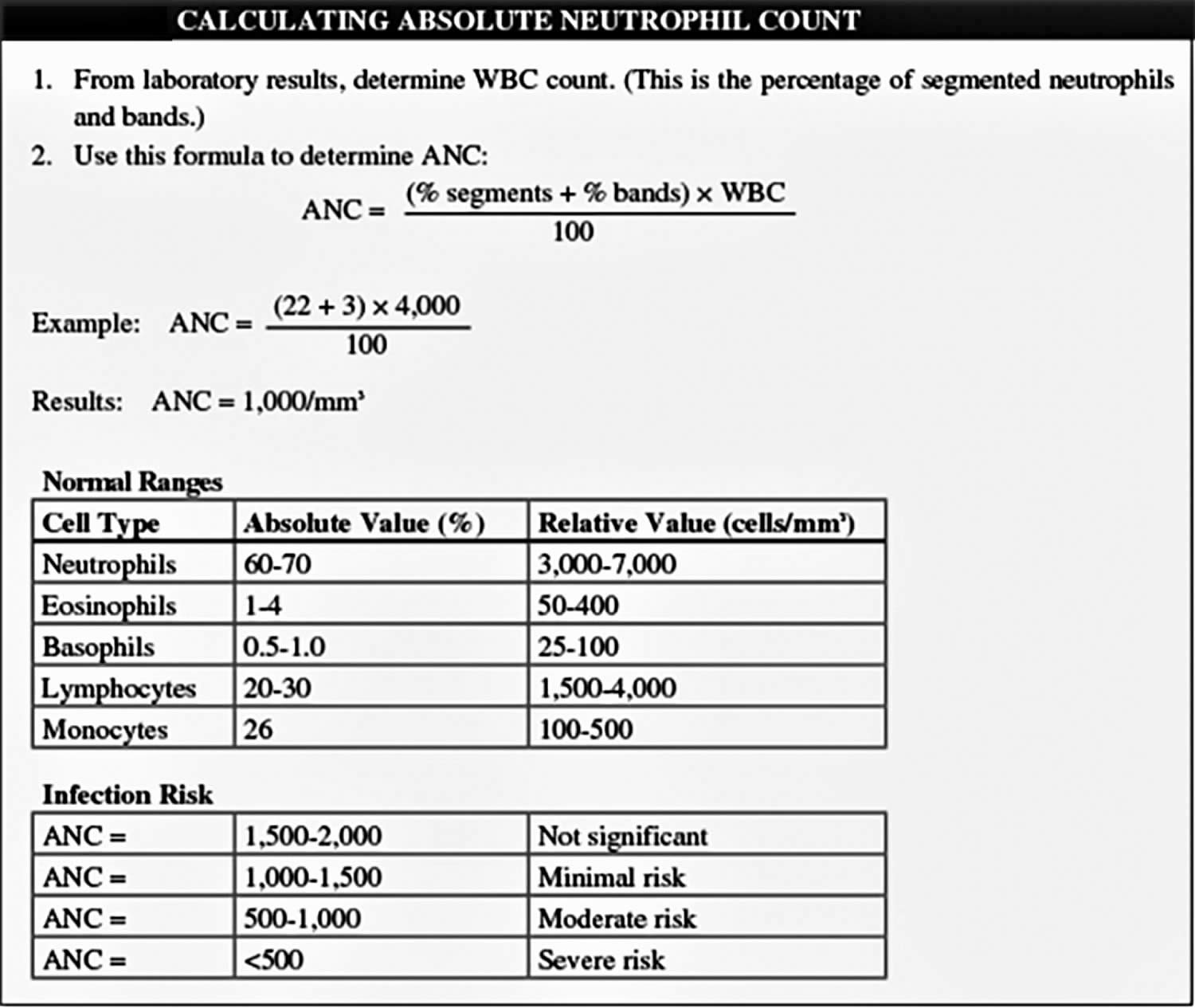
You might hear your doctor or nurse talk about your absolute neutrophil count or ANC. This is the number of neutrophils you have in a certain amount of blood. Your health care team will use your absolute neutrophil count (ANC) to get an idea of how well your immune system might work during treatment. You might want to keep track of your absolute neutrophil count (ANC) so you’ll know when you have a higher risk of getting an infection.
Some labs put this number on your complete blood count (CBC) report, but it isn’t always labeled “ANC,” so you may need to ask your doctor or nurse for help finding it. Sometimes the lab will only report different types of neutrophils as a percentage of white blood cells, and then your health care team will calculate your absolute neutrophil count (ANC). You can also calculate it yourself.
A routine blood smear identifies the five types of white blood cells—neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Neutrophils make up about 55% to 70% of the total white blood cell count. Their primary function is phagocytosis—a process by which they engulf and digest microorganisms and cell fragments.
Acute bacterial infection and trauma stimulate neutrophil production, which elevates the white blood cell count. Significant stimulation of neutrophil production causes immature neutrophil forms, called bands or stab cells, to enter the circulation.
Absolute neutrophil count is an essential monitoring parameter for cancer patients at risk for bone marrow suppression caused by chemotherapy, radiation therapy, or bone marrow transplant. If your patient’s absolute neutrophil count is abnormally low, be sure to practice meticulous hand hygiene—the single most important way to prevent infection in these patients.
Normal and abnormal absolute neutrophil count values
A healthy person has an absolute neutrophil count (ANC) between 2,500 and 6,000/mm³ or per microliter.
The absolute neutrophil count is found by multiplying the white blood cell count by the percent of neutrophils in the blood. For instance, if the white blood cell count is 8,000/mm³ and 50% of the white blood cells are neutrophils, the absolute neutrophil count is 4,000 (8,000 × 0.50 = 4,000).
When the absolute neutrophil count drops below 1,000/mm³ it is called neutropenia. Neutropenia refers to an abnormally low absolute neutrophil count. Your doctor will watch your absolute neutrophil count closely because the risk of infection is much higher when the absolute neutrophil count is below 500. A value above 1,000/mm³ usually means it’s safe to continue chemotherapy. On the other hand, a value below 1,000/mm³ sharply increases the risk of infection.
Figuring out your absolute neutrophil count (ANC)
The numbers for your absolute neutrophil count (ANC) are taken from the results of a blood test called the differential white blood cell (WBC) count. You can ask about the results of your blood tests or get copies of your test results from your doctor or nurse.
To find out your absolute neutrophil count (ANC), multiply the percentage of neutrophils by the total number of white blood cells. Neutrophils are sometimes called segs or polys, and young neutrophils may be called bands on your lab report. If bands are listed as a percentage of white blood cells, add them to the neutrophils before multiplying.
