Contents
Bladder retraining
The aim of bladder training is to help you gain better control over your bladder. When you do bladder training you are aiming to:
- decrease the number of times you go to the toilet (frequency)
- hold on for longer or put off emptying your bladder until your bladder is full, and
- increase the volume of urine you pass each time when you do go to the toilet.
The Continence Foundation recommends you work with a continence nurse advisor or physiotherapist to design a bladder training program to suit your individual needs. Bladder training programs may take up to three months, with weekly or fortnightly appointments to monitor your progress and measure your improvement.
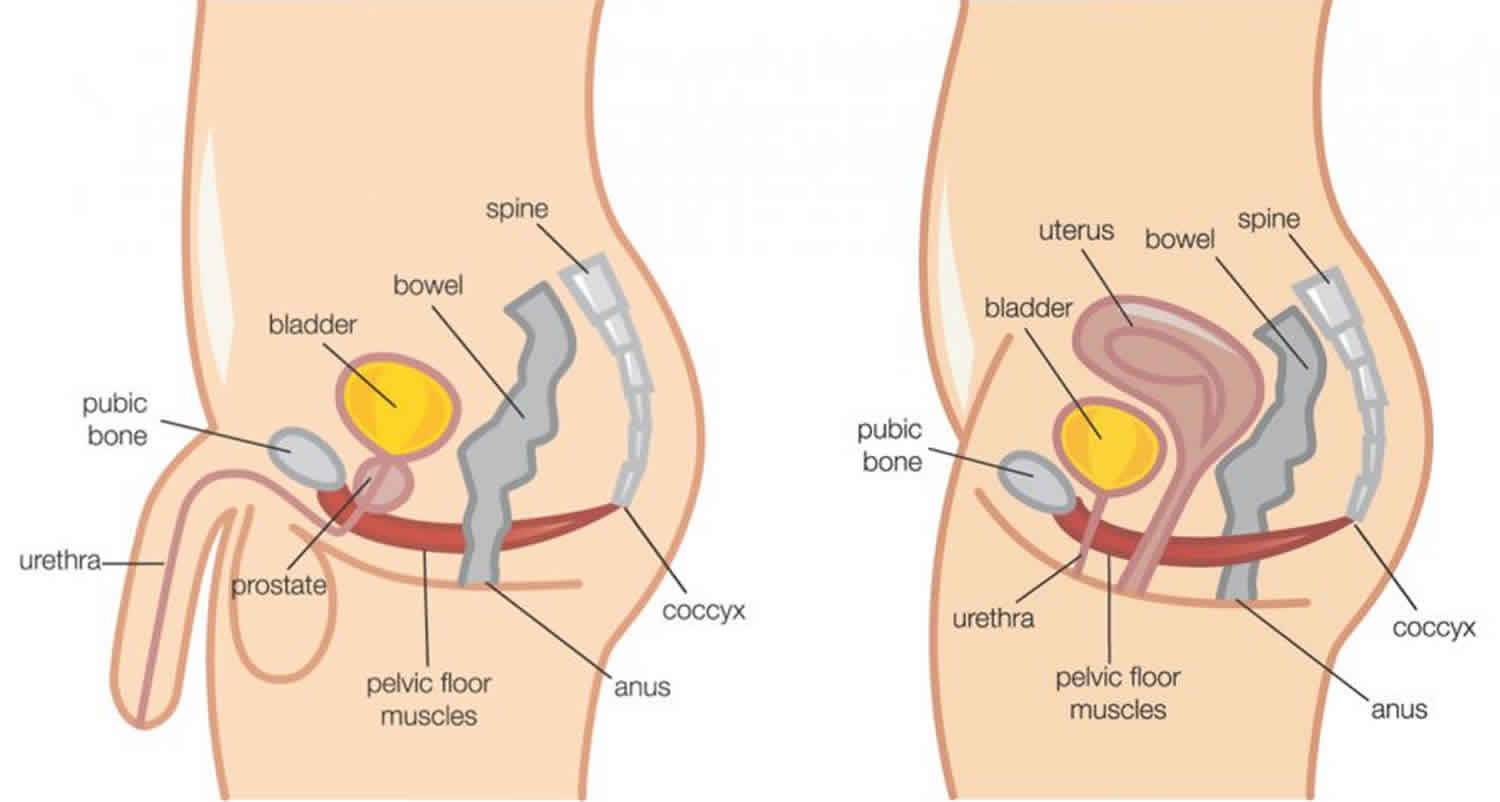
Your continence professional will teach you how to use your pelvic floor muscles. These muscles support your bladder and urethra (the tube that carries urine from the bladder to outside) and help to hold back the strong urge to pass urine. This will help you defer (put off) going to the toilet, or hold it in until you reach a toilet. The overall aim of bladder training is to restore the normal function of your bladder.
Over time, you should notice not needing to go to the toilet all the time, being able to stop yourself from going and passing more urine when you do go. You will also learn about diet and lifestyle modifications, including how to manage constipation (and straining), which can cause poor bladder control.
Bladder training takes time, so don’t worry if it feels like things are not improving right away. The important thing is to keep trying, make note of the things that make a difference, and stay positive.
Most bladder training programs will start by asking you to keep a bladder diary (see below). Every time you pass urine, you record the date, time and how much urine you passed. You will need to do this for a few days to identify how much your bladder holds and how often you need to empty it. You should also include comments about leaking or other symptoms such as burning or pain.
Step-by-step bladder-training technique
- Keep track. For a day or two, keep track of the times you urinate or leak urine during the day.
- Keeping a bladder diary
- Complete the information for two consecutive 24-hour periods. Record both day and night.
- Begin with first urination upon arising.
- Record intake amount in ounces and type of fluid (for example, coffee, juice, water, etc.).
- Record approximate urine output and time of urination.
- Keeping a bladder diary
- Calculate. On average, how many hours do you wait between urinations during the day?
- Choose an interval. Based on your typical interval between urinations, select a starting interval for training that is 15 minutes longer. If your typical interval is one hour, make your starting interval one hour and 15 minutes.
