Contents
What is bow legged
Bowlegs also called genu varum, is a condition in which the knees stay wide apart when a person stands with the feet and ankles together. Bowlegs is considered normal in children under 18 months. Infants are born bowlegged because of their folded position in the mother’s womb. Bowed legs begin to straighten once the child starts to walk and the legs begin to bear weight (about 12 to 18 months old).
Bowed legs in a toddler is very common. When a child with bowed legs stands with his or her feet together, there is a distinct space between the lower legs and knees. This may be a result of either one, or both, of the legs curving outward. Walking often exaggerates this bowed appearance.
In most cases, bowed legs will naturally begin to straighten as the child grows. If bowed legs have not resolved by the age of 3 years, there may be an underlying cause, such as Blount’s disease or rickets.
Adolescents occasionally have bowed legs. In many of these cases, the child is significantly overweight.
By around age 3, the child can most often stand with the ankles apart and the knees just touching. If the bowed legs are still present, the child is called bowlegged.
See your healthcare provider if your child shows ongoing or worsening bowed legs after age 3.
Here are some signs that suggest a child’s bowlegs or knock-knees may be caused by a serious problem:
- The curvature is extreme.
- Only one side is affected.
- The bowlegs get worse after age two years.
- The knock-knees persist after age seven years.
- Your child also is unusually short for his/her age.
If your child fits any of these descriptions, talk to your pediatrician. In some cases, treatment, including referral to a pediatric orthopedist, may be needed.
Bow legged causes
In most children under 2 years old, bowing of the legs is simply a normal variation in leg appearance. Doctors refer to this type of bowing as physiologic genu varum.
In children with physiologic genu varum, the bowing begins to slowly improve at approximately 18 months of age and continues as the child grows. By ages 3 to 4, the bowing has corrected and the legs typically have a normal appearance.
Bowlegs may be caused by illnesses, such as:
- Abnormal bone development
- Blount disease
- Fractures that do not heal correctly
- Lead or fluoride poisoning
- Rickets, which is caused by a lack of vitamin D
- Paget’s disease of bone
What is rickets
Rickets causes soft, weak bones in children. It usually occurs when they do not get enough vitamin D, which helps growing bones absorb the minerals calcium and phosphorous. It can also happen when calcium or phosphorus levels are too low.
Your child might not get enough vitamin D if he or she:
- Has dark skin
- Spends too little time outside
- Has on sunscreen all the time when out of doors
- Doesn’t eat foods containing vitamin D because of lactose intolerance or a strict vegetarian diet
- Is breastfed without receiving vitamin D supplements
- Can’t make or use vitamin D because of a medical disorder such as celiac disease
In addition to dietary rickets, children can get an inherited form of the disease. Symptoms include bone pain or tenderness, impaired growth, and deformities of the bones and teeth. Your child’s doctor uses lab and imaging tests to make the diagnosis. Treatment is replacing the calcium, phosphorus, or vitamin D that are lacking in the diet. Rickets is rare in the United States.
Rickets signs and symptoms
Signs and symptoms of rickets can include:
- Delayed growth
- Pain in the spine, pelvis and legs
- Muscle weakness
Because rickets softens the growth plates at the ends of a child’s bones, it can cause skeletal deformities such as:
- Bowed legs or knock knees
- Thickened wrists and ankles
- Breastbone projection
Rickets also can cause dental issues, such as cavities and problems with teeth structure.
Rickets complications
Left untreated, rickets can lead to:
- Failure to grow
- Abnormally curved spine
- Skeletal deformities
- Dental defects
- Seizures
What causes rickets?
A lack of vitamin D causes most cases of rickets. Vitamin D helps bones absorb calcium and phosphorus. If your child does not get enough vitamin D, their body may not get the nutrients it needs to make bones strong. Occasionally, not getting enough calcium or lack of calcium and vitamin D can cause rickets.
Rickets is most common in children ages 6 to 24 months. This is because their bones grow rapidly during this period. Your child also may be at risk if they:
- Have dark skin.
- Don’t get enough exposure to sunlight.
- Don’t eat enough foods containing vitamin D, calcium, or phosphorus.
- Breastfeed without getting a vitamin D supplement.