You can figure out your white blood cell using this formula:
- [(% of neutrophils + % of bands) ÷ 100] × white blood cell count = absolute neutrophil count (ANC)
So, for example, if a patient’s white blood cell count is 2,000, with 65% neutrophils and 5% bands, then the ANC is 1,400, which is calculated like this:
- ANC = [(65 + 5) ÷ 100] × 2,000
- ANC = (70 ÷ 100) × 2,000
- ANC = 0.7 × 2,000 = 1,400
An absolute neutrophil count (ANC) of less than 1,000 means that you have neutropenia (a low number of neutrophils) and your immune system is weak. Ask your doctor or nurse to tell you exactly what your numbers mean.
The lower the absolute neutrophil count (ANC) drops and the longer it stays low, the higher your risk of getting a serious infection. If the absolute neutrophil count (ANC) drops below 500 for a few days, you are at a very high risk of getting an infection. If your absolute neutrophil count (ANC) is 100 or less for more than a week, your risk of serious infection is extremely high.
In a person with a healthy immune system, the usual signs of infection are fever, pus, pain, swelling, and redness. As the absolute neutrophil count (ANC) gets lower, many of these signs may not show up when an infection starts. This is because these signs are caused by neutrophils fighting off germs, and you don’t have enough neutrophils to produce the signs. This can make it hard to know if you have an infection. The good thing is that another white blood cell (WBC), called the monocyte, can still cause fever in the person who has neutropenia. In people with severe neutropenia, a fever may be the only sign of an infection.
If your absolute neutrophil count (ANC) is 1,000 or lower and you have a fever of 100.5° F (38° C) or higher when taken by mouth, your doctor will likely assume that you have an infection. Antibiotic treatment is usually started right away, often before the cause of the infection can even be found. Until they can pinpoint the exact bug, doctors learn what they can about the infection to narrow down the treatment options. But they still look for the exact cause so that they can choose the treatment that’s most likely to work – even if it means changing to different antibiotics than what they started with.
Uses of the absolute neutrophil count
Knowing a patient’s absolute neutrophil count has several advantages:
- It reflects the patient’s immunologic status in response to chemotherapy. Myelosuppressive chemotherapy suppresses white blood cell (and thus neutrophil) production, raising the risk of severe infection. A low absolute neutrophil count may indicate the need to delay the next chemotherapy dose or to reduce the dosage.
- The absolute neutrophil count value helps predict subsequent neutropenic events (such as fever) after the first chemotherapy cycle by providing a more accurate picture of immunologic status than the neutrophil or white blood cell count alone.
- It helps the physician determine whether to initiate treatment with growth factors, antibiotics, and other protective measures to decrease the risk of neutropenic complications. For example, administering filgrastim (recombinant methionyl human granulocyte colony-stimulating factor) can shorten neutropenia duration and reduce the risk of febrile neutropenia. This in turn increases the chance that full-dose chemotherapy can be given on time.
- For a hospitalized patient, a low absolute neutrophil count may indicate the need for protective isolation to guard against exposure to infection. For an outpatient, it may indicate the need to avoid crowds and people with colds, runny noses, or influenza.
How to calculate absolute neutrophil count
You can calculate your patient’s absolute neutrophil count in one of two ways.
Figure 7. How to calculate absolute neutrophil count (ANC)
Neutropenia causes
Numerous factors may cause neutropenia through destruction, decreased production or abnormal storage of neutrophils.
Cancer and cancer treatments
Cancer chemotherapy is a common cause of neutropenia. In addition to killing cancer cells, chemotherapy can also destroy neutrophils and other healthy cells.
- Leukemia
- Chemotherapy
- Radiation therapy
Drugs
- Medications used to treat overactive thyroid, such as methimazole (Tapazole) and propylthiouracil
- Certain antibiotics, including vancomycin (Vancocin), penicillin G and oxacillin
- Antiviral drugs, such as ganciclovir (Cytovene) and valganciclovir (Valcyte)
- Anti-inflammatory medication for conditions such as ulcerative colitis or rheumatoid arthritis, including sulfasalazine (Azulfidine)
- Some antipsychotic medications, such as clozapine (Clozaril, Fazaclo, others) and chlorpromazine
- Drugs used to treat irregular heart rhythms, including quinidine and procainamide
- Levamisole — a veterinary drug that’s not approved for human use in the United States, but may be mixed in with cocaine
Infections
- Chickenpox
- Epstein-Barr
- Hepatitis A
- Hepatitis B
- Hepatitis C
- HIV/AIDS
- Measles
- Salmonella infection
- Sepsis (an overwhelming bloodstream infection)
Autoimmune diseases
- Granulomatosis with polyangiitis (formerly called Wegener’s granulomatosis)
- Lupus
- Rheumatoid arthritis
Myeloproliferative neoplasms or myeloproliferative disorders
- Aplastic anemia
- Myelodysplastic syndromes
- Myelofibrosis
Additional causes
- Conditions present at birth, such as Kostmann’s syndrome (a disorder involving low production of neutrophils)
- Unknown reasons, called chronic idiopathic neutropenia
- Vitamin deficiencies
- Abnormalities of the spleen
People can have neutropenia without an increased risk of infection. This is known as benign neutropenia.
Neutropenia prevention
You cannot prevent neutropenia from occurring, but you can decrease your risk of getting an infection while your white blood cell count is low.
Tips to prevent an infection:
- Wash your hands often.
- Clean your teeth and gums with a soft toothbrush, and if your doctor or nurse recommends one, use a mouthwash to prevent mouth sores.
- Shower or bathe daily and use an unscented lotion to prevent your skin from becoming dry and cracked.
- Do not share food, drink cups, utensils or other personal items, such as toothbrushes.
- Try to avoid crowded places and contact with people who are sick.
- Cook meat and eggs all the way through to kill any germs.
- Carefully wash raw fruits and vegetables.
- Try and keep all your household surfaces clean.
- Protect your skin from direct contact with pet bodily waste (urine or faeces) by wearing vinyl or household cleaning gloves when cleaning up after your pet.
- Wash your hands immediately afterwards.
- Use gloves for gardening.
- Get your flu vaccination every year.
Neutropenia symptoms
If you have neutropenia, you might have no symptoms at all. Some people get bacterial infections on different parts of the body like their skin, mouth area and gums, sinuses or internal organs such as their lungs.
Neutropenia is usually found when your doctor orders tests for a condition you’re already experiencing. It’s rare for neutropenia to be discovered unexpectedly or by chance.
Hsieh and collaborators reported that in the United States, the prevalence of neutropenia was 0.38% among Mexican-Americans, 0.79% among whites, and 4.5% among black participants 38). Weycker and collaborators 39) reported that the risk of febrile neutropenia during the chemotherapy regimen course for treating solid tumor was 16.8%. Severe neutropenia was present in 1 of every 2 patients with lymphoma receiving chemotherapy with a higher risk of febrile neutropenia, and it was found in approximately 1 of every 10 breast cancer patients in Spain 40).