- Hold back. When you start training, empty your bladder first thing in the morning and not again until the interval you’ve set. If the time arrives before you feel the urge, go anyway. If the urge hits first, remind yourself that your bladder isn’t really full, and use whatever techniques you can to delay going. Try the pelvic floor exercises sometimes called Kegels, or simply try to wait another five minutes before walking slowly to the bathroom.
- Increase your interval. Once you are comfortable with your set interval, increase it by 15 minutes. Over several weeks or months, you may find you are able to wait much longer and that you experience far fewer feelings of urgency or episodes of urge incontinence.
People with an overactive or weak bladder have to rush off to find a bathroom because of an urge to urinate, or may gradually lose urine drop by drop before arriving at a toilet. Bladder training can then help you to regain at least some control over your bladder.
The bladder muscle can be trained to stretch more so that the bladder is able to hold more urine. Bladder training also includes various behavioral treatment approaches and a particular drinking and voiding schedule (bathroom visit schedule).
Review any lifestyle factors which may be contributing to poor bladder function.
Lifestyle measures
- Regulating your fluid intake: Your professional advisor can help you regulate your fluid intake so you drink the correct volume for your body and level of activity at the right times. Too much fluid can overfill the bladder and too little can concentrate the urine, which irritates the bladder. Drinking about 1.5L of fluid per day (mostly water) aim to regularly pass 300ml or more urine.
- Limit alcohol and caffeine-based drinks: Alcohol, caffeine-based drinks and fizzy drinks are known to irritate the bladder, which exacerbates symptoms of overactive bladder. Alcohol also has a diuretic effect, which can cause more frequent urination.
- Avoid constipation: Constipation can trigger or worsen symptoms of overactive bladder. Straining on the toilet can also weaken the pelvic floor.
- Keep your weight in the healthy range: there is evidence that losing weight decreases the severity and frequency of symptoms of overactive bladder. Maintain a healthy weight by walking for at least thirty minutes each day
- Only going to the toilet when you need to go (not going “just-in-case”)
- Get rid of any cough or sneezing
- Exercise your pelvic floor muscles as you have been shown.
- It is important to have strong pelvic floor muscles.
- Do persevere. You have the ability to make your brain the boss and retrain your bladder!
- Do speak to your physiotherapist, doctor or continence consultant about any concerns or problems you encounter.
Figure 1. Bladder diary
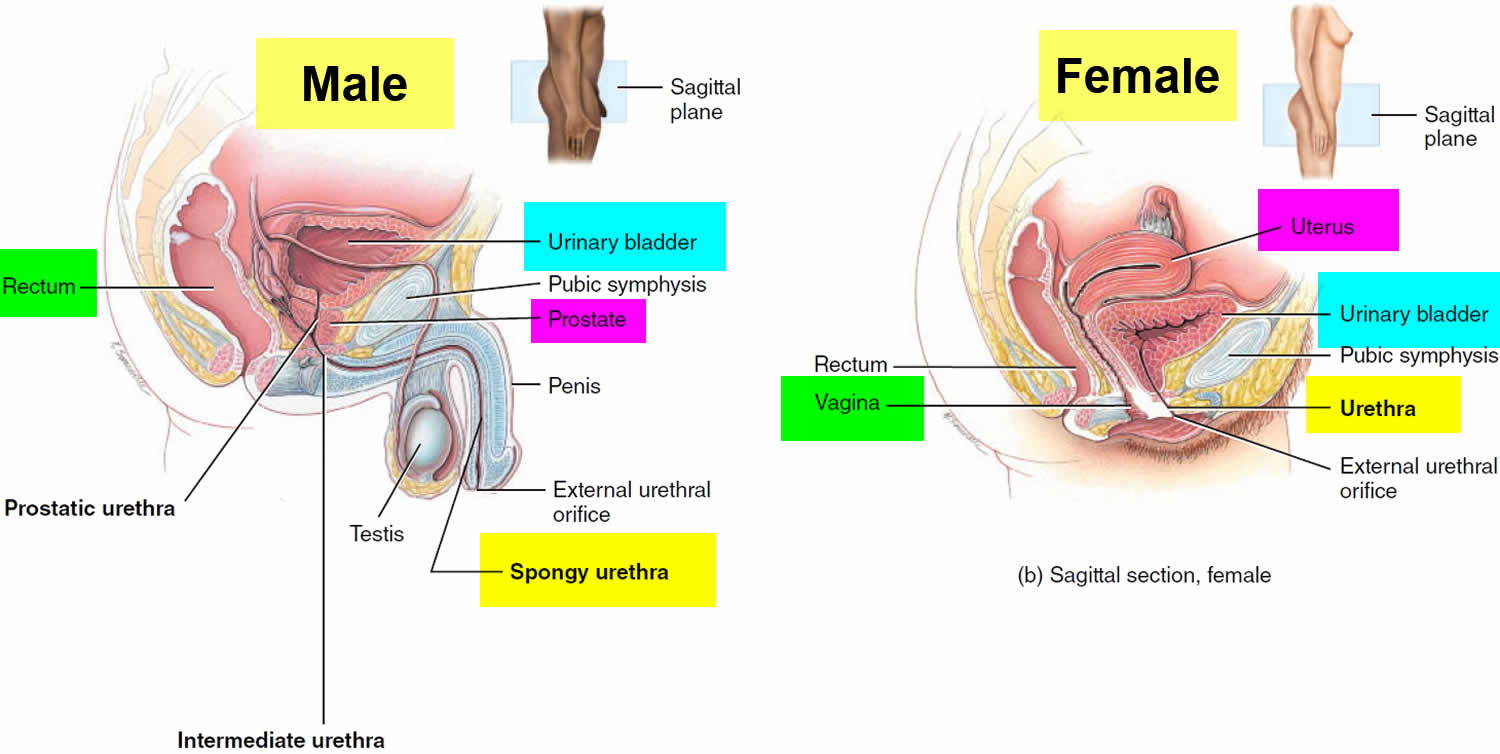
Figure 2. Urinary bladder anatomy
Figure 3. Urinary bladder anatomy
What are normal bladder habits?
Your bladder normally stores urine, which is produced by your kidneys. The kidneys produce urine all the time, but the amount of urine you produce depends on how much you drink, eat and sweat.