- Have an illness that prevents their body from making or absorbing vitamin D. One example is celiac disease.
Rickets also can run in families, and children can inherit it.
Lack of vitamin D
Children who don’t get enough vitamin D from these two sources can develop a deficiency:
- Sunlight. Your skin produces vitamin D when it’s exposed to sunlight. But children in developed countries tend to spend less time outdoors. They’re also more likely to use sunscreen, which blocks the rays that trigger the skin’s production of vitamin D.
- Food. Fish oils, fatty fish and egg yolks contain vitamin D. Vitamin D also has been added to some foods, such as milk, cereal and some fruit juices.
Problems with vitamin D absorption
Some children are born with or develop medical conditions that affect the way their bodies absorb vitamin D. Some examples include:
- Celiac disease
- Inflammatory bowel disease
- Cystic fibrosis
- Kidney problems
Risk factors for rickets
Factors that can increase a child’s risk of rickets include:
- Dark skin. Dark skin doesn’t react as strongly to sunshine as does lighter skin, so it produces less vitamin D.
- Mother’s vitamin D deficiency during pregnancy. A baby born to a mother with severe vitamin D deficiency can be born with signs of rickets or develop them within a few months after birth.
- Northern latitudes. Children who live in geographical locations where there is less sunshine are at higher risk of rickets.
- Premature birth. Babies born before their due dates are more likely to develop rickets.
- Medications. Certain types of anti-seizure medications and antiretroviral medications, used to treat HIV infections, appear to interfere with the body’s ability to use vitamin D.
- Exclusive breast-feeding. Breast milk doesn’t contain enough vitamin D to prevent rickets. Babies who are exclusively breast-fed should receive vitamin D drops.
Rickets prevention
In most cases, you can help prevent your child from having rickets. Make sure they get enough vitamin D and calcium. If your baby is breastfed or consumes more breast milk than formula, they need a vitamin D supplement. This is because breast milk does not contain enough vitamin D alone. Do not give your child vitamin supplements unless your doctor recommends them. Ask your doctor for dosage information.
If your child eats solid foods, you should manage their diet. Offer them foods high in vitamin D, such as breakfast cereals and orange juice, and calcium, such as milk, cheese, and salad greens.
Ask your doctor how much time in the sun is safe for your child. Remember that infants and babies require protection from direct sunlight. In addition, because of skin cancer concerns, infants and young children, especially, are warned to avoid direct sun or to always wear sunscreen and protective clothing.
For adults, during most seasons, 10 to 15 minutes of exposure to the sun near midday is enough. However, if you’re dark-skinned, if it’s winter or if you live in northern latitudes, you might not be able to get enough vitamin D from sun exposure.
If you’re pregnant, ask your doctor about taking vitamin D supplements.
Because human milk contains only a small amount of vitamin D, all breast-fed infants should receive 400 international units (IU) of oral vitamin D daily. The American Academy of Pediatricians recommends that breast-fed infants or those who drink less than 33.8 ounces (1 liter) of infant formula a day to take an oral vitamin D supplement.
Rickets diagnosis
Your doctor will ask about your family health history and your child’s health and diet. Your child will need a full physical exam. Blood tests and bone X-rays also help the doctor determine if your child has rickets.
Your doctor will pay particular attention to your child’s:
- Skull. Babies who have rickets often have softer skull bones and might have a delay in the closure of the soft spots (fontanels).
- Legs. While even healthy toddlers are a little bowlegged, an exaggerated bowing of the legs is common with rickets.
- Chest. Some children with rickets develop abnormalities in their rib cages, which can flatten and cause their breastbones to protrude.
- Wrists and ankles. Children who have rickets often have wrists and ankles that are larger or thicker than normal.
X-rays of the affected bones can reveal bone deformities. Blood and urine tests can confirm a diagnosis of rickets and also monitor the progress of treatment.
Rickets treatment
Treatment depends on the type of rickets your child has. For children who lack enough nutrients, the doctor will prescribe supplements for vitamin D and calcium. Your child’s pain and muscle weakness should get better within a few weeks.
Follow your child’s doctor’s directions as to dosage. Too much vitamin D can be harmful.