Since having neutropenia puts you at increased risk of infection, you may have one or more of these symptoms:
- Fever (temperature over 100.4 °F [38°C])
- Chills or shaking
- Unusual sweating including night sweat
- Sore throat
- Mouth ulcers
- Burning feeling when passing urine; more frequent urination
- Diarrhea.
If you have one or more of the symptoms above, contact your doctor immediately.
People with neutropenia who develop an infection can become seriously ill very quickly. In some cases, this can be life-threatening. Some people who have neutropenia are more at risk of becoming seriously ill than other people. This may be because they have other illnesses as well as their cancer. They may have a more severe infection.
Neutropenia complications
- Recurrent and fatal bacterial and fungal infections 41)
- Bacteremia
- Septic shock
- Premature death
- Failure to thrive
- Protein-energy malnutrition
- Multi-organ failure
Neutropenia diagnosis
In neutropenia there is a history of 42):
- Recurrent infections
- Infections caused by rare bacteria and fungi
- Opportunistic infections
- Frequent use of antibiotics and antifungals
The physical findings include 43):
- Delayed separation of umbilical cord
- Skin infections
- Gingivitis
- Deep abscesses
- Peritonitis
- Osteomyelitis
- Lung abscesses
- Pneumatoceles
- Sinus and lung infections, e.g., pneumonia
- Otitis media
- Meningitis
- Septicemia
- Arthritis
- Bacteremia
- Fever
- Coarse facial features
- Mucocutaneous candidiasis
- Cough
- Malaise
- Intestinal malabsorption
- Bronchiectasis
- Recurrent tonsillitis
- Extensive cutaneous bacterial (Staphylococcal) infections
- Sore throat
- Purulent conjunctivitis
- Granuloma with catalase-positive organisms
- Skin abnormalities, e.g., pyodermitis
- Splenomegaly
- Diarrhea
- Recurrent abscess
- Aphthous stomatitis
- Urinary sepsis
- Vasculitis
- Poor wound healing
The immunological investigation of a patient with neutropenia includes the assessment of immunoglobulins, complement system, and phagocytes 44).
Quantitative Serum Immunoglobulins
- IgG
- IgM
- IgA
- IgE
Blood Lymphocyte Subpopulations
- B lymphocytes (CD19 and CD20)
Phagocytic Function
Nitroblue tetrazolium (NBT) test (before and after stimulation with endotoxin)
- Unstimulated
- Stimulated
Neutrophil mobility
- In medium alone
- In presence of chemoattractant
Complement System Evaluation
Measurement of individuals components by immunoprecipitation tests, ELISA, or Western blotting
- C3 serum levels
- C4 serum levels
Hemolytic assays
- CH50
Complement system functional studies
- Classical pathway assay (using IgM on a microtiter plate)
- Alternative pathway assay (using LPS on a microtiter plate)
- Mannose pathway assay (using mannose on a microtiter plate)
Microbiological studies
- Blood culture
- Urine culture
- Stool culture
- Sputum culture
- Cerebrospinal fluid (culture, chemistry, and histopathology)
Other investigations of immunodeficiency disorders
- Complete blood cell count
- Bone marrow biopsy
- Histopathological studies
- Blood chemistry
- Tumoral markers
- Levels of cytokines (granulocyte-colony stimulating factor)
- Chest x-ray
- Diagnostic ultrasound
- CT scan
- Fluorescent in situ hybridization (FISH)
- DNA testing (for most congenital disorders)
Neutropenia treatment
Application of granulocyte-colony stimulating factor (G-CSF) can improve neutrophil functions and number 45). Prophylactic use of antibiotics and antifungals is reserved for some forms of alteration in neutrophil function such as chronic granulomatous disease) 46). The utilization of antimicrobials is compulsory if recurrent infections exist. Interferon-gamma has been successfully used to improve the quality of life of the patient suffering from neutropenia. Allogenic bone marrow transplantation from an HLA-matched related donor can cure chronic granulomatous disease but has a high mortality rate 47), and gene therapy is also a therapeutic option for treating disorders with neutropenia. Furthermore, intravenous immunoglobulins can be another option in the management of these disorders 48).
Neutropenia prognosis
The prognosis of neutropenia disorders base on the cause and organs involved. Chronic granulomatous disease has a better prognosis if allogenic bone marrow transplantation can successfully achieve. Neutropenia due to chemotherapy or drugs may cause remission once the treatment is over. Some primary defects of neutrophil functions affect the prognosis, where devastating fatal diseases can lead to death in young age 49).
Febrile neutropenia
Febrile neutropenia or neutropenic fever is defined as a single oral temperature of greater than or equal to 101 °F (38.3°C) or a temperature greater than or equal to 100.4 °F (38 °C) for at least an hour, with an absolute neutrophilic count (ANC) of less than 1,500 cells/microliter (1.5 x 109/L) of blood 50). In severe neutropenia, the absolute neutrophilic count (ANC) is less than 500 per microliter (<0.5 x 109/L) or ANC that is expected to decrease below 500 cells/microL (<0.5 x 109/L) in the next 2 hours. In profound neutropenia, the ANC is less than 100 cells/microliter (0.1 x 109/L). To calculate absolute neutrophilic count (ANC), multiply the total white blood cell (WBC) count by the percentage of polymorphonuclear cells and band neutrophils (see ANC calculation and formula above) 51).
Febrile neutropenia is the most common and serious complication associated with hematopoietic cancers or with patients receiving chemotherapeutic regimens for cancer 52). Febrile neutropenia occurs when a neutropenic patient encounters an infectious pathogen. In this immunocompromised state, patients lose or have weakened immunity to fend off infections. The host barriers, such as the mucosal lining of the gastrointestinal tract or sinuses, may be damaged leading the host, open to invasion from an infectious pathogen 53). About 1% of patients undergoing chemotherapy and radiation experience this complication 54).
Despite major advances in prevention and treatment, febrile neutropenia remains one of the most frequent and serious complications of cancer chemotherapy 55). Febrile neutropenia is a major cause of morbidity, healthcare resource use and compromised treatment efficacy resulting from delays and dose reductions of cancer chemotherapy. Mortality from febrile neutropenia has diminished steadily, but remains significant.
The specific frequency of neutropenia is unknown; It could be estimated to be 1.0 to 3.4 cases per million population per year 56). Neutropenia was particularly associated with HIV infection, acute leukemias, and myelodysplastic syndromes. Drug-induced neutropenia has an incidence of one case per million persons per year. About, 50% of patients with febrile neutropenia will develop an infection, of which 20% with profound neutropenia will observe bacteremia 57).
Most standard-dose cancer chemotherapy regimens are associated with 6–8 days of neutropenia, and febrile neutropenia is observed in ∼8 cases per 1000 patients receiving cancer cancer chemotherapy 58). Febrile neutropenia is responsible for considerable morbidity as 20%–30% of patients present complications that require in-hospital management, with an overall in-hospital mortality of ∼10%. The mean cost per hospitalisation in Western countries is ∼€13,500 (US$15 000).