A healthy bladder can hold one and a half to two cups (300-400 mls) of urine during the day and about four cups (800mls) at night. It is normal to pass urine five or six times a day and possibly once during the night if you drink between 6-8 glasses of fluid. The amount of fluid you drink will affect how often you need to pass urine. For most people the average fluid intake should be approximately 2 liters (3 and 1/2 pints) a day. It is usual to empty your bladder when you get out of bed in the morning, three times during the day, and before you go to bed at night. As you age this pattern may change, as older people tend to make more urine at night.
Your bladder should act like a balloon, which fills gradually. The outlet for the urine (the urethra) is normally kept closed. This is helped by the pelvic floor muscles beneath the bladder, which sweep around the urethra.
As your bladder fills, the need to pass urine increases. When the bladder functions normally it should be possible for you to ‘hold on’ for a suitable and convenient time to empty your bladder.
Your bladder is made up of a muscle called the ‘detrusor’. When this contracts (squeezes), the muscles in the urethra relax and your bladder will empty. Complex nerve messages are sent between the brain, bladder and the pelvic floor muscles. This influences the sensation of your bladder filling and the use of the right muscles at the right time.
Common bladder problems you may experience
- Urgency – feeling the sudden need to rush to the toilet.
- Urge incontinence – feeling the urgent need to go to the toilet and not making it in time.
- Frequency – going to the toilet often, then only passing small amounts.
Urgency and urge incontinence often occur because the bladder gets over excited and overactive.
What is an overactive bladder?
If your bladder contracts without any warning it can give you an urgent need to pass urine. This gives you little or no time to get to the toilet. This is called urinary urgency. If you have this problem you are likely to need to pass urine more frequently and in small volumes. This is because your bladder often feels fuller than it actually is. It can also cause you to get up in the night more than once to pass urine. If the contractions are large or your pelvic floor muscles are weak, an overactive bladder can cause leakage of urine. This is called urge incontinence.
For most people the cause of an overactive bladder is unknown. An overactive bladder can be a problem for many people of all ages. Other members of your family may suffer from similar symptoms. There could be a neurological cause for the problem (relating to the brain or spinal nerves) but this is uncommon. Stress can make the problem worse and the types of fluid you drink can also influence your symptoms.
How is overactive bladder diagnosed?
Urodynamics is a special test on your bladder which is used to help find out the cause of your bladder symptoms. It may show the cause of symptoms such as incontinence, urgency or difficulty emptying your bladder. If the results of the urodynamic investigation show that you have uncontrolled contractions of the bladder muscle then the diagnosis would be called detrusor over-activity.
Bladder retraining program
Every person will have different needs in regard to bladder training. The first step is to complete a three-day bladder diary to get information about your bladder function. From this your personal goals can be set. Set yourself achievable goals. For example, if you start with a break of one hour between emptying your bladder, your initial goal may be to “hang on” for 5 or 10 minutes. The aim is to gradually increase the time you can “hang-on”. Discuss appropriate goals with your doctor, Continence Nurse or Physiotherapist.
How will I know if bladder training is working?
You may not notice an improvement immediately, but gradually you will become aware of not having to go to the toilet as often, being able to stop yourself going, passing more urine each time you
go, having less urgency, and not getting up to the toilet at night time.
Bladder training takes time. You may have good and bad days. Persevere and you will eventually be the boss of your bladder.
What happens if bladder training doesn’t work?
Despite best efforts, in a few cases, the bladder will not respond to the bladder training program. In these cases, some medications, prescribed by the doctor, may assist. If you decide to take medications it is important to still continue your bladder training strategies.
Bladder diary
A bladder diary will help you record the amount of urine you pass every time you go to the toilet and every time you leak. Take a record over at least 3 days for a bladder diary. Each diary page will cover 24 hours. It will give a clearer picture of your pattern of leaking over the day and night, including any effects of fluids that are “bladder-irritants”. Keeping a diary can be helpful for your doctor or continence nurse.
When collecting urine to measure the volume passed, you will need to measure this fairly accurately. To make recording of drinks easier, note the amount that your favorite tea/coffee-cup or glass holds – use this to record your drinks in “milliliters”. You could use a good-sized measuring jug to “pee” into. Make a note of the volume for your diary before tipping its contents into the toilet. Or you may find it easier to use a large plastic container (such as an ice-cream container) and set this directly down into the toilet. Then tip the contents into the measuring jug.
Your bladder diary is all about recording four important things:
- Input (fluids drunk): Record the type or names of all fluids that you drink. Be aware that “fluids” also includes foods that are mainly liquid, such as soups, jellies and custards.
- Output: Record the amount of urine you pass over at least 3 days and nights (Make these 3 consecutive days if you can).
- Leakage: Record the amount of any leakage of urine, e.g. spot, dribble, flood, a few teaspoons, or similar description.
- Circumstances: Where you were, or what you were doing, at the time of leakage is important information, both for your own awareness and for a Continence Assessment. “Circumstances” will include whether you felt an urgent, sudden need to pass urine just before the leakage happened, or you leaked when you coughed or while lifting, or you leaked at aerobics class, for example. Perhaps you arrived home, put the key in the door and lost control before you reached the toilet? Maybe at the time you leaked you weren’t aware you were losing urine? Or perhaps you got out of bed in the morning and, as you stood up, you “lost it”.
Looking back at the entries in your bladder diary could be helpful for you anticipate problems, so you’re ready for a possible leakage episode. Perhaps there’s a problem at a particular time of the day, or overnight, or following certain drinks or foods? It can be difficult to remember every time you empty your bladder (“pee”) so writing this information down will help. Be aware that the part of the week you choose to record may be significant – your weekends may be quite different to a week-day, for example.
How to measure your urine
To measure the amount of urine you pass, put a container (like an ice cream container) in the toilet bowl. Sit on the toilet and pass urine into the container. When you have finished, measure the urine by tipping it into a measuring jug. For men, you may prefer to stand and pass urine directly into the measuring jug. You should note the measurement from the jug in your bladder diary, then tip the urine into the toilet and flush.