Your child’s doctor will monitor your child’s progress with X-rays and blood tests.
If your child has bone defects caused by rickets, they may need braces or surgery to correct the problem.
For children who inherit rickets or have an illness that caused rickets, you may need to see a specialist.
Living with rickets
Most cases of rickets go away once your child gets enough vitamin D. There may be lasting effects or defects that require further treatment, such as braces or surgery. Your child may need therapy as a result. It is possible that your child may require a strict diet in order to stay healthy.
What is Blount disease
Blount disease is a growth disorder that affects the bones of the lower leg, causing them to bow outward. In younger kids, just the tibia (shin bone) is affected. In teens, it’s usually both the tibia and the femur (thigh bone).
Many babies are born with slightly bowed legs from being in the small space of the womb. Their legs usually straighten out as they grow and start walking.
Blount disease is different. The curve gets worse if it’s not treated, so early diagnosis is very important.
In a child under the age of 2 years, it may be impossible to distinguish infantile Blount’s disease from physiologic genu varum. By the age of 3 years, however, the bowing will worsen and an obvious problem can often be seen in an x-ray.
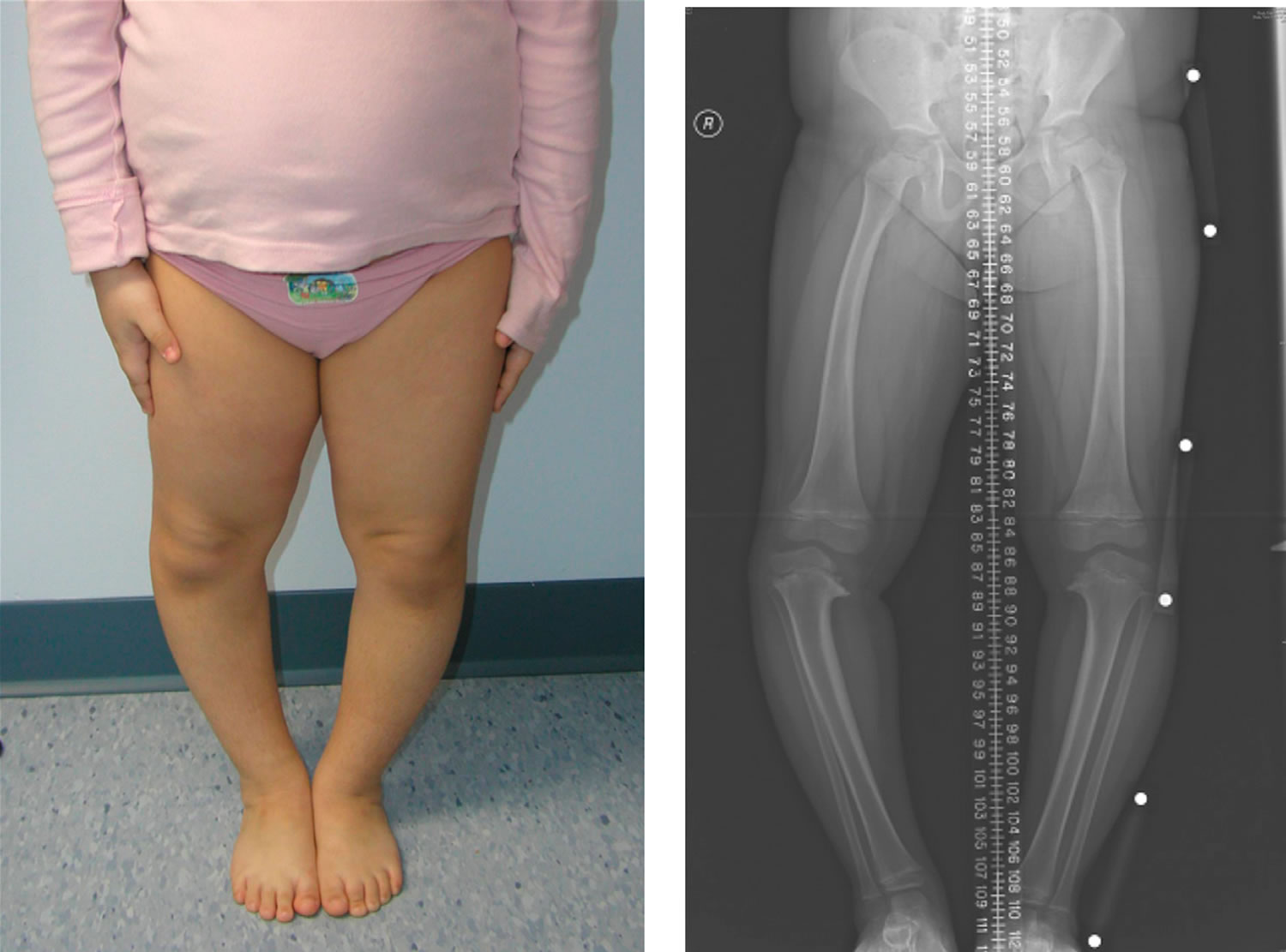
Figure 1. Blount disease
Footnote: 5 year old girl with bilateral early-onset Blount disease
[Source 1) ]Risks factors for Blount disease
Most kids who get Blount disease are overweight or gained weight very quickly. It’s also more common in people of African heritage, kids who started walking at an early age, and those with a family member who had it.