There is a clear relationship between the severity of neutropenia (which directly influences the incidence of febrile neutropenia) and the intensity of cancer chemotherapy. Currently, the different regimens are classified as producing a high risk (>20%), an intermediate risk (10%–20%) or a low risk (<10%) of febrile neutropenia.
It has been shown that several factors, other than cancer chemotherapy itself, are responsible for increasing the risk of febrile neutropenia and its complications. Among them, age plays a major role with older patients having a higher risk of febrile neutropenia following cancer chemotherapy, with worse morbidity and mortality rates. Other factors having a similar role are as follows: The risk of febrile neutropenia and its complications increases when one or several co-morbidities are present in the patient. These considerations will be instrumental in deciding whether a cancer chemotherapy-treated patient should receive primary prophylaxis to decrease the potential risk of febrile neutropenia.
- advanced disease,
- history of prior febrile neutropenia,
- no antibiotic prophylaxis or granulocyte colony-stimulating factor (G-CSF) use,
- mucositis,
- poor performance status and/or
- cardiovascular disease.
In the case of febrile neutropenia, prognosis is worst in patients with proven bacteraemia, with mortality rates of 18% in Gram-negative and 5% in Gram-positive bacteremia [for bacteremias due to coagulase-negative Staphylococcus only, no attributable mortality has been reported] 59). The presence of a focal site of presumed infection (e.g. pneumonia, abscess, cellulitis) also makes the outcome worse. Mortality varies according to the Multinational Association of Supportive Care in Cancer (MASCC) prognostic index (see Table 1 below): lower than 5% if the MASCC score is ≥21, but possibly as high as 40% if the MASCC score is <15 60).
Febrile neutropenia causes
In the majority of cases, the infectious cause is unable to be determined and gets marked as fever of unknown origin (FUO). The definition of fever of unknown origin (FUO) is neutropenic cases with a fever greater than 100.94 °F (38.3°C), without any clinically or microbiologically defined infection 61). Documented infections only comprise approximately 30% of cases. However, infections are the primary cause of morbidity and mortality in patients with cancer who present with fever and neutropenia 62). Majority of infections are bacterial, but viral or fungal etiology is possible 63). Common bacterial pathogens include gram-positive bacteria infections such as Staphylococcus, Streptococcus and Enterococcus species 64). Drug-resistant organisms including Pseudomonas aeruginosa, Acinetobacter species, Stenotrophomonas maltophilia, Escherichia coli and Klebsiella species have also been identified as infectious agents.
Febrile neutropenia diagnosis
A detailed history of the patients presenting illness, chemotherapy treatment, medication use, previous history of infections especially with bacterial resistant organisms and presence of allergies should be noted to guide your therapy 65). Signs of infection may require assessment; Pain and tenderness may be the only indicators of infection. Significant risk factors for the development of febrile neutropenia include older age, comorbidities, the specific type of cancer, and the type and number of myelosuppressive chemotherapy agents in use 66).
Lab tests
Lab tests should be ordered; complete blood count (CBC) to determine patients’ neutropenic level; blood, urinanalysis and throat cultures are needed to determine the source of infection. Two sets of blood cultures should be obtained from a peripheral vein and any venous catheters as well as specimens for testing from any sites of infection, before the immediate administration of empirical broad-spectrum antimicrobial therapy. Urinary tract infections should be suspected in asymptomatic patients with a history of such infections 67). If diarrhea is present a sample may be checked. If the patients have any respiratory symptoms, a chest X-ray is necessary.
Two widely used assessment tools, The Multinational Association for Supportive Care in Cancer (MASCC), and The Clinical Index of the Stable Febrile Neutropenia (CISNE) can be part of the patient interview. These tools can help to risk-stratify patients into high risk and low-risk neutropenic fever.
The Multinational Association for Supportive Care in Cancer (MASCC) was created the assess the risk of serious complications in patients with neutropenic fever. The Multinational Association for Supportive Care in Cancer (MASCC) index has a max score of 26. Patients with a score greater than 21 are considered low risk and patients less than 21 are high risk 68).
Multinational Association for Supportive Care in Cancer (MASCC) Scoring Index
Table 1. Multinational Association for Supportive Care in Cancer (MASCC) febrile neutropaenia risk index
| Characteristics | Score |
|---|---|
| Burden of illness: no or mild symptoms | 5 |
| Burden of illness: moderate symptoms | 3 |
| Burden of illness: severe symptoms | 0 |
| No hypotension (systolic BP > 90 mmHg) | 5 |
| No chronic obstructive pulmonary disease | 4 |
| Solid tumour/lymphoma with no previous fungal infection | 4 |
| No dehydration | 3 |
| Outpatient status (at onset of fever) | 3 |
| Age <60 years | 2 |
Footnote: BP = blood pressure
Characteristic/Score
- The burden of illness: no or mild symptoms/5
- The burden of illness: none or mild/5
- The burden of illness: moderate symptoms/3
- The burden of illness: severe symptoms/0
- No hypotension (systolic BP greater than 90mmHg)/5
- No chronic obstructive pulmonary disease/4
Type of Cancer
- Solid tumor/4
- Lymphoma with previous fungal infection/4
- Hematologic with previous fungal infection/4
- No dehydration/4
- Outpatient status (at the onset of fever)/3
- Age less than 60 years/2
Patients with scores ≥21 are at low risk of complications. Points attributed to the variable ‘burden of illness’ are not cumulative. The maximum theoretical score is therefore 26 69).
The Clinical Index of Stable Febrile Neutropenia Score
A more specific scale for classification of low-risk patients is the Clinical Index of the Stable Febrile Neutropenia (CISNE) and may be more useful in the Emergency Department setting 70). One of the components of the scale is the Eastern Cooperative Oncology Group (ECOG) Performance Status, which helps determines the patient’s functional status as a surrogate for the patient’s ability to undergo therapies in serious illnesses.
The Clinical Index of Stable Febrile Neutropenia Score
Characteristics/Score
- Eastern Cooperative Oncology Group (ECOG) performance status (greater than 2)/2
- COPD/1
- Stree-induced hyperglycemia/2
- Chronic cardiovascular disease/1
- Monocytes less than 200 per mcL/1
- Grade greater than or equal to 2 mucositis/1
- Interpretation
CISNE/Recommendation
- 0-2/Consider outpatient management with oral antibiotics
- Greater than or equal to 3/Inpatient management
Febrile neutropenia treatment
In low-risk patients, oral empiric therapy with a fluoroquinolone plus amoxicillin/clavulanate is recommended in the outpatient setting 71). Clindamycin can be used for those with penicillin allergy. If the patient remains febrile for 48 to 72 hours, the patient will require admission 72).