You can also use absorbent pads to work out how much urine you leak over one or two days. This is done by using a dry pad that has been weighed in a plastic bag. When you change the wet pad you put it back in the plastic bag and weight it. If you take away the weight of the dry pad from the weight of the wet pad you can work out how much urine you have leaked. One milliliter (ml) of urine weighs one gram.
For example:
- Wet pad = 350 grams
- Dry pad = 150 grams
Weight difference
- 200 grams
Amount leaked
- 200 mls
Bladder retraining exercises and techniques
Some techniques which may help you control your urge:
- Stop and relax – do not rush to the toilet.
- Breathe slowly and evenly.
- Perineal / Vaginal pressure:
- Sit on the arm of a chair or the edge of a desk.
- Sit on a rolled-up towel.
- Cross your legs.
- Curl your toes repeatedly or hold firmly.
- Stretch your calf muscles and hold the stretch.
- If you are walking, slow your pace and emphasize heel-toe walking.
- Press or rub the trigger point on the inside of your leg just above your ankle.
- Press or rub the trigger point at the base of your nose.
- Squeeze and lift your pelvic floor muscles – hold them tight.
- Distract yourself. Do not think about the toilet or about leaking. Distract yourself with a physical or mental task e.g. count backwards from 100 by 3’s or 7’s; think of 3 American towns starting with A, then with B, then C etc.
- When you have performed the technique, walk to the toilet in a slow and controlled manner.
Remember: Your bladder does not have eyes or ears; it cannot see the toilet nor know how far away you are. If you feel you may leak on the way it is just anxiety. Relax, stay calm and walk slowly.
Different techniques work for different people. By practicing these techniques you will find out which ones work for you. Use the above techniques to gradually increase the time between toileting and to stop getting out of bed at night when you feel the urge to go to the toilet.
Retraining your bladder
Review any lifestyle factors which may be contributing to poor bladder function, such as:
- reducing or ceasing caffeine intake (tea, coffee, cola drinks), alcohol and very sweet drinks
- not being constipated
- only going to the toilet when you need to go (not going “just-in-case”)
- drinking about 1.5L of fluid per day (mostly water) aim to regularly pass 300ml or more urine
- get rid of any cough or sneezing
- exercise your pelvic floor muscles as you have been shown
- maintain a healthy weight by walking for thirty minutes each day
- do persevere. You have the ability to make your brain the boss and retrain your bladder.
- do speak to your Physiotherapist or Continence Nurse about any concerns or problems you encounter.
It is important to have strong pelvic floor muscles (see Pelvic Floor Exercises).
Bladder retraining:
- Instead of rushing to the toilet as soon as you get the urge to pass urine, it important to try to learn to ‘hold on’. If you have an overactive bladder you may tend to go to the toilet more often than you need to, as a precaution to avoid ‘accidents’. Unfortunately, rather than helping the problem this can make it worse, as your bladder will become used to holding less urine. Your bladder then becomes more sensitive, even when there is very little urine in it to stretch it. Try to avoid ‘just in case’ visits to the toilet.
- Bladder retraining should be carried out in small stages. For example, if you find you are going to the toilet every half an hour, try extending the time (or ‘holding on’) by 10 minutes for a week, then by 15 minutes for a week, and then 30 minutes, etc.
- Ideally you should be able to hold on for 3-4 hours between toilet visits.
Learn to suppress the urgency
There are different techniques for this. What works for one person may not work for another. Here are some suggestions:
- Sit straight on a hard seat.
- Distract yourself – for example, try doing a crossword or word search puzzle; count down from 100; think of girls or boys names beginning with a certain letter; read a book or newspaper. It is important to plan in advance how you will distract yourself, so that you are prepared.
- Contract your pelvic floor muscles. Contracting these muscles may help to suppress both urgency and incontinence.
The above techniques may help you gradually, but patience is needed as it may take weeks or months before you notice a significant improvement. You will find it helpful to keep a diary of when you go to the toilet at the start of bladder training and then again a few months later. You may see more improvement than you expected.
Change your drinking habits
There are a number of drinks that may irritate the bladder. If you do have these drinks, try to have them less often or stop having them completely, to see if this helps.
Drinks which may irritate the bladder are:
- drinks containing caffeine such as tea and coffee• carbonated (fizzy) drinks
- drinks containing aspartame (an artificial sweetener, which can be found in diet drinks. It can also be labelled as E951)
- hot chocolate
- alcohol
- green tea and mint tea
- blackcurrant juice
- citrus fruit juices (e.g. orange and grapefruit).
Drinks which are believed not to irritate the bladder are:
- water (definitely not a bladder irritant)
- fruit teas
- caffeine-free tea and coffee (make sure all the caffeine has been removed). However, some people’s bladders can also be irritated by de-caffeinated drinks. Try de-caffeinated drinks for a month to see if this improves your symptoms.
- milk
- diluted fruit juice.
Many people with an overactive bladder reduce the amount they drink. However, this can make the problem worse, as the bladder then never gets full and so loses the ability to stretch. Also, the urine becomes concentrated, which can irritate the bladder even further. Aim to drink 1.5 to 2 liters a day (although this amount will vary depending on the weather, your activity levels and your weight. You need to drink a certain amount of fluid for your weight; your healthcare team will talk about this with you).
Medications
Medicines that may help. There are various medicines that you can try. They work for some people, but not all. It’s worth trying them for one to two months before deciding if they are suitable for you. If they do work, they will work best alongside the bladder techniques described here. You can continue to take them for as long as you need them.
The medicines are called antimuscarinics (anticholinergics) or a newer medication called mirabegron (Betmiga). Antimuscarinics work by blocking certain nerve impulses to the bladder, which stops it contracting and helps it to hold on to more urine. They need to be taken for at least 4 weeks to notice any benefit.
Mirabegron relaxes the bladder muscle. This reduces the activity of an overactive bladder and treats urge and urge incontinence. It starts to work about eight weeks after you begin taking it.
You may need to try different medicines to find one that works best for you. All medicines have possible side effects. The most common side effects from antimuscarinics are a dry mouth and constipation. Ask your doctor or specialist nurse for more information on side effects and make sure they know your medical history before recommending the medicines.
