Contents
Blocked milk duct
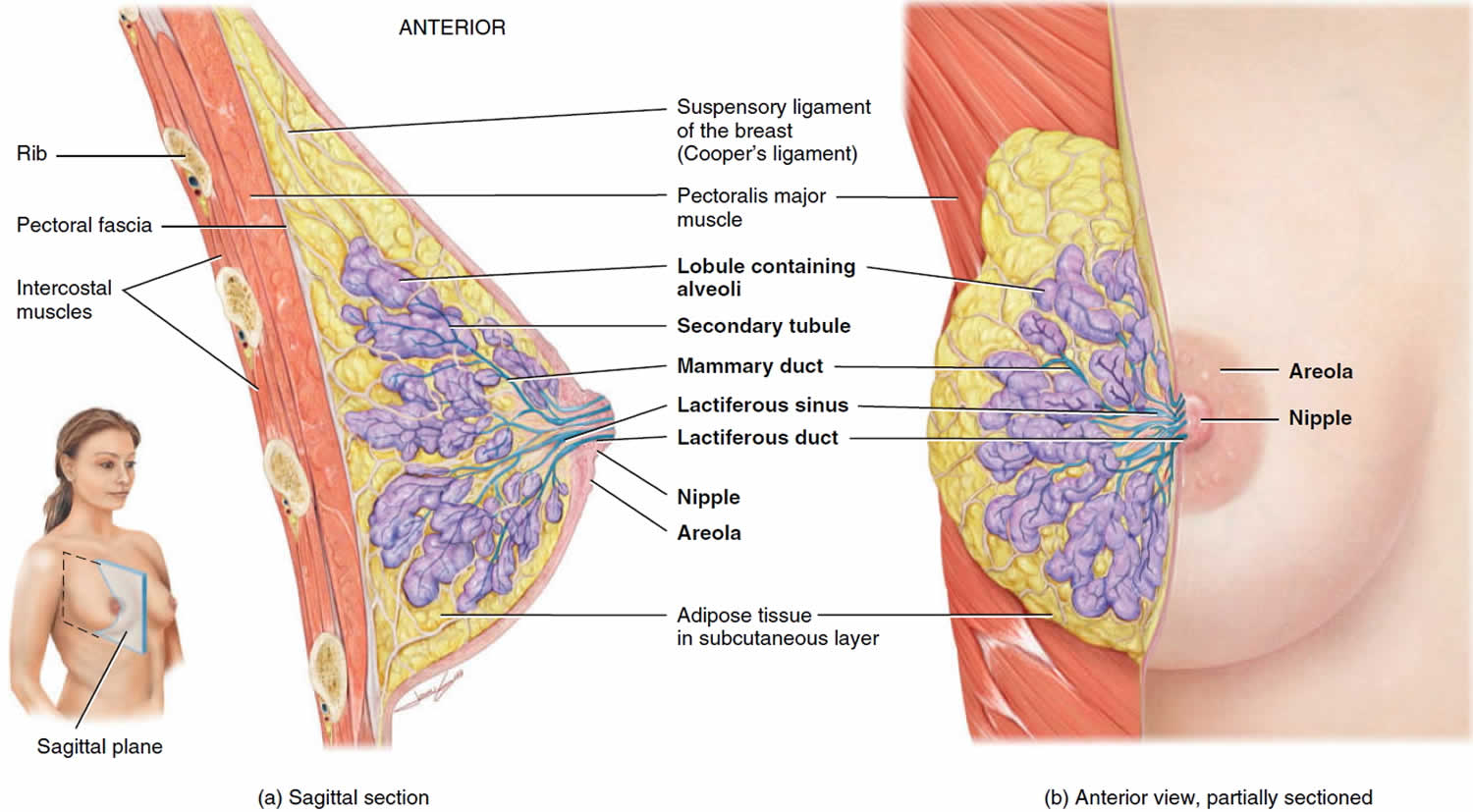
Blocked milk ducts also known as clogged milk ducts is an area or segment of the breast where milk flow is obstructed (milk stasis) causing a tender lump or spot in the breast of breastfeeding mothers. If a sore lump appears in your breast but you otherwise feel well, you probably have a blocked milk duct instead of mastitis (breast infection). This lump may be the result of a clogged milk duct, which can happen if there’s an abrupt change in the feeding schedule, inadequate draining of the breast, not varying nursing positions, or wearing clothes or bras that are too tight. Milk ducts also known as lactiferous ducts, are small tubes inside the breast that carry milk through to the nipples (see Figure 1). A blocked milk duct causes tender or painful lumps as a result of milk building up in the breast behind a duct. Occasionally, a mother with a blocked duct may notice a white spot on her nipple too.
Breast engorgement is when your breasts become swollen and get too full of milk. Breast engorgement is a painful condition affecting large numbers of women in the early postpartum period. Your breasts may feel hard, tight and painful. It is normal for your breasts to become larger, heavier, and a little tender when they begin making milk. Sometimes, this fullness may turn into breast engorgement, when your breasts feel very hard and painful. Breast engorgement is the result of the milk building up. Breast engorgement usually happens during the third to fifth day after giving birth. But it can happen at any time, especially if you have an oversupply of milk or are not feeding your baby or expressing your milk often. Breast engorgement can happen in the early days when you and your baby are still getting used to breastfeeding. It can take a few days for your milk supply to match your baby’s needs. Breast engorgement can also happen when your baby is older and not feeding so frequently, perhaps when they start having solid foods.
If breast engorgement continues, it can lead to a blocked milk duct. You may feel a small, tender lump in your breast.
Frequent feeding from the affected breast may help. If possible, position your baby with their chin pointing towards the lump so they can feed from that part of the breast.