For high-risk patients presenting with neutropenic fever, an intravenous antibiotic therapy should be given within 1 hour after triage and be monitored more than 4 hours before discharge. The Infectious Disease Society of America (IDSA) recommends monotherapy with antipseudomonal beta-lactam agents such as cefepime, carbapenems or Zosyn 73). Vancomycin is not recommended for initial therapy but should be considered if suspecting catheter-related infection, skin or soft tissue infections pneumonia or hemodynamic instability 74). If patients do not respond to treatments, coverage should be expanded to include resistant species 75):
- Methicillin-resistant Staphylococcus aureus (MRSA): vancomycin, linezolid, and daptomycin
- Vancomycin-resistant enterococci (VRE): linezolid and daptomycin
- Extended Spectrum Beta-Lactamase (ESBL): carbapenems
- Klebsiella pneumonia: carbapenems, polymyxin, colistin, or tigecycline
Recommendation for prevention of infection in neutropenic patients:
- Fluoroquinolones as prophylaxis for patients who are high risk
- Antifungal prophylaxis with an oral triazole with patients with profound neutropenia
- Trimethoprim/sulfamethoxazole (TMP-SMX) is the recommended treatment for patients receiving chemotherapy regimens associated with greater than 3.5% risk for pneumonia from Pneumocystis jirovecii
- Yearly influenza vaccination is recommended for all patients receiving chemotherapy
- Treatment with a nucleoside reverse transcription inhibitor is recommended for patients who are at high risk of hepatitis B virus reactivation
- Herpes simplex virus- seropositive patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT) or leukemia induction therapy should receive prophylaxis
In National Comprehensive Cancer Network guidelines, it is recommended that patients that are at a high risk of febrile neutropenia can benefit from G-CSFs 76).
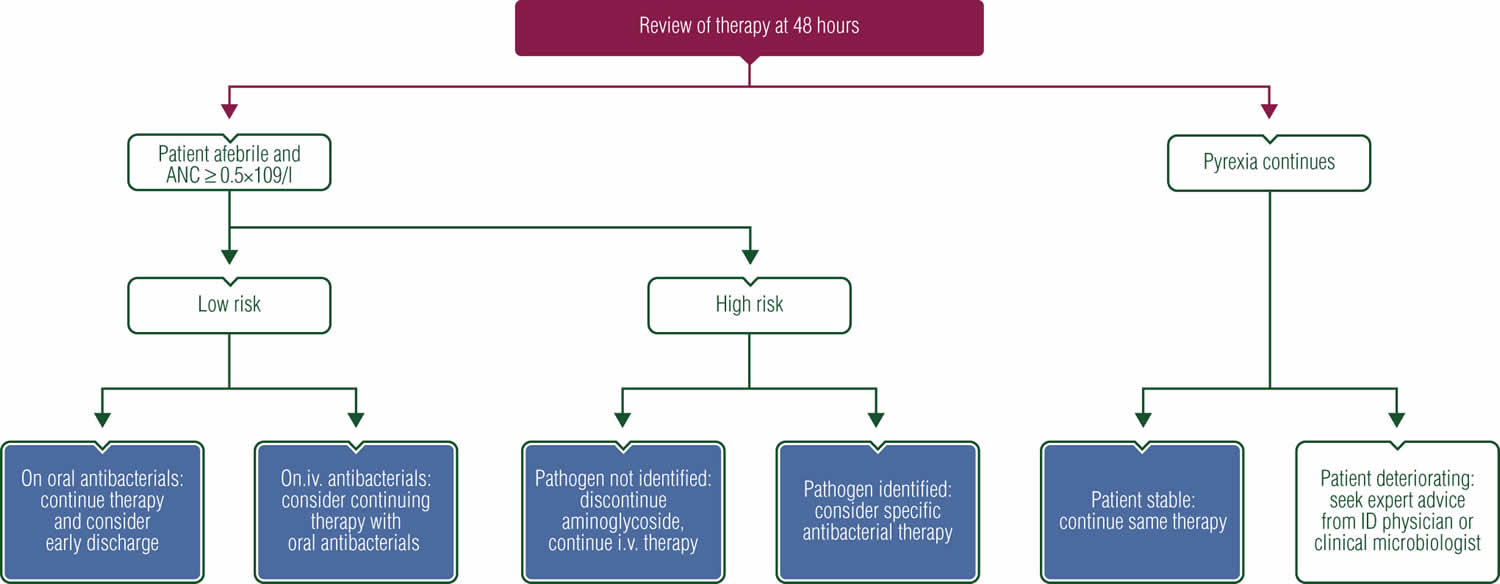
Daily follow-up and assessment of response
The frequency of clinical assessment is determined by severity but may be required every 2–4 hours in cases needing resuscitation. Daily assessment of fever trends, bone marrow and renal function is indicated until the patient is afebrile and has an ANC of ≥500 neutrophils per microliter (≥0.5 x 109/L) of blood (Figure 8) for 24 hours 77). Repeated imaging may be required in patients with persistent pyrexia.
If the patient is afebrile and has an ANC of ≥500 neutrophils per microliter (≥0.5 x 109/L) of blood at 48 hours, has low risk and no cause of infection has been found, consider changing to oral antibiotics. If the patient is at high risk with no cause found and is on dual therapy, aminoglycoside may be discontinued. When the cause is found, continue on appropriate specific therapy 78).
If the patient is still febrile at 48 hours, but clinically stable, initial antibacterial therapy should be continued. If the patient is clinically unstable, antibacterial therapy should be rotated or broadened if clinical developments justify this. Some haematology units will add a glycopeptide to the regimen, while other centres will change the regimen to imipenem or meropenem and a glycopeptide. This group of patients with persistent fever is at a high risk of serious complications, and prompt advice from an ID physician or clinical microbiologist should be sought. Unusual infections should be considered, particularly in the context of a rising C-reactive protein, with a view to proceeding to imaging of the chest and upper abdomen, to exclude probable fungal or yeast infection, or abscesses. When the pyrexia lasts for >4–6 days, empirical initiation of antifungal therapy may be needed 79).
Duration of therapy
If the ANC is ≥500 neutrophils per microliter (≥0.5 x 109/L) of blood, the patient is asymptomatic and has been afebrile for 48 hours and blood cultures are negative, antibacterials can be discontinued 80).
If the ANC is ≤500 neutrophils per microliter (≤0.5 x 109/L) of blood, the patient has suffered no complications and has been afebrile for 5–7 days, antibacterials can be discontinued except in certain high-risk cases with acute leukaemia and following high-dose cancer chemotherapy when antibacterials are often continued for up to 10 days, or until the ANC is ≥500 neutrophils per microliter (≥0.5 x 109/L) of blood 81).
Patients with persistent fever despite neutrophil recovery should be assessed by an infectious disease physician or clinical microbiologist and antifungal therapy considered 82).