There is another form of therapy using a bacterial toxin (Botox) which can help an overactive bladder. However, it is an invasive procedure involving injections into the bladder and is only performed as a last resort. This would need to be discussed carefully with your doctor or specialist nurse.
Medications that may make the problem worse
If you take diuretics (water tablets) they can make you pass more urine, so it may be worth changing the time you take them. For example, don’t take them late at night as you will pass urine a lot during the night. However, you may not wish to take them in the morning if that is the time of day when you want to go out. Speak to your doctor before you change the pattern of taking your diuretics.
Other medicines can also adversely affect your bladder. Your doctor or specialist nurse will be able to give you more specific information.
Pelvic Floor Exercises
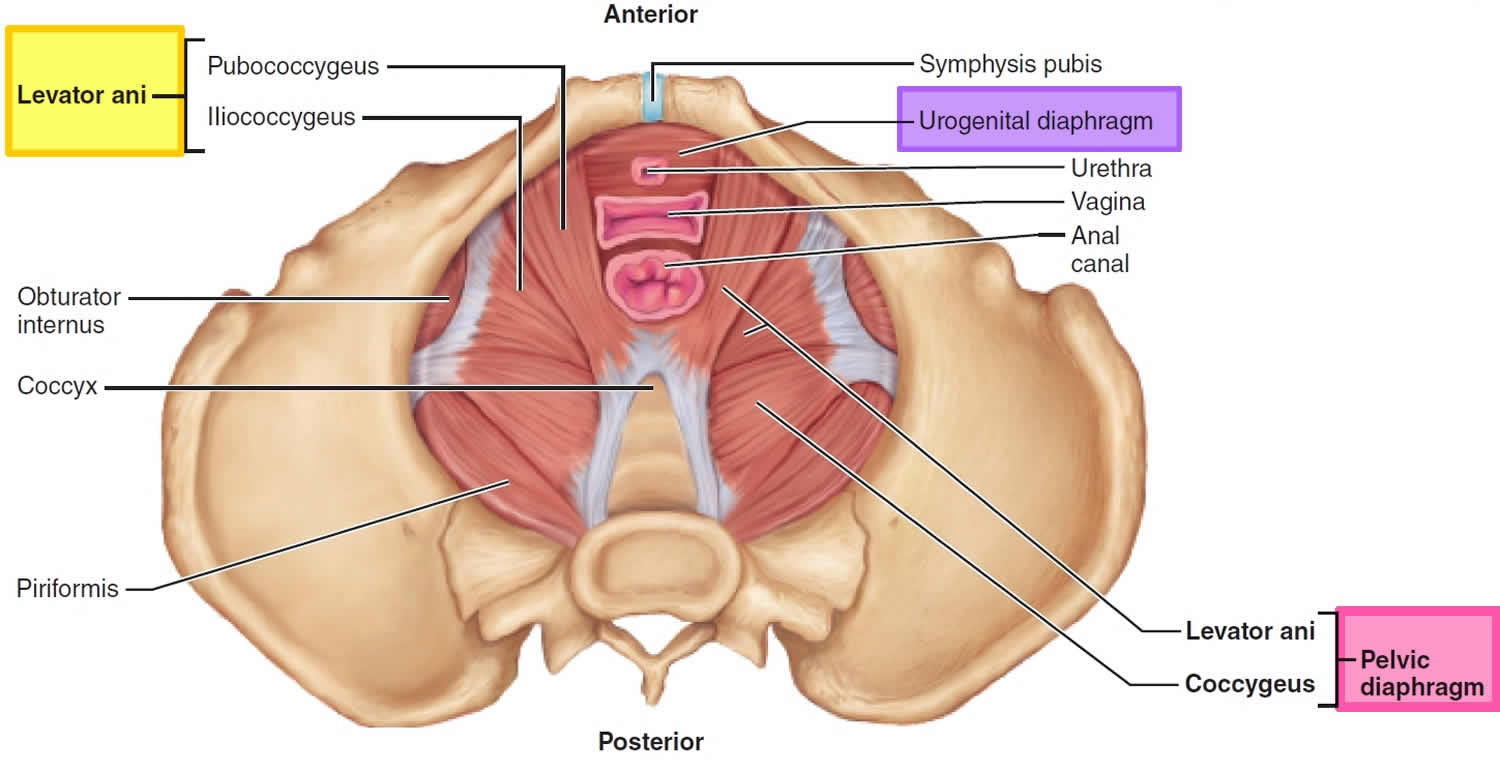
Pelvic floor muscle training exercises also called Kegel exercises, are exercises to make your pelvic floor muscles stronger. The pelvic floor are the muscles that hold up your bladder, rectum and uterus (womb) and help keep them from prolapsing (a condition where organs fall down or slip out of place), resulting in urinary or fecal leakage (incontinence).
Kegel exercises (pelvic floor muscle training exercises) can help both men and women who have problems with urine leakage or bowel control. Kegel exercises (pelvic floor muscle training exercises) can also make sex better.
Building up your pelvic muscles with Kegel exercises (pelvic floor muscle training exercises) can help with your bladder and bowel control. Kegel exercises strengthen the pelvic muscles — the muscles under the uterus, bladder, and bowel (large intestine) and don’t require any equipment. Once you learn how to do “Kegel exercises” you can Kegel anywhere. You can do Kegel exercises while lying down, sitting at a desk, or standing up.
The trick is finding the right muscles to squeeze (see Figures 1 and 2 for reference). Your doctor or nurse can help make sure you are squeezing the right muscles. Your doctor may refer you to a specially trained physical therapist who will teach you to find and strengthen the sphincter muscles. Learning when to squeeze these muscles can also help stop the bladder spasms that cause urge incontinence. After about 6 to 8 weeks, you should notice that you have fewer leaks and more bladder control.
To do Kegel exercises, you just squeeze your pelvic floor muscles. The part of your body including your hip bones is the pelvic area. At the bottom of the pelvis, several layers of muscle stretch between your legs. The muscles attach to the front, back, and sides of the pelvic bone (see Figures 4 and 5). Pelvic floor exercises are designed to make your pelvic floor muscles stronger. These are the muscles that hold up your bladder and help keep it from leaking.