Ducts carry the milk from deep in the breast to the nipple openings. Sometimes these ducts can become blocked. Milk builds up behind the blockage, a lump forms and your breast begins to feel sore. Your breast may become engorged in one area and might also look red. Mastitis is an inflammation of the breast which is usually caused by a blocked milk duct that hasn’t cleared, or a damaged nipple. Infection may or may not be present.
The most important part of treatment is frequent milk removal by breastfeeding or expressing (eight or more times each 24 hrs).
Figure 1. Normal breast (female)
What is mastitis?
Mastitis is infection in the breast. Mastitis can happen when you have a plugged duct that is not relieved, you miss or delay breastfeeding or if your breasts become engorged. Mastitis makes your breast feel painful and inflamed, and can make you feel very unwell with flu-like symptoms. You may feel a tender or painful hard spot in your breast that’s warm to the touch. The area may be red. You may have a fever, chills, aches or pain.
If you have mastitis, you’ll probably have at least 2 of these symptoms:
- a breast that feels hot and tender
- a red patch of skin that’s painful to touch
- a general feeling of illness, as if you have flu
- feeling achy, tired and tearful
- a high temperature (fever)
If you don’t deal with the early signs of mastitis, it can turn into an infection and you’ll need to take antibiotics. This can happen suddenly, and can get worse quickly. It’s important to carry on breastfeeding as this will help to speed your recovery.
If you think you’re developing a blocked duct or mastitis, try the following:
- Check your baby’s positioning and attachment. Ask your midwife, health visitor or a breastfeeding specialist to watch a feed.
- Let your baby feed on the tender breast first.
- Don’t stop nursing your baby even if your breast is sore. The infection doesn’t harm the baby. Breastfeeding more often can help clear the infection. Or use a breast pump to express milk from the infected breast.
- If the affected breast still feels full after a feed, or your baby can’t feed for some reason, express your milk by hand.
- Warmth can help the milk flow, so a warm towel on your breast or a warm bath or warm shower, can help.
- Get as much rest as you can. Go to bed if you can.
- Take acetaminophen (paracetamol) or ibuprofen to relieve the pain.
- If you’re no better within 12 to 24 hours or you feel worse, contact your doctor.
- If you’re in severe pain or have a fever, see your doctor. You may need antibiotics, which will be fine to take while breastfeeding.
- If your doctor prescribes an antibiotic to treat the infection, take it exactly as your doctor tells you to. Take all the medicine until it’s gone. Your provider makes sure the antibiotic is safe for your baby. Don’t start or stop taking any medicine during breastfeeding without your provider’s OK.
Remember, stopping breastfeeding will make your symptoms worse, and may lead to a breast abscess.
What is breast abscess?
If a mastitis infection isn’t treated, it can lead to a breast abscess (a collection of pus in the breast), which may need an operation to drain it.
Breast abscess can also develop if the mastitis doesn’t respond to frequent feeding plus a course of antibiotics.
You’ll have an ultrasound scan of your breast to check for an abscess.
The pus can be drained from an abscess with either:
- a needle – this might need to be done a few times, and you may have to go back to hospital each time
- a small cut in your skin
Your skin will be numbed before this is done. You can usually go home the same day and may be given antibiotics to take at home.
The abscess should heal completely in a few days or weeks.
You can carry on breastfeeding after an abscess has been drained.
What is breast engorgement
Breast engorgement is when your breasts become swollen and get too full of milk. Breast engorgement is a painful condition affecting large numbers of women in the early postpartum period. Your breasts may feel hard, tight and painful. It is normal for your breasts to become larger, heavier, and a little tender when they begin making milk. Sometimes, this fullness may turn into breast engorgement, when your breasts feel very hard and painful. Breast engorgement is the result of the milk building up. Breast engorgement usually happens during the third to fifth day after giving birth. But it can happen at any time, especially if you have an oversupply of milk or are not feeding your baby or expressing your milk often. Breast engorgement can happen in the early days when you and your baby are still getting used to breastfeeding. It can take a few days for your milk supply to match your baby’s needs. Breast engorgement can also happen when your baby is older and not feeding so frequently, perhaps when they start having solid foods.
Surgical enlargement of breasts (augmentation mammoplasty) may also predispose to breast engorgement 1). Breast engorgement should be differentiated from normal breast fullness, often called physiological breast engorgement 2), occurring between day two to three postpartum, in which secretory activation of the breast is triggered by the delivery of the placenta (progesterone withdrawal) and subsequent rise in prolactin levels 3). Increased milk production and interstitial tissue edema ensue resulting in visibly larger, warmer and slightly uncomfortable breasts. In women with normal breast fullness, milk flow from the breast is not hindered and with frequent, efficient breastfeeding, discomfort resolves within a few days.
Breast engorgement, on the other hand, is a distressing and debilitating condition affecting between 15% and 50% of women 4). Breast engorgement may lead to premature weaning, cracked nipples, mastitis and breast abscess.
Breast engorgement can also cause:
- Breast swelling
- Breast tenderness
- Warmth
- Redness
- Throbbing
- Flattening of the nipple
- Low-grade fever
Breast engorgement can lead to plugged ducts or a breast infection, so it is important to try to prevent it before this happens.
When breast engorgement was described as part of an inflammatory process (any mixture of redness, pain, fever, breast tension and resistance in breast tissue), 75% of women in a Swedish study experienced symptoms within eight weeks postpartum 5). Some level of breast tenderness during the first five days after birth was experienced by 72% of women in a study by Hill and Humenick 6). Breast engorgement symptoms occur most commonly between the second and fifth days postpartum 7), peaking at day five 8), but may occur as late as day 14 9) and are usually diffuse, bilateral and may be associated with a low‐grade fever. Complications are common and include sore/damaged nipples, mastitis, abscess formation, decreased milk supply 10), premature introduction of breast milk substitutes, and premature cessation of breastfeeding 11). Difficulty in feeding the baby occurs in up to 82% of mothers with breast engorgement 12).