An overall algorithm for the assessment of response and subsequent management is proposed in Figure 8.
Figure 8. Febrile neutropenia assessment of response and subsequent management
[Source 83) ]Febrile neutropenia guidelines
Key recommendations for the management of febrile neutropenia 84)
- Febrile neutropenia is observed in ±1% of patients receiving cancer chemotherapy; it is associated with considerable morbidity (20%–30%) and mortality (10%)
- Febrile neutropenia can be effectively prevented by the use of granulocyte colony-stimulating factors (G-CSFs); it is recommended to use these agents in patients receiving chemotherapies with a >20% risk of developing febrile neutropenia and in those having serious co-morbidities and/or aged >60 years
- Patients with febrile neutropenia should be assessed for the risk of complications using a validated predictive tool, such as the Multinational Association of Supportive Care in Cancer (MASCC) score
- Patients with febrile neutropenia at a low risk of complications can often be treated with oral antibiotics and possibly as outpatients, if adequate follow-up is available
- Patients with febrile neutropenia at a high risk of complications should be hospitalised and treated without delay with broad spectrum antibiotics; these patients should be closely monitored for instability (pre-shock)
Specific indications for alternative therapy
Apart from the standard treatment with broad-spectrum antibacterial agents, there are a number of situations, in clinical practice, that require a specific regimen. The duration of treatment may vary and local antibacterial guidelines should be followed in these circumstances.
Central I.V. catheters
If a patient has an I.V. catheter, catheter-related infection (CRI) should be suspected, and blood must be cultured from the catheter and peripherally to measure the differential time to positivity (DTTP), which is the difference in time between positivity of results between catheter culture and peripheral blood culture. A differential time to positivity of ±2 h is a highly sensitive and specific indicator of catheter-related bacteraemia 85).
All cases of catheter-related infection in the setting of febrile neutropenia require decision-making on the choice and duration of i.v. antibiotics, and the need for catheter removal. When catheter-related infection is suspected, and the patient is stable, the catheter should not be removed without microbiological evidence of infection 86).
A glycopeptide such as vancomycin should be administered through the line when possible to cover Gram-positive organisms. Teicoplanin is a useful alternative as it can be administered once daily as a line lock. Success in treating catheter-related infection without removing the catheter depends on the pathogen isolated in the blood cultures.
In catheter-related infection due to coagulase-negative Staphylococcus, an attempt at preserving the catheter can be made if the patient is stable. Catheter retention does not have an impact on the resolution of coagulase-negative Staphylococcus bacteraemia but is a significant risk factor for recurrence in those patients in whom the catheter was retained.
Removal of the line is indicated in the context of tunnel infections, pocket infections (implanted port system), persistent bacteraemia despite adequate treatment, atypical mycobacterial infection and candidaemia. With regard to line infections caused by Staphylococcus aureus, the literature is divided. The desire to preserve the line must be balanced against the risk of metastatic spread by bloodstream seeding. The recommendation should be to remove the line if at all possible, while recognising that, with careful management, it might be possible to maintain it for a short period. Persistent fever and bacteremia despite appropriate antibiotics are indications for line removal.
Pneumonia
If pneumonia in an outpatient is diagnosed either on clinical grounds and/or on the basis of radiological imaging, antibiotic cover may be extended to treat atypical organisms such as Legionella and Mycoplasma by adding a macrolide or a fluoroquinolone antibiotic to a β-lactam antibiotic. Consideration for infection with Pneumocystis jirovecii should be given in patients who present with high respiratory rates and/or desaturate readily off oxygen or on minimal exertion. Predisposing factors include prior corticosteroid therapy, use of immune suppressants after organ transplantation and exposure to purine analogues, as well as lack of reliable chemoprophylaxis with co-trimoxazole 87). In high-risk patients with profound prolonged neutropaenia and lung infiltrates, early treatment with a mould-active antifungal agent is recommended.
Lung infiltrates
Patients with AML during remission induction ChT and those undergoing allogeneic haematopoietic stem cell transplantation with prior conditioning cancer chemotherapy are at risk of invasive fungal infections (namely aspergillosis) due to prolonged and profound neutropaenia 88). Frequent assessment of initial response to antibacterial therapy is essential, and, in the absence of prompt improvement, further investigations are warranted. If invasive aspergillus is suspected, a high-resolution chest computed tomography (CT) scan should be carried out on the same day, looking for typical features such as nodules with halos or ground-glass change, and galactomannan should be measured in serum. If any infiltrate is found, bronchoalveolar lavage should be undertaken if possible.
Advice from an infectious diseases specialist or clinical microbiologist is recommended, and an appropriate therapy against infection with fungi or Pneumocystis species should be instituted. The choice of antifungal agents will depend on centres, individual patients and use of prior prophylactic therapy 89).
Therapy for presumed aspergillosis (for cases with typical infiltrates on CT) could consist of either voriconazole or liposomal amphotericin B 90). These antifungals can be combined with an echinocandin in unresponsive disease. A precise microbiological diagnosis is highly desirable in patients suspected of invasive fungal infection, as the sensitivity to various antifungal agents is variable among different species.
High-dose co-trimoxazole is the treatment of choice for suspected Pneumocystis infection.
After appropriate samples are taken, therapy with aciclovir should be initiated. Ganciclovir (or foscarnet) should be substituted only when there is a high suspicion of invasive cytomegalovirus infection 91).
Suspected meningitis or encephalitis
Lumbar puncture (if in any way possible before the institution of antibiotics) is mandatory in these rare cases. Bacterial meningitis should be treated with ceftazidime plus ampicillin (to cover for Listeria monocytogenes) or meropenem. Viral encephalitis is treated with a high dose of aciclovir.
Cellulitis
The addition of vancomycin broadens the cover against skin pathogens. Linezolid and daptomycin are emerging alternatives to glycopeptides; however, more clinical experience is needed, especially in neutropaenic patients.
Intra-abdominal or pelvic sepsis
If clinical or microbiological evidence of intra-abdominal or pelvic sepsis exists, metronidazole should be commenced, unless the patient is on a carbapenem or piperacillin–tazobactam, which have adequate anaerobic coverage.
Diarrhea
Assessment for Clostridium difficile is needed and, if suspected, oral vancomycin or metronidazole treatment should be administered.
Candidiasis
Patients at risk of disseminated candidiasis are those with prolonged neutropaenia and especially those with haematological malignancies undergoing myeloablative therapy 92). Candidaemia can be diagnosed on blood culture; however, cultures may take several days to become positive. Empirical initiation of antifungal therapy is recommended in patients whose fever fails to respond to broad-spectrum antibiotics after 3–7 days of appropriate treatment. A CT scan of the liver and spleen should be carried out before commencing anti-Candida treatment, looking for typical changes.