A pelvic floor muscle training exercise is like pretending that you have to urinate, and then holding it. You relax and tighten the muscles that control urine flow. It is important to find the right muscles to tighten.
Find the right muscles. Try one of the following ways to find the right muscles to squeeze.
- Imagine that you are trying to stop passing gas. Squeeze the muscles you would use. If you sense a “pulling” feeling, you are squeezing the right muscles for pelvic exercises.
- Imagine that you are sitting on a marble and want to pick up the marble with your vagina. Imagine “sucking” the marble into your vagina.
- Lie down and put your finger inside your vagina. Squeeze as if you were trying to stop urine from coming out. If you feel tightness on your finger, you are squeezing the right pelvic muscles.
The next time you have to urinate, start to go and then stop. Feel the muscles in your vagina, bladder, or anus get tight and move up. These are the pelvic floor muscles. If you feel them tighten, you have done the exercise right.
If you are still not sure whether you are tightening the right muscles, keep in mind that all of the muscles of the pelvic floor relax and contract at the same time. Because these muscles control the bladder, rectum, and vagina, the following tips may help:
- Women: Insert a finger into your vagina. Tighten the muscles as if you are holding in your urine, then let go. You should feel the muscles tighten and move up and down.
- Men: Insert a finger into your rectum. Tighten the muscles as if you are holding in your urine, then let go. You should feel the muscles tighten and move up and down. These are the same muscles you would tighten if you were trying to prevent yourself from passing gas.
It is very important that you keep the following muscles relaxed while doing pelvic floor muscle training exercises:
- Abdominal
- Buttocks (the deeper, anal sphincter muscle should contract)
- Thigh
If you’re having trouble doing Kegel exercises, don’t be embarrassed to ask for help. Your doctor or other health care provider can give you important feedback so that you learn to isolate and exercise the correct muscles.
In some cases, vaginal weighted cones or biofeedback might help. A woman can also strengthen these muscles by using a vaginal cone, which is a weighted device that is inserted into the vagina. To use a vaginal cone, you insert it into your vagina and use pelvic muscle contractions to hold it in place during your daily activities. During a biofeedback session, your doctor or other health care provider inserts a pressure sensor into your vagina or rectum. As you relax and contract your pelvic floor muscles, a monitor will measure and display your pelvic floor activity.
If you are unsure whether you are doing the pelvic floor muscle training correctly, you can use biofeedback and electrical stimulation to help find the correct muscle group to work.
- Biofeedback is a method of positive reinforcement. Electrodes are placed on the abdomen and along the anal area. Some therapists place a sensor in the vagina in women or anus in men to monitor the contraction of pelvic floor muscles.
- A monitor will display a graph showing which muscles are contracting and which are at rest. The therapist can help find the right muscles for performing pelvic floor muscle training exercises.
Let your doctor, nurse, or therapist help you. Many people have trouble finding the right muscles. Your doctor, nurse, or therapist can check to make sure you are doing the exercises correctly. You can also exercise by using special weights or biofeedback. Ask your health care team about these exercise aids.
Don’t squeeze other muscles at the same time. Be careful not to tighten your stomach, legs, or other muscles. Squeezing the wrong muscles can put more pressure on your bladder control muscles. Just squeeze the pelvic muscle. Don’t hold your breath.
Repeat, but don’t overdo it. At first, find a quiet spot to practice—your bathroom or bedroom—so you can concentrate. Lie on the floor. Pull in the pelvic muscles and hold for a count of 3. Then relax for a count of 3. Work up to 10 to 15 repeats each time you exercise. Use the Exercise Log below to keep track of your sessions.
Do your pelvic exercises at least three times a day. Every day, use three positions: lying down, sitting, and standing. You can exercise while lying on the floor, sitting at a desk, or standing in the kitchen. Using all three positions makes the muscles strongest.
Be patient. Don’t give up. It’s just 5 minutes, three times a day. You may not feel your bladder control improve until after 3 to 6 weeks. Still, most women do notice an improvement after a few weeks.
Performing Pelvic Floor Exercises
- Begin by emptying your bladder.
- Tighten the pelvic floor muscles and hold for a count of 10.
- Relax the muscles completely for a count of 10.
- Do 10 repetitions, 3 to 5 times a day (morning, afternoon, and night).
You can do these exercises at any time and place. Most people prefer to do the exercises while lying down or sitting in a chair. After 4 to 6 weeks, most people notice some improvement. It may take as long as 3 months to see a major change.
After a couple of weeks, you can also try doing a single pelvic floor contraction at times when you are likely to leak (for example, while getting out of a chair).
A word of caution: Some people feel that they can speed up the progress by increasing the number of repetitions and the frequency of exercises. However, over-exercising can instead cause muscle fatigue and increase urine leakage.
If you feel any discomfort in your abdomen or back while doing these exercises, you are probably doing them wrong. Breathe deeply and relax your body when you do these exercises. Make sure you are not tightening your stomach, thigh, buttock, or chest muscles.
When done the right way, pelvic floor muscle exercises have been shown to be very effective at improving urinary continence.
There are physical therapists specially trained in pelvic floor muscle training. Many people benefit from formal physical therapy.
Pelvic Floor Exercises Log
Week: ______________
My Pelvic Muscle Exercise Log
Sunday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Monday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Tuesday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Wednesday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Thursday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Friday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Saturday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Use this sheet as a master for making copies that you can use to record your exercises week after week.
Muscles of the pelvic floor
The pelvic floor also called the pelvic diaphragm (Figures 4 and 5), is a complex layer of muscles and ligaments which stretches like a hammock from the pubic bone at the front of your pelvis to the coccyx at the bottom your spine.
The pelvic floor is a sheet consisting of two muscles, the levator ani and the small coccygeus (ischiococcygeus). The pelvic floor supports the pelvic organs, seals the inferior opening of the bony pelvis, and lifts superiorly to help release feces during defecation. The pelvic floor is pierced by the rectum and urethra (the tube for urine) and (in females) by the vagina.