If your baby isn’t well attached to the breast it may be hard for them to take your milk when your breast is engorged. The nipple can become a little over-stretched and flattened, and possibly painful.
Breast engorgement can still happen once you have learnt the skill of positioning and attachment, usually when your baby hasn’t fed for a while.
Your baby usually knows when they need a feed, for how long and from which breast. Early signs (cues) that your baby is ready to feed can include:
- moving their eyes rapidly
- putting their fingers into their mouth
- rooting (turning to one side with their mouth open as if seeking the breast)
- becoming restless
Crying is the very last sign that your baby needs feeding. Feeding them before they cry often leads to a much calmer feed. Keeping your baby close so you can watch and learn their early feeding cues will help.
Most of the time the discomfort goes away once you start breastfeeding regularly. Here are some ways to help with breast engorgement:
- Try not to miss or go a long time between feedings. Don’t skip night feedings.
- Express a small amount of milk with a breast pump or by hand before breastfeeding.
- Take a warm shower or put warm towels on your breasts. If your engorgement is really painful, put cold packs on your breasts.
- Tell your provider if your breasts stay swollen.
- Ask your midwife, doctor or a breastfeeding specialist for help immediately to help your baby drain your breasts more effectively.
Milk ejection reflex
Each time you express milk or sit down to breastfeed your baby, you may notice a sensation in your breasts called the ‘milk ejection’ reflex. In the early days, this takes a few minutes to appear, but later on it will occur within a few seconds. Milk ejection feels different to different women. You may have tingling or prickling in your breasts and nipples, or a feeling as if the milk is rushing in to fill them. Some mothers describe a slight pain and some mums have no sensations at all, but notice that milk starts to drip from both breasts.
What to do when you have oversupply of breast milk?
An overfull breast can make breastfeeding stressful and uncomfortable for you and your baby.
What you can do:
- Breastfeed on one side for each feeding. Continue to offer that same breast for at least two hours until the next full feeding, gradually increasing the length of time per feeding.
- If the other breast feels unbearably full before you are ready to breastfeed on it, hand express for a few moments to relieve some of the pressure. You can also use a cold compress or washcloth to reduce discomfort and swelling.
- Feed your baby before he or she becomes overly hungry to prevent aggressive sucking.
- Burp your baby often if he or she is gassy so there is more room in baby’s tummy for milk.
Clogged milk duct causes
The milk-making glands in your breasts are divided up into segments, rather like an orange (see Figure 1).
Narrow tubes called lactiferous ducts carry the milk from each segment to your nipple.
If one of the segments isn’t drained properly during a feed (perhaps because your baby isn’t attached properly), this can lead to a blocked duct.
You may feel a small, tender lump in your breast. And this needs relieving as soon as possible, and your baby may be able to help. If possible, place your baby with his/her chin pointing towards the lump so she/he can feed from that part of the breast.
Avoid wearing tight clothes or bras so your milk can flow freely from every part of your breast.
Other things that may help include:
- frequent feeding from the affected breast
- warm flannels or a warm shower to encourage the flow
- gently massaging the lump towards your nipple while your baby feeds
It’s important to deal with a blocked duct quickly as, if left, it could lead to mastitis.
Clogged milk duct prevention
Keeping pressure off your breasts will help prevent clogged ducts. You can do this by wearing clothing that is not restrictive (avoid tight tops, bras, or underwire bras; if necessary, switch to a larger bra size, or go without a bra for a while); by changing your nursing position so that your baby drains the milk from all areas of the breast equally; and by not sleeping on your stomach.
If you notice dried milk plugging the openings in your nipples, wash them gently with warm water after each breastfeeding session. Continued difficulties with clogged ducts may signal a problem with your baby’s latching on or with your nursing position. Arrange for a visit with your pediatrician or lactation specialist to correct these problems.
How can I prevent blocked milk ducts?
- Feed your baby often.
- Ensure correct positioning and attachment.
- Frequent drainage of the breast.
- Alter your position during breast feeds to include underarm position, cradle position or lying on your side.
- Check for a white ‘spot’ on the nipple as this may be blocking the milk duct.
- Avoid tight tops or bras or anything that puts pressure on your breasts.
- Rest as much as you can, eat well and stay healthy.
Avoid
- Sudden long gaps between breastfeeds or expressing for your baby.
- Tight or restrictive clothing such as a bra.
- Pressing or holding one area of the breast too tightly, especially close to the nipple.
Clogged milk duct symptoms
A painful red lump or swollen spot on the breast. You might also see a white spot on your nipple which is another sign that a duct may be blocked.
Blocked milk duct symptoms
- Local symptoms
- A reddened area or segment of the breast which becomes tender, hard and painful
- Occasionally, there can be localized tenderness or pain without an obvious lump
- May occur with a painful white blob/spot on the nipple
- Systemic symptoms
- Occasionally, a low-grade fever may be present, usually less than 101.3 °F (38.5 °C)
Mastitis
- Local symptoms
- A reddened area or segment of the breast which becomes tender, hard and painful
- Occasionally, there can be localized tenderness or pain without an obvious lump
- Usually more intense pain/heat/swelling than a blocked duct
- There may be red streaks extending outward from the affected area
- Systemic symptoms
- Fever of 101.3 °F (38.5 °C) or greater
- Flu-like symptoms including joint aches, pains and lethargy. Often rapid onset of symptoms
It’s important to start treatment as soon as you feel a lump or sore spot on your breast
Clogged milk duct treatment
A clogged duct should be dealt with immediately since it can lead to a breast infection. The best initial treatment for a clogged duct is to continue nursing, taking care to drain the breast as much as possible with each feeding. (If you suddenly stop breastfeeding, your breast will probably become engorged, which could make the condition worse and lead to an infection.)