First-line empirical treatment depends on what is known about the patient. Liposomal amphotericin B and an echinocandin antifungal such as caspofungin are appropriate first-line treatments if the patient has already been exposed to an azole or if the patient is known to be colonised with non-albicans Candida. Fluconazole can be given first line provided the patient is at low risk of invasive aspergillosis; local epidemiological data suggest low rates of azole-resistant isolates of Candida and the patient has not received an azole antifungal as prophylaxis. Once begun, antifungal treatment should be continued until neutropaenia has resolved, or for at least 14 days in patients with a demonstrated invasive Candida infection.
Specific needs for preventing other opportunistic infections are required in patients with haematological malignancies, namely those undergoing haematopoietic stem cell transplants 93).
Autoimmune neutropenia
Autoimmune neutropenia involves neutrophil-specific antibodies in the blood that actually attack the body’s own neutrophils. Severe acute neutropenia discovered in older children and adults unassociated with an acute viral syndrome may represent autoimmune neutropenia. However, demonstration of neutrophil antibodies is required to differentiate autoimmune neutropenia from benign chronic idiopathic neutropenia. Presence of neutrophil-specific antibodies can result in increased destruction of the body’s own blood neutrophils. Physical examination in these patients is usually unremarkable, but occasionally splenomegaly is noted. Marrow finding generally reflect that of “bone marrow arrest” – where adeuate numbers of early myeloid cells can be identified, but more mature myeloid elements appear lacking. The level of this “arrest” seems to vary between patients, and may reflect patient variability with regard to the myeloid antigen (early versus late) target by autoantibodies. Since young patients with autoimmune neutropenia are likely to have a relatively benign course, most do not appear to require treatment of any kind. In some children where severe infections occur, treatment with G-CSF is indicated. In most children the blood counts normalize during the first 2 – 3 years. In patients with recurrent infections, treatment with corticosteroids results in improved neutrophil counts in about half of patients. The majority of patients less than 2 years of age spontaneously achieve a durable remission within 3 years of their initial diagnosis. In contrast, adults and children over the age of 2 tend to have accompanying immunologic abnormalities and appear less likely to improve spontaneously over time. Similarly, older patients appear more resistant to therapeutic interventions including corticosteroids, intravenous immune globulin, and splenectomy. Two patients have acheived clinical improvement with cyclosporine.
Autoimmune neutropenia is occasionally seen in young people (20 – 40 year age group) predominantly women and in this setting is often associated with other disorders or conditions 94).
Congenital neutropenia
Congenital neutropenia or Kostmann’s syndrome, is a form of severe chronic neutropenia 95). Kostmann, a Swedish physician who described a large family with several severely affected members, originally described this disease entity in 1956. Inherited in both an autosomal dominant and recessive manner, this syndrome is most often recognized at birth or shortly thereafter because of significant fever and infection. Oomphalatis, cellulitis, and perirectal abscesses are particularly common. Morphologic examination of bone marrow from these patients usually reveals almost no evidence of developing neutrophils beyond the promyelocyte stage. However, formation of monocytes and eosinophils usually remains normal. In vitro cultures demonstrate adequate numbers of colony forming cells (CFCGM), in which normal maturation of progenitor cells into mature neutrophils variably occurs. Upon the exposure to supraphysiologic levels of recombinant human granulocyte colony stimulating factor (rHuGCSF), however, these CFC-GM often form mature neutrophils. While this observation might suggest impaired synthesis of G-CSF in these patients, biologically active levels of this cytokine are usually elevated or normal. Hence, the G-CSF receptor somehow fails to transduce its signal appropriately.
G-CSF receptors appear normal in number and binding affinity in almost all patients evaluated. However, occasional children with Kostmann’s syndrome – almost all in transition to acute myeloid leukemia (AML) – have been shown to manifest abnormalities of the receptor for G-CSF. In these rare cases, somatic mutation in one of the two alleles prevents function of the receptor encoded by the remaining normal allele. This mutated receptor appears to disrupt the normal regulation of myeloid growth, and might facilitate the evolution of leukemic subpopulations. It should be emphasized, however, that for the large majority of patients with Kostmann’s syndrome, no obvious defect has been detected – suggesting a postreceptor problem.
Cyclic neutropenia
Cyclic neutropenia is a rare disorder that causes frequent infections and other health problems in affected individuals 96). People with cyclic neutropenia have recurrent episodes of neutropenia during which there is a shortage (deficiency) of neutrophils. The episodes of neutropenia are apparent at birth or soon afterward. For most affected individuals, neutropenia recurs every 21 days and lasts about 3 to 5 days 97).
Cyclic neutropenia is a rare condition and is estimated to occur in 1 in 1 million individuals worldwide.
Cyclic neutropenia appears to affect males and females in equal numbers. Most cases of cyclic neutropenia are thought to be present at birth (congenital); however, in some cases, the symptoms may not become obvious until childhood, adolescence, or early adulthood.
Cyclic neutropenia is a subdivision of severe chronic neutropenia. Severe chronic neutropenia is estimated to affect approximately 0.5 to 1 per million population in the United States 98).
Neutropenia makes it more difficult for the body to fight off pathogens such as bacteria and viruses, so people with cyclic neutropenia typically develop recurrent infections of the sinuses, respiratory tract, and skin. Additionally, people with this condition often develop open sores (ulcers) in the mouth and colon, inflammation of the throat (pharyngitis) and gums (gingivitis), recurrent fever, or abdominal pain. People with cyclic neutropenia have these health problems only during episodes of neutropenia. At times when their neutrophil levels are normal, they are not at an increased risk of infection and inflammation.
Cyclic neutropenia causes
Cyclic neutropenia may be inherited or acquired. Some cases are present at birth (congenital) and appear to occur randomly for no apparent reason (sporadically). There have been reports in the medical literature in which individuals within several multigenerational families (kindreds) have an increased incidence of cyclic neutropenia. In such familial cases, the disorder may be inherited as an autosomal dominant trait.
Investigators have determined that cases of sporadic and autosomal dominant cyclic neutropenia may be caused by disruption or changes (mutations) of the ELANE gene located on the short arm (p) of chromosome 19 (19p13.3) 99).
Mutations in the ELANE gene cause cyclic neutropenia. The ELANE gene provides instructions for making a protein called neutrophil elastase, which is found in neutrophils. When the body starts an immune response to fight an infection, neutrophils release neutrophil elastase. This protein then modifies the function of certain cells and proteins to help fight the infection.
ELANE gene mutations that cause cyclic neutropenia lead to an abnormal neutrophil elastase protein that seems to retain some of its function. However, neutrophils that produce abnormal neutrophil elastase protein appear to have a shorter lifespan than normal neutrophils. The shorter neutrophil lifespan is thought to be responsible for the cyclic nature of this condition. When the affected neutrophils die early, there is a period in which there is a shortage of neutrophils because it takes time for the body to replenish its supply.