The muscles of the pelvic floor are the levator ani and ischiococcygeus. Along with the fascia covering their internal and external surfaces, these muscles are referred to as the pelvic diaphragm, which stretches from the pubis anteriorly to the coccyx posteriorly, and from one lateral wall of the pelvis to the other. This arrangement gives the pelvic diaphragm the appearance of a funnel suspended from its attachments. The pelvic diaphragm separates the pelvic cavity above from the perineum below. The anal canal and urethra pierce the pelvic diaphragm in both sexes, and the vagina also goes through it in females. The three components of the levator ani muscle are the pubococcygeus, puborectalis, and iliococcygeus. Figure 1 shows these muscles in the female and Figure 2 illustrates them in the male. The levator ani is the largest and most important muscle of the pelvic floor. It supports the pelvic viscera and resists the inferior thrust that accompanies increases in intraabdominal pressure during functions such as forced exhalation, coughing, vomiting, urination, and defecation. The muscle also functions as a sphincter at the anorectal junction, urethra, and vagina. In addition to assisting the levator ani, the ischiococcygeus pulls the coccyx anteriorly after it has been pushed posteriorly during defecation or childbirth.
The body region inferior to the pelvic floor is the perineum. In the anterior half of the perineum is a triangular sheet of muscle called the urogenital diaphragm. It contains the external urethral sphincter muscle, which surrounds the urethra. You use this muscle voluntarily to prevent urination. Just inferior to the urogenital diaphragm is the superficial perineal space, which contains muscles (bulbospongiosus, ischiocavernosus) that help maintain erection of the penis and clitoris. In the posterior half of the perineum, circling the anus, lies the external anal sphincter. This muscle is used voluntarily to prevent defecation. Just anterior to this sphincter, at the exact midpoint of the perineum, is the central tendon. Many perineal muscles insert on this strong tendon and, in so doing, are able to support the heavy organs in the pelvis.
The pelvic floor has several functions:
- it supports your pelvic and abdominal organs, especially when you are standing or straining;
- it helps your urethra stay closed when you cough, sneeze or strain;
- it controls leakage of wind or motions from your lower bowel;
- it helps to heighten sexual awareness by tightening during intercourse.
A weak pelvic floor gives you less control so that you may have urinary stress incontinence (urine leakage) or fecal incontinence (fecal leakage) when you exercise, lift, cough, laugh hard or sneeze.
Often women leak urine when they are pregnant or after they have given birth.
Female athletes of all ages sometimes have urine leakage during strenuous sports activities.
A man’s pelvic floor muscles support the bladder and bowel and affect sexual function. Kegel exercises can help strengthen these muscles.
The pelvic floor muscles can be weakened by:
- operations on your prostate gland (in men);
- pregnancy and childbirth (in women);
- operations on other organs within the pelvis (e.g. the bowel);
- damage to the nerves of your pelvic floor muscles (by disease, injury, surgery or radiotherapy);
- repeated straining to empty your bowels, usually due to constipation;
- a chronic cough such as a smoker’s cough, chronic bronchitis or asthma;
- being overweight;
- lack of general fitness;
- ageing;
- lack of exercise and the menopause.
Figure 4. Pelvic floor female
Figure 5. Pelvic floor male
Pelvic Floor Exercises for men
Pelvic floor exercises are an important part of preparation before surgery for removal of your prostate for cancer (radical prostatectomy) 1). They ensure that the pelvic floor muscles are in good condition and can help reduce urine leakage after the operation.
How do I contract the pelvic floor muscles?
The first thing you need to do is to identify the muscles to exercise. You can do this by sitting or lying comfortably with the muscles of your thighs, buttock and abdomen relaxed.
Step 1
Tighten the ring of muscle around the back passage as if you are trying to control diarrhea or wind. Relax the muscle again. Practice this movement several times until you are sure you are exercising the correct muscles. Try not to squeeze your buttocks, thighs or abdominal (tummy) muscles
Step 2
Imagine you are trying to pass urine, stop the flow in mid-stream and then re-start it. If your technique is correct, you will feel the base of your penis move upwards slightly towards your tummy. You can check this “for real” while passing urine, but no more than once a week, in case it interferes with normal bladder emptying
How do I do pelvic floor exercises?
Learning how to do these exercises can take a little time but, with practice, you should be able to learn the technique:
- tighten and draw in the muscles around the anus (back passage) and the urethra (water pipe) all at once. Lift them up inside you and hold this position as you count to five. Release the muscles slowly and relax for a few seconds
- repeat the contraction and relax again. Once you find it easy to hold the contraction for a count of five, try to hold it for longer (up to ten seconds)
- repeat this for a maximum of eight to ten squeezes. Try to make each contraction strong, slow and controlled
- do the same thing again but, this time, using ten short, fast contractions, pulling up rapidly and immediately letting go
- repeat this whole exercise routine at least four to five times every day. You can do it in a variety of positions – lying, sitting, standing and walking
- try to avoid holding your breath, pushing down (instead of squeezing) and tightening your abdominal muscles, buttocks or thighs
- the exercises can be performed standing, sitting or lying down but you may find it easier at first to do them sitting down
Other things that help
Once you have learnt how to do these exercises, they should be done regularly, giving each set your full attention. Find at least five regular times during the day to do them e.g. after going to the toilet, when having a drink, when lying in bed. Tightening the pelvic floor before you cough, lift anything heavy or get up from a chair will also help.
You will probably not notice an improvement for several weeks. It may take a few months before you get maximum benefit. Once you have recovered control over your bowel and bladder, continue doing the exercises twice a day for life, to keep the pelvic floor muscles strong.
When to do your Kegel exercises
Make Kegel exercises part of your daily routine. For example:
- Fit in a set of Kegel exercises every time you do a routine task, such as brushing your teeth.
- Do another set after you urinate, to get rid of the last few drops of urine.
- Contract your pelvic floor muscles just before and during any activity that puts pressure on your abdomen, such as sneezing, coughing, laughing or heavy lifting.
Other things to do include:
- Share the lifting of heavy loads;
- Avoid constipation and straining when opening your bowels;
- Seek medical advice for hay fever, asthma or bronchitis to reduce sneezing and coughing;
- Keep your weight within the correct range for your height and age; and
- Other methods which have been shown to help some men include biofeedback and electrical stimulation.