Before each feeding, gently massage the breast, beginning on the outside and working your way toward the nipple, paying particular attention to the firm area. Breastfeed as often and as long as possible, offering your baby the sore breast first if you can tolerate it, because your baby will nurse most vigorously on the first breast, thus draining it more effectively.
Try switching positions to allow better drainage. Express milk from that breast after each feeding if your baby has not completely relieved breast fullness. Apply comfortably warm, moist towels on the affected breast several times a day (or take several warm baths or showers), gently massaging the area around the clogged duct down toward the nipple.
If the lump on your breast remains for more than a few days, if it increases in size or redness, or if you develop a fever or significant discomfort, make an appointment to see your doctor.
Management of blocked milk ducts:
- Start treatment as soon as you feel a lump or sore spot.
- Rest as much as possible.
- The most important part of treatment is frequent milk removal by breastfeeding or expressing (eight or more times each 24hrs).
- Feed frequently from the affected side first.
- Keep the affected breast as empty as possible by feeding from that side as often as you can.
- Applying warmth for up to a few minutes to the affected breast before a feed can help with milk flow.
- Feed from the affected breast first, when baby is sucking vigorously.
- Milk supply from the affected breast may decrease temporarily. This is normal – extra feeding or expressing will return your milk supply to normal.
- Your breast milk may taste salty due to increased sodium and chloride content. If your baby is breastfeeding, they may fuss due to this change in taste. If your baby is being fed by a naso-gastric tube they will not notice any difference.
- Check that your baby is attached well and can get the milk easily.
- Relax to help your let-down reflex work well.
- Gentle massage of the lump toward the nipple during feeds. This may assist the let-down reflex.
- Change feeding positions to help empty the breast.
- Hand express if needed, after feeds.
- You may express strings of thickened or fatty looking milk.
- Cold packs after a feed may help relieve pain and inflammation.
- If there is a white spot on your nipple – soak the nipple with a warm moist cloth and rub or scratch off the spot with a sterile needle to allow the duct to open and the milk to flow again.
- Use paracetamol or anti-inflammatory tablets according to directions until the lump clears.
- If the lump has not cleared after the next breastfeed, therapeutic ultrasound treatment (by a physiotherapist) of the affected breast may help clear blocked ducts.
- It is important the breast is well drained within 20 minutes of having the ultrasound treatment. This may be either by breastfeeding or expressing the breast.
- See your doctor if you cannot clear the lump in a few days, or sooner if you develop a fever or feel unwell.
After the mastitis has resolved, it is common for the affected area to feel bruised or remain reddened for a week or so afterwards.
Management before feeding or expressing
Apply warmth to the breast just before a feed (for up to 10minutes) or try expressing to help trigger a let-down. Warmth can be provided by a warm shower or a well-covered heat pack.
Gentle massage may also help trigger a let-down.
Hand express if needed to soften the areola to help your baby latch well.
Management during feeding or expressing
Start feeding or expressing on the sore breast first, but if too painful, start feeding or expressing on the less-sore side until your milk let-down occurs and then change sides.
Ensure your baby is latching well and ask for assistance if you are experiencing any difficulties.
Continue to massage your breast during feeding/expressing.
Management after feeding or expressing
If your baby has not drained the breast well during the feed, continue to massage and express until the breast feels well-drained.
If your baby has not been feeding effectively, you can feed this additional milk to your baby.
Cold packs can be applied to the affected breast for up to 10 minutes to reduce pain and inflammation.
Pain medication
A non-steroidal anti-inflammatory drug such as ibuprofen provides the most-effective reduction in symptoms such as pain and inflammation. Acetaminophen (paracetamol) can be taken in conjunction with ibuprofen. Use as directed.
Antibiotics
- Antibiotics are not needed to treat a blocked milk duct.
- If you have been unable to relieve the symptoms of a blocked duct after 12-24 hours, or if you develop a fever, you should see your GP for further management.
- If antibiotics are required, it is usually still safe to continue breastfeeding or expressing milk for your baby. Check with your doctor or pharmacist.
- Consider taking a probiotic to reduce the risk of thrush.
Tips to avoid further problems
- Do not wear bras or other clothing that is too tight.
- Avoid sleeping on your stomach.
- Do not go for long periods without either breastfeeding or expressing.
- Rest when you are able.
- Drink adequate fluids.
- Ensure correct attachment.
- Ensure the breast pump is positioned correctly.
- Regularly examine your breasts for lumps and massage these while feeding or expressing.
- Breastfeed as often as your baby needs (normally eight-to-12 times in 24hrs).
You should not try weaning if you have a blocked duct or are suffering mastitis. You must continue to remove milk from your breasts at this time in order to reduce the risk a breast abscess.