In Blount disease, a lot of pressure is put on the growth plate (an area of growing bone tissue) at the top of the tibia. As a result, the bone can’t grow normally. The lateral (outer) side of the tibia keeps growing but the medial (inner) side of the bone does not.
This uneven bone growth causes the tibia to bend outward instead of grow straight. One leg may also become slightly shorter than the other.
Blount disease signs and symptoms
The most obvious symptom of Blount disease is a bowing of the leg below the knee. In young kids, it’s usually not painful, though it can affect the way they walk. For preteens and teens, Blount disease may cause knee pain that gets worse with activity.
The tibia can be rotated as well as bowed, causing a condition called in-toeing (when the feet point inward instead of straight out).
Over time, Blount disease can lead to arthritis of the knee joint and, in severe cases, trouble walking.
Blount disease diagnosis
When doctors suspect Blount disease, they may recommend taking a child to an orthopedic doctor (bone specialist) for leg X-rays and further examination.
Mild bone changes can be hard to spot in kids younger than 2 because their bowed legs might be normal and straighten out on their own. It’s easier for doctors to diagnose Blount disease in kids after age 2.
Blount disease treatment
Treatment of Blount disease depends on a child’s age and how curved the bone is.
Usually, doctors will just keep a close eye on the condition in children younger than 2. Kids 2 to 4 years old and those with severe bowing might need leg braces, called KAFOs (knee-ankle-foot orthotics). Knee-ankle-foot orthotics, which go from the thigh to the toes, are created for kids using a mold of their leg. The hope is that the braces gradually shift leg bones to a straighter position over time. However, doctors have differing opinions on KAFOs. If you have questions about them, talk to your doctor.
Older kids and teens, or kids who don’t get better wearing knee-ankle-foot orthotics, might need surgery:
- The surgeon can cut the bone, straighten it, and fasten it with plates and screws. This is called an osteotomy.
- Another procedure can slow or stop the growth of half of the growth plate to allow the other side to catch up and straighten the leg.
- A device called an external fixator can be put on the outside of the leg and attached to the bones after they are cut. It holds the bones in place while gradually straightening the leg.
If surgery is necessary, it will be done under general anesthesia. This means your child will be sedated and asleep and won’t feel anything. Afterward, your child might wear a cast or use crutches and a wheelchair for a while. Physical therapy also might be needed.
Blount disease prognosis
Most kids who are treated for Blount disease get better and have active lives.
If being overweight caused the Blount disease, it’s important for parents to help their child reach and maintain a healthy weight. This can reduce stress on the bones and joints and prevent other long-term problems from weight gain (like type 2 diabetes and heart disease).
If you need help getting your child to adopt a healthier lifestyle that includes a balanced diet and exercise, talk to your doctor.
Bow legged prevention
There is no known way to prevent bowlegs, other than to avoid rickets. Make sure your child is exposed to sunlight and gets the proper amount of vitamin D in their diet.
Bow legged symptoms
Bowed legs are most evident when a child stands and walks. The most common symptom of bowed legs is an awkward walking pattern.