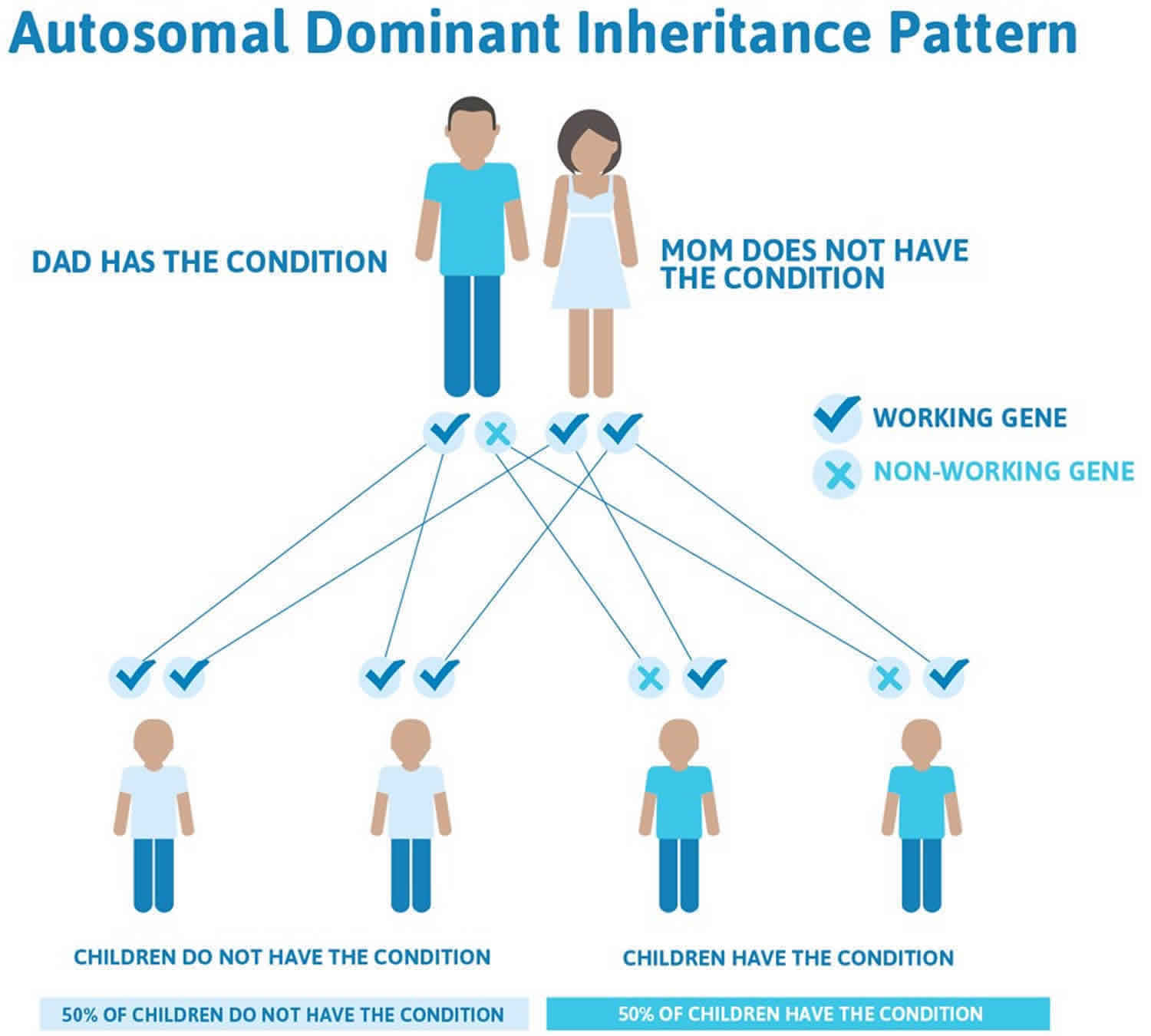
Cyclic neutropenia inheritance pattern
Cyclic neutropenia is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder.
In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
In most cases, an affected person inherits the mutation from one affected parent. Other cases result from new mutations in the gene and occur in people with no history of the disorder in their family. This is called a de novo mutation.
Figure 9 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 9. Cyclic neutropenia autosomal dominant inheritance pattern
Cyclic neutropenia symptoms
The primary finding associated with cyclic neutropenia is a severe chronic decrease in certain white blood cells (neutrophils). In most cases, episodes of neutropenia recur every 21 days (cyclic) and may last for three to six days. The cycling period usually remains constant and consistent among affected individuals. In addition, abnormal levels of red blood cells that assist in clotting (platelets), immature red blood cells (reticulocytes), and other types of white blood cells (monocytes) may occur. The monocyte count invariable increases during the periods of neutropenia.
During episodes of neutropenia, affected individuals may experience fever, a general feeling of ill health (malaise), inflammation and ulceration of the mucous membranes of the mouth (stomatitis), inflammation of the throat (pharyngitis), inflammation and degeneration of the tissues that surround and support the teeth (periodontal disease), and/or loss of appetite. Peridontal disease may result in loosening of teeth and early tooth loss in young children.
Individuals with cyclic neutropenia may be abnormally susceptible to various bacterial infections that often affect the skin, digestive (gastrointestinal) tract, and respiratory system. Such bacterial infections vary in severity and, in some cases, may result in life-threatening complications.
Cyclic neutropenia diagnosis
A diagnosis of cyclic neutropenia is made based upon a detailed patient history and thorough clinical evaluation. A diagnosis may be confirmed by monitoring an individual’s neutrophil count twice or three times per week for six weeks. Individuals with cyclic neutropenia should be genetically tested for mutations in the ELANE gene.
Cyclic neutropenia treatment
Prompt, appropriate treatment of the infections associated with cyclic neutropenia is important. Such treatment may include antibiotic therapy. Careful oral and dental care is also required. In addition, individuals with cyclic neutropenia should avoid activities that may cause minor injuries.
A synthetic drug that stimulates the bone marrow’s production of neutrophils (recombinant human granulocyte-colony stimulating factor [rhG-CSF]) has been used to treat severe chronic neutropenia. One form, the orphan drug neupogen (Filgrastim), has been approved by the Food and Drug Administration for use in the treatment of severe chronic neutropenia. Studies have shown that long-term therapy can elevate the numbers of neutrophils to normal range in most individuals, thereby reducing infections and other associated symptoms. Careful evaluation prior to initiation of such therapy and ongoing observation during therapy are essential to ensure the long-term safety and effectiveness of such treatment in individuals with severe chronic neutropenia. Neupogen is manufactured by Amgen Inc.
Genetic counseling may be of benefit for individuals with inherited forms of cyclic neutropenia and their families. Other treatment is symptomatic and supportive.
References [ + ]