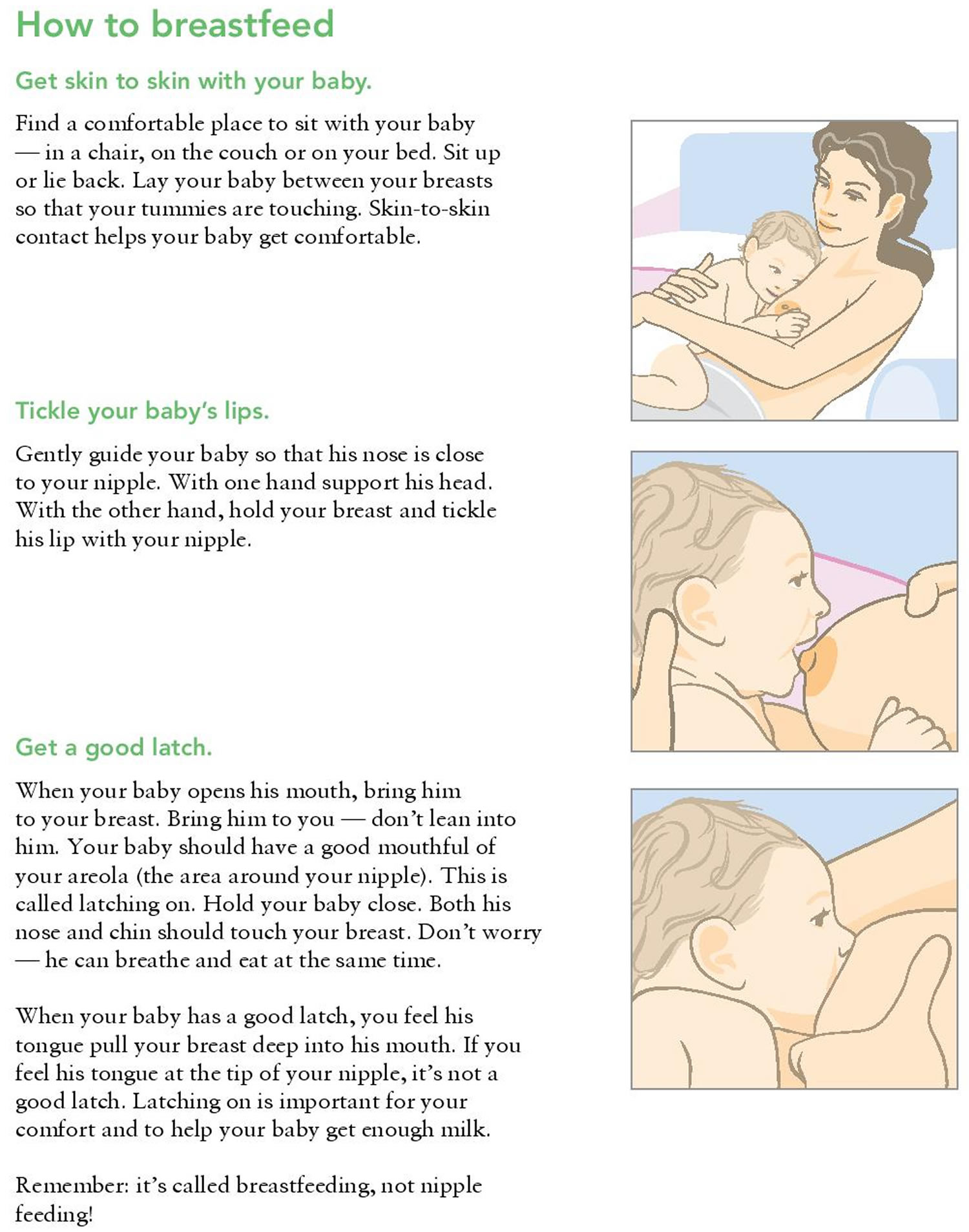
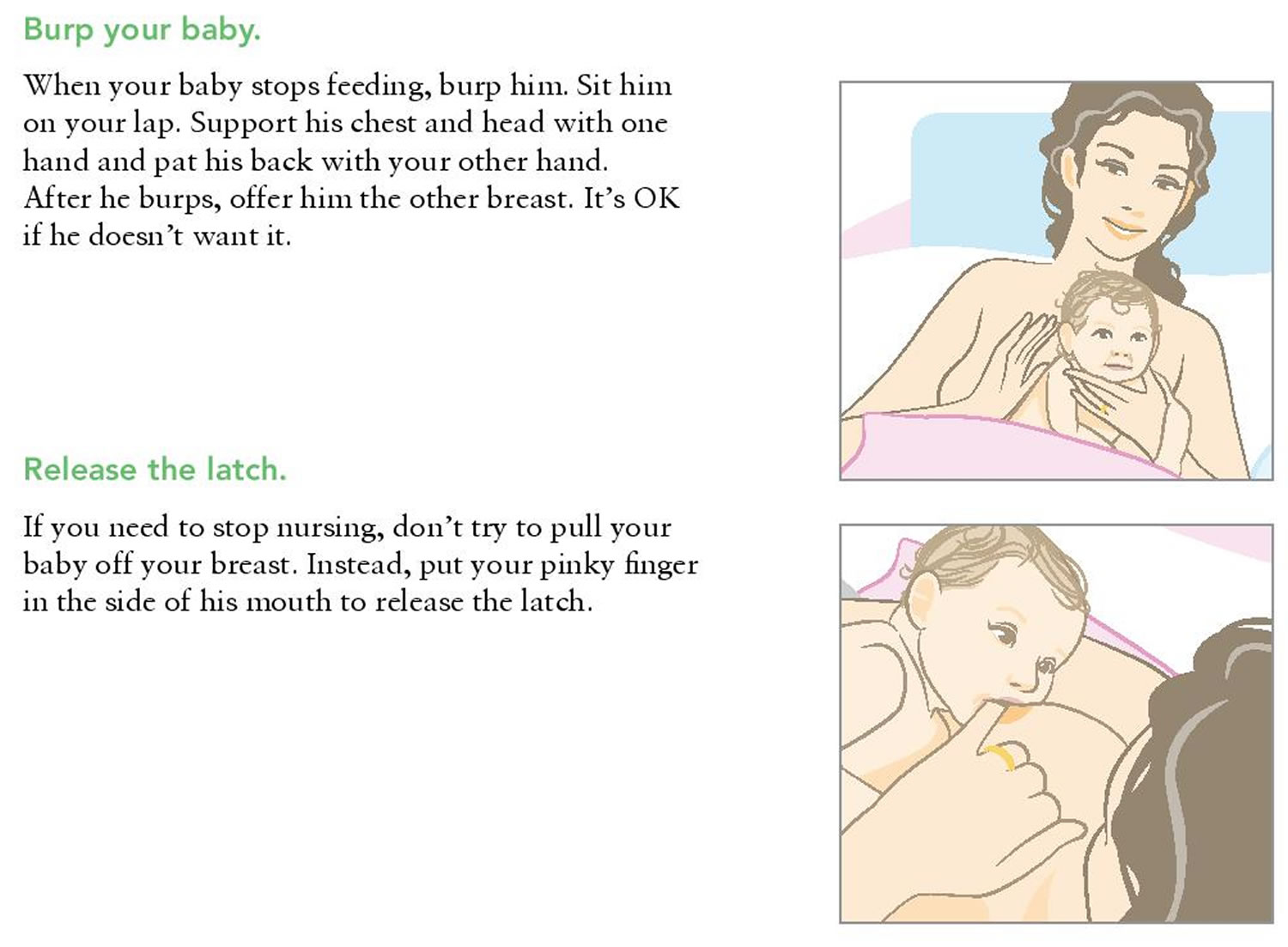
How to breastfeed
Breastfeeding positioning and attachment
If breastfeeding feels a bit awkward at first, don’t worry. Breastfeeding is a skill that you and your baby learn together, and it can take time to get used to.