Toddlers with bowed legs usually have normal coordination, and are not delayed in learning how to walk. The amount of bowing can be significant, however, and can be quite alarming to parents and family members.
Turning in of the feet (intoeing) is also common in toddlers and frequently occurs in combination with bowed legs.
Bowed legs do not typically cause any pain. During adolescence, however, persistent bowing can lead to discomfort in the hips, knees, and/or ankles because of the abnormal stress that the curved legs have on these joints. In addition, parents are often concerned that the child trips too frequently, particularly if intoeing is also present.
Symptoms may include:
- Knees that do not touch when standing with feet together (ankles touching)
- Bowing of legs is same on both sides of the body (symmetrical)
- Bowed legs continue beyond age 3
Bow legged diagnosis
Your doctor will begin your child’s evaluation with a thorough physical examination.
If your child is under age 2, in good health, and has symmetrical bowing (the same amount of bowing in both legs), then your doctor will most likely tell you that no further tests are currently needed.
However, if your doctor notes that one leg is more severely bowed than the other, he or she may recommend an x-ray of the lower legs. An x-ray of your child’s legs in the standing position can show Blount’s disease or rickets.
If your child is older than 2 1/2 at the first doctor’s visit and has symmetrical bowing, your doctor will most likely recommend an x-ray. The likelihood of your child having infantile Blount’s disease or rickets is greater at this age. If the x-ray shows signs of rickets, your doctor will order blood tests to confirm the presence of this disorder.
X-rays may be needed if:
- The child is 3 years old or older.
- The bowing is getting worse.
- Bowing is not the same on both sides.
- Other test results suggest disease.
Bow legged treatment
No treatment is recommended for bowlegs unless the condition is extreme. The child should be seen by a medical professional at least every 6 months.
Physiologic genu varum nearly always spontaneously corrects itself as the child grows. This correction usually occurs by the age of 3 to 4 years.
Untreated infantile Blount’s disease or untreated rickets results in progressive worsening of the bowing in later childhood and adolescence. Ultimately, these children have leg discomfort (especially the knees) due to the abnormal stresses that occur on the joints. Adolescents with Blount’s disease are most likely to experience pain with the bowing.
Nonsurgical Treatment
- Physiologic genu varum. Although physiologic genu varum does not require active treatment, your doctor will want to see your child every 6 months until the bowing has resolved.
- Blount’s disease. Infantile Blount’s disease does require treatment for the bowing to improve. If the disease is caught early, treatment with a brace may be all that is needed. Bracing is not effective, however, for adolescents with Blount’s disease.
- Rickets. If your child has rickets, your doctor will refer you to a metabolic specialist for medical management, in addition to regular orthopaedic followup. The effects of rickets can often be controlled with medication.
Surgical Treatment
- Physiologic genu varum. In rare instances, physiologic genu varum in the toddler will not completely resolve and during adolescence, the bowing may cause the child and family to have cosmetic concerns. If the deformity is severe enough, then surgery to correct the remaining bowing may be needed.
- Blount’s disease. If bowing continues to progress in a child with infantile Blount’s disease despite the use of a brace, surgery will be needed by the age of 4 years. Surgery may stop further worsening and prevent permanent damage to the growth area of the shinbone. Older children with bowed legs due to adolescent Blount’s disease require surgery to correct the problem.
- Rickets. Surgery may also be needed for children with rickets whose deformities persist despite proper management with medications.
Surgical procedures
There are different procedures to correct bowed legs, and they fall into two main types.
- Guided growth. This surgery of the growth plate stops the growth on the healthy side of the shinbone which gives the abnormal side a chance to catch up, straightening the leg with the child’s natural growth.
- Tibial osteotomy. In this procedure, the shinbone is cut just below the knee and reshaped to correct the alignment. The bone is held in place while it heals with either an internal plate and screws, or an external frame that is positioned on the outside of the leg.
After surgery, a cast may be applied to protect the bone while it heals. Crutches may be necessary for a few weeks, and your doctor may recommend physical therapy exercises to restore strength and range of motion. Your doctor will talk to you about full recovery time and return to regular activities.
References [ + ]