There are lots of different positions you can use to breastfeed. You just need to check the following points:
- Are you comfortable? It’s worth getting comfortable before a feed. Use pillows or cushions if necessary. Your shoulders and arms should be relaxed.
- Are your baby’s head and body in a straight line? (It’s hard for your baby to swallow if their head and neck are twisted.)
- Are you holding your baby close to you, facing your breast? Supporting their neck, shoulders and back should allow them to tilt their head back and swallow easily.
- Always bring your baby to the breast rather than leaning forward to ‘post’ your breast into your baby’s mouth, as this can lead to poor attachment.
- Your baby needs to get a big mouthful of breast. Placing your baby with their nose level with your nipple will encourage them to open their mouth wide and attach to the breast well.
- Avoid holding the back of your baby’s head, so that they can tip their head back. This way your nipple goes past the hard roof of their mouth and ends up at the back of their mouth against the soft palate.
Breastfeeding positions
Some moms find that the following positions are helpful ways to get comfortable and support their babies while breastfeeding. You can also use pillows under your arms, elbows, neck, or back to give you added comfort and support. Keep trying different positions until you are comfortable. What works for one feeding may not work for the next feeding.
Clutch or “football” hold: useful if you had a C-section, or if you have large breasts, flat or inverted nipples, or a strong let-down reflex. This hold is also helpful for babies who like to be in a more upright position when they feed. Hold your baby at your side with the baby lying on his or her back and with his or her head at the level of your nipple. Support your baby’s head by placing the palm of your hand at the base of his or her head.
Cross-cradle or transitional hold: useful for premature babies or babies with a weak suck because this hold gives extra head support and may help the baby stay latched. Hold your baby along the area opposite from the breast you are using. Support your baby’s head at the base of his or her neck with the palm of your hand.
Cradle hold: an easy, common hold that is comfortable for most mothers and babies. Hold your baby with his or her head on your forearm and his or her body facing yours.
Laid-back hold (straddle hold): a more relaxed, baby-led approach. Lie back on a pillow. Lay your baby against your body with your baby’s head just above and between your breasts. Gravity and an instinct to nurse will guide your baby to your breast. As your baby searches for your breast, support your baby’s head and shoulders but don’t force the latch.
Side-lying position: useful if you had a C-section, but also allows you to rest while the baby breastfeeds. Lie on your side with your baby facing you. Pull your baby close so your baby faces your body.
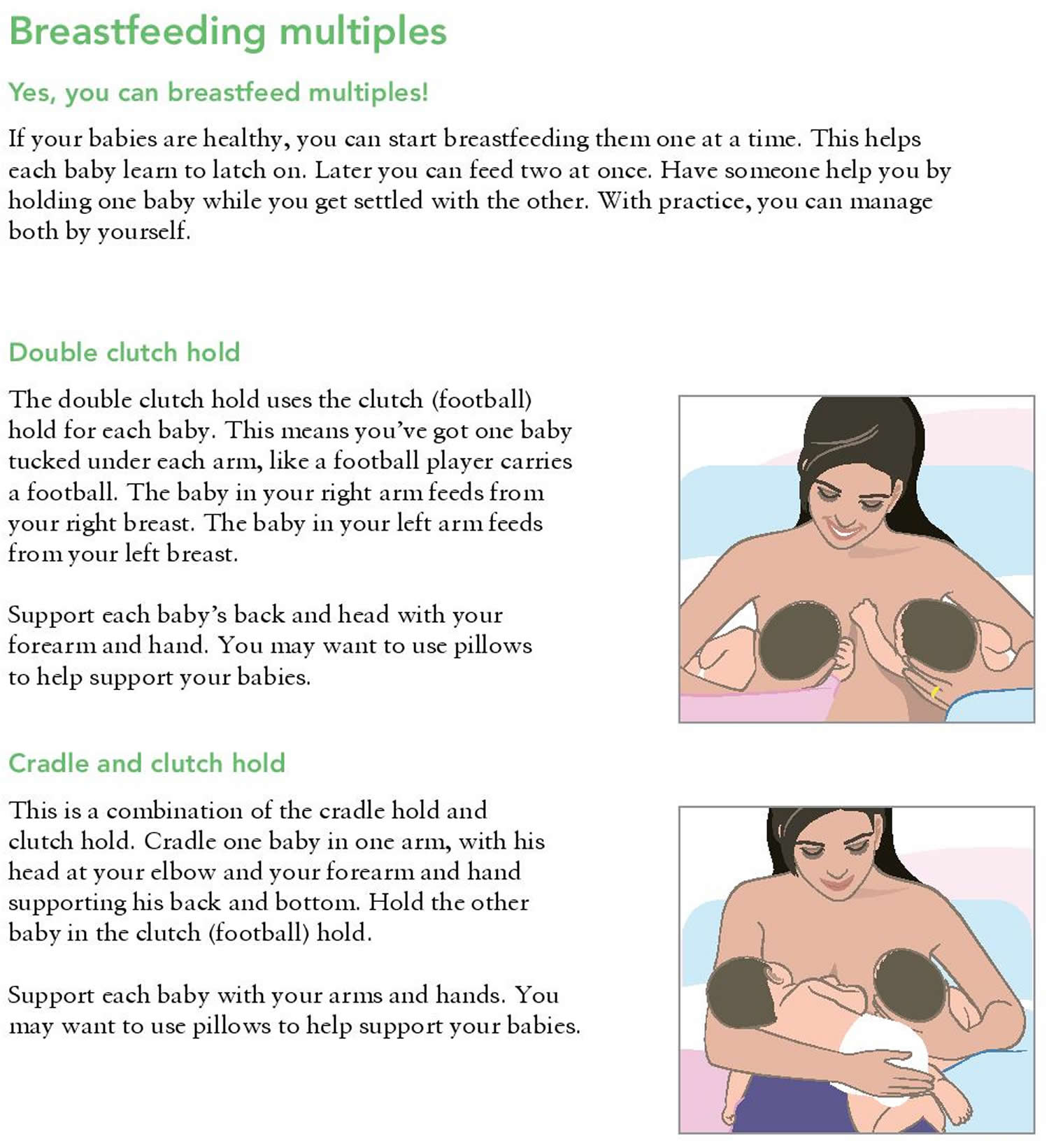
How to breastfeed twins, triplets or more
How to latch your baby on to your breast
- Hold your baby close to you with their nose level with the nipple.
- Wait until your baby opens their mouth really wide with their tongue down. You can encourage them to do this by gently stroking their top lip.
- Bring your baby on to your breast.
- Your baby will tilt their head back and come to your breast chin first. Remember to support your baby’s neck but not hold the back of their head. They should then be able to take a large mouthful of breast. Your nipple should go towards the roof of their mouth.
Getting a good latch
Getting your baby to “latch on” properly can take some practice. You can try different breastfeeding holds to help your baby get a good latch.
The steps below can help your newborn latch on to the breast to start sucking when he or she is ready. Letting your baby begin the process of searching for the breast may take some of the pressure off you and keeps the baby calm and relaxed. This approach to learning to breastfeeding is a more relaxed, baby-led latch. Sometimes called biological nurturing, laid-back breastfeeding, or baby-led breastfeeding, this style of breastfeeding allows your baby to lead and follow his or her instincts to suck.
Keep in mind that there is no one way to start breastfeeding. As long as the baby is latched on well, how you get there is up to you.
- Create a calm environment first. Recline on pillows or other comfortable area. Be in a place where you can be relaxed and calm.
- Hold your baby skin-to-skin. Hold your baby, wearing only a diaper, against your bare chest. Hold the baby upright between your breasts and just enjoy your baby for a while with no thoughts of breastfeeding yet.
- Let your baby lead. If your baby is not hungry, she will stay curled up against your chest. If your baby is hungry, she will bob her head against you, try to make eye contact, and squirm around. Learn how to read your baby’s hunger signs.
- Support your baby, but don’t force the latch. Support her head and shoulders as she searches for your breast. Avoid the temptation to help her latch on.
- Allow your breast to hang naturally. When your baby’s chin hits your breast, the firm pressure makes her open her mouth wide and reach up and over the nipple. As she presses her chin into the breast and opens her mouth, she should get a deep latch. Keep in mind that your baby can breathe at the breast. The nostrils flare to allow air in.
If you have tried the “baby-led” approach and your baby is still having problems latching on, try these tips:
- Tickle the baby’s lips with your nipple to encourage him or her to open wide.
- Pull your baby close so that the baby’s chin and lower jaw moves in to your breast.
- Watch the baby’s lower lip and aim it as far from the base of the nipple as possible so that the baby takes a large mouthful of breast.
Step by Step Guide in Getting your baby into position
Breastfeeding – Step 1. Hold your baby’s whole body close with their nose level with your nipple.
Breastfeeding – Step 2. Let your baby’s head tip back a little so that their top lip can brush against your nipple. This should help your baby to make a wide open mouth.
Breastfeeding – Step 3. When your baby’s mouth opens wide, their chin should be able to touch your breast first, with their head tipped back so that their tongue can reach as much breast as possible.
Breastfeeding – Step 4. With your baby’s chin firmly touching your breast and their nose clear, their mouth should be wide open. You should see much more of the darker nipple skin above your baby’s top lip than below their bottom lip. Your baby’s cheeks will look full and rounded as they feed.
What are signs of a good latch?
Signs your baby is well attached to your breast
- The latch feels comfortable to you and does not hurt or pinch.
- Your baby’s chest rests against your body. Your baby does not have to turn his or her head while drinking.
- Your baby has a wide mouth and a large mouthful of breast.
- The baby’s tongue is cupped under the breast, so you might not see the baby’s tongue.
- You hear or see your baby swallow. Some babies swallow so quietly that a pause in their breathing may be the only sign of swallowing.
- You see the baby’s ears “wiggle” slightly.
- Your baby’s lips turn outward like fish lips, not inward. You may not even be able to see the baby’s bottom lip.
- Your baby’s chin is touching your breast, their lower lip is rolled down (you can’t always see this) and their nose isn’t squashed against your breast.
- You don’t feel any pain in your breasts or nipples when your baby is feeding, although the first few sucks may feel strong.
- You can see more of the dark skin around your nipple (areola) above your baby’s top lip than below their bottom lip, depending on the size of your areola and the size of your baby’s mouth.
What are some common breastfeeding latch problems?
Below are some common latch problems and how to deal with them.
- You’re in pain. Many moms say their breasts feel tender when they first start breastfeeding. A mother and her baby need time to find comfortable breastfeeding positions and a good latch. If breastfeeding hurts, your baby may be sucking on only the nipple, and not also on the areola (the darker skin around the nipple). Gently break your baby’s suction to your breast by placing a clean finger in the corner of your baby’s mouth. Then try again to get your baby to latch on. To find out if your baby is sucking only on your nipple, check what your nipple looks like when it comes out of your baby’s mouth. Your nipple should not look flat or compressed. It should look round and long or the same shape as it was before the feeding.
- You or your baby feels frustrated. Take a short break and hold your baby in an upright position. Try holding your baby between your breasts with your skin touching his or her skin (called skin-to-skin). Talk or sing to your baby, or give your baby one of your fingers to suck on for comfort. Try to breastfeed again in a little while.
- Your baby has a weak suck or makes tiny sucking movements. Your baby may not have a deep enough latch to suck the milk from your breast. Gently break your baby’s suction to your breast by placing a clean finger in the corner of your baby’s mouth. Then try to get your baby to latch on again. Talk with a lactation consultant or pediatrician if you are not sure if your baby is getting enough milk. But don’t worry. A weak suck is rarely caused by a health problem.
- Your baby may be tongue-tied. Babies with a tight or short lingual frenulum (the piece of tissue attaching the tongue to the floor of the mouth) are described as “tongue-tied.” The medical term is ankyloglossia. These babies often find it hard to nurse. They may be unable to extend their tongue past their lower gum line or properly cup the breast during a feed. This can cause slow weight gain in the baby and nipple pain in the mother. If you think your baby may be tongue-tied, talk to your doctor.
How to tell if your baby is getting enough milk
- Your baby will appear content and satisfied after most feeds.
- They should be healthy and gaining weight (although it’s normal for babies to lose a little weight in the first days after birth). Talk to your midwife or health visitor if you are concerned your baby is not gaining weight and is unsettled during or after breast feeds.
- After the first few days, your baby should have at least six wet nappies a day.
- After the first few days, they should also pass at least two soft yellow poos (stools) every day.
How often you should feed your baby
How often babies feed varies. As a very rough guide, your baby should feed at least eight times or more every 24 hours during the first few weeks.
It’s fine to feed your baby whenever they are hungry, when your breasts feel full or if you just want to have a cuddle.
It’s not possible to overfeed a breastfed baby.
When your baby is hungry they may:
- get restless
- suck their fist or fingers
- make murmuring sounds
- turn their head and open their mouth (rooting)
It’s best to try and feed your baby during these early feeding cues as a crying baby is difficult to feed.
How to tell if your baby is getting enough milk
When you first start breastfeeding, you may be concerned your baby is not getting enough milk. You can’t always tell how much a breastfed baby is drinking.
It’s very rare that women don’t make enough breast milk for their babies, but it may take a little while before you feel confident your baby is getting what they need.
Your baby will generally let you know, but wet and dirty nappies are a good indication, as well as hearing your baby swallow.
If you need some reassurance your baby is getting enough milk, it’s a good idea to get a midwife, health visitor or breastfeeding specialist to watch your baby feed.
Try to carry on breastfeeding if you can. Introducing bottles of formula milk can fill up your baby’s stomach so they no longer want to breastfeed as frequently. This then reduces the stimulation for you to make more milk.
Signs your baby is getting enough milk
- Your baby starts feeds with a few rapid sucks followed by long, rhythmic sucks and swallows with occasional pauses.
- You can hear and see your baby swallowing.
- Your baby’s cheeks stay rounded, not hollow, during sucking.
- They seem calm and relaxed during feeds.
- Your baby comes off the breast on their own at the end of feeds.
- Their mouth looks moist after feeds.
- Your baby appears content and satisfied after most feeds.
- Your breasts feel softer after feeds.
- Your nipple looks more or less the same after feeds – not flattened, pinched or white.
- You may feel sleepy and relaxed after feeds.
Other signs your baby is feeding well
- Your baby gains weight steadily after the first two weeks – it’s normal for babies to lose some of their birth weight in the first two weeks.
- They appear healthy and alert when they’re awake.
- From the fourth day, they should do at least two soft, yellow poos (stools) every day for the first few weeks.
- From day five onwards, wet nappies should start to become more frequent, with at least six heavy, wet nappies every 24 hours. In the first 48 hours, your baby is likely to have only two or three wet nappies.
It can be hard to tell if disposable nappies are wet. To get an idea, take a nappy and add two to four tablespoons of water. This will give you an idea of what to look and feel for.
Things that can affect your milk supply
- Poor attachment and positioning.
- Not feeding your baby often enough.
- Drinking alcohol and smoking while breastfeeding – these can both interfere with your milk production.
- Previous breast surgery, particularly if your nipples have been moved.
- Having to spend time away from your baby after the birth – for example, because they were premature: Frequent gentle hand expression will help.
- Illness in you or your baby.
- Giving your baby bottles of formula or a dummy before breastfeeding is well established.
- Using nipple shields – although this may be the only way to feed your baby with damaged nipples and is preferable to stopping feeding.
- Some medications, including dopamine, ergotamine and pyridoxine.
- Anxiety, stress or depression.
- Your baby having a tongue tie that restricts the movement of their tongue.
With skilled help, lots of these problems can be sorted out. If you have concerns about how much milk your baby is getting, it’s important to ask for help early. Speak to your midwife, health visitor or a breastfeeding specialist. They can also tell you where you can get further support.
References [ + ]