If you would like to explore other methods or you are not sure whether you are performing the exercises correctly, ask your urologist or specialist nurse. They will be able to give you more advice or put you in touch with a continence advisor or physiotherapist.
When you’re having trouble
If you’re having trouble doing Kegel exercises, don’t be embarrassed to ask for help. Your doctor or other health care provider can give you important feedback so that you learn to isolate and strengthen the correct muscles.
In some cases, biofeedback training might help. In a biofeedback session, your doctor or other health care provider inserts a small probe into your rectum. As you relax and contract your pelvic floor muscles, a monitor will measure and display your pelvic floor activity. Research suggests that biofeedback training is more effective in treating fecal incontinence.
When to expect results
If you do your Kegel exercises regularly, you can expect results — such as less frequent urine leakage — within about a few weeks to a few months. For continued benefits, make Kegel exercises a permanent part of your daily routine.
Pelvic Floor Exercises for women and pregnant mothers
If you’re pregnant or planning to get pregnant, you can start doing pelvic floor exercises straight away. Kegel exercises will lower your risk of experiencing incontinence after having your baby. The more active and fit you are during pregnancy, the easier it will be for you to adapt to your changing shape and weight gain. It will also help you to cope with labor and get back into shape after the birth. Exercise is not dangerous for your baby – there is some evidence that active women are less likely to experience problems in later pregnancy and labor.
Kegel exercises help to strengthen the muscles of the pelvic floor, which come under great strain in pregnancy and childbirth. The pelvic floor consists of layers of muscles that stretch like a supportive hammock from the pubic bone (in front) to the end of the backbone (see Figure 1 above).
If your pelvic floor muscles are weak, you may find that you leak urine when you cough, sneeze, laugh or strain. This is quite common and you needn’t feel embarrassed. It’s known as stress incontinence and it can continue after pregnancy.
You can strengthen the muscles by doing pelvic floor exercises. This helps to reduce or avoid stress incontinence after pregnancy. All pregnant women should do Kegel exercises, even if you’re young and not suffering from stress incontinence now.
It is not easy to identify your pelvic floor muscles. Exercising them should not be visible from the outside. Read the section above on “How do you do Kegel exercises.” The steps are essentially the same because doing Kegel exercise (pelvic floor muscle training exercise) is simple. However, if you’re still unsure about what to do, let your doctor, nurse, or therapist help you. Many people have trouble finding the right muscles. Your doctor, nurse, or therapist can check to make sure you are doing the exercises correctly. You can also exercise by using special weights or biofeedback. Ask your health care team about these exercise aids.
Don’t squeeze other muscles at the same time. Be careful not to tighten your stomach, legs, or other muscles. Squeezing the wrong muscles can put more pressure on your bladder control muscles. Just squeeze the pelvic muscle. Don’t hold your breath.
Here is what to do 2):
Step 1
Sit comfortably with your knees slightly apart. Imagine that you are trying to stop yourself passing wind from your bowel. To do this, you must squeeze the muscle around the back passage. Try lifting and squeezing the muscle as if you have wind. If you sense a “pulling” feeling, you are squeezing the right muscles for pelvic exercises. You should be able to feel the muscle move and your buttocks or legs should not move at all. You should notice that the skin around your back passage tightens up and creates the sensation of lifting you from your chair.
Step 2
Imagine that you are sitting on the toilet to pass urine and try to stop yourself from producing a stream of urine. You should be using the same group of muscles that you used before but you will find this a little more difficult. Do not try to stop the urinary stream when you are actually passing water because it can cause problems with bladder emptying.
Or you can lie down and put your finger inside your vagina. Squeeze as if you were trying to stop urine from coming out. If you feel tightness on your finger, you are squeezing the right pelvic muscles.
Step 3
Try to tighten the muscles around your back passage and vagina, by lifting up inside as if you are trying to stop passing wind and urine at the same time. Do not tense your abdomen, squeeze your legs together, tighten your buttocks or hold your breath. If you can master this, most of the muscle contraction should be coming from the pelvic floor.
How do you practice the exercises?
You need to develop two types of muscle activity, slow and fast.
- to practice slow contractions
- do the exercises above and try to hold the pelvic floor tight for up to ten seconds. Rest for four seconds and then repeat the contraction as many times as you can, up to a maximum of ten
- to practice quick contractions
- draw the pelvic floor rapidly upwards and hold this for one second. Repeat up to a maximum of ten times. This will protect you against sudden leakage during coughing, laughing or exercise
- Aim to do one set of slow contractions followed by one set of fast contractions up to six times a day. Do not over-do it or the muscles will get tired. The exercises can be performed standing, sitting or lying down but you may find it easier at first to do them sitting down.
- Don’t make a habit of using Kegel exercises to start and stop your urine stream. Doing Kegel exercises while emptying your bladder can actually lead to incomplete emptying of the bladder — which increases the risk of a urinary tract infection.
Other things that help
- Get into the habit of doing your exercises regularly and linking them to everyday activities e.g. do them after emptying your bladder, while answering the telephone, standing in a queue or whenever you turn on a tap. Do your pelvic exercises at least three times a day. Every day, use three positions: lying down, sitting, and standing. You can exercise while lying on the floor, sitting at a desk, or standing in the kitchen. Using all three positions makes the muscles strongest.
- At first, find a quiet spot to practice—your bathroom or bedroom—so you can concentrate. Lie on the floor. Pull in the pelvic muscles and hold for a count of 3. Then relax for a count of 3. Work up to 10 to 15 repeats each time you exercise.
- If you are not sure you are doing the exercises correctly, insert a thumb or two fingers into the vagina and try the exercises; you should feel a gentle squeeze as the muscles contract
- Use the pelvic floor exercises to prevent leakage before you do anything which might make you leak; this way, your control will gradually improve
- Drink normally – six to eight cups (two litres) per day – avoiding caffeine and alcohol if you can
- Avoid going to the toilet “just in case”; go only when you feel that your bladder is full
- Watch your weight; extra weight puts more strain on your pelvic floor muscles and your bladder
- Avoid constipation. Straining can put excessive pressure on your bladder and bowels
- Pelvic floor exercises take three to six months to produce maximum benefit, but you should continue them for life to prevent problems recurring or worsening; you should seek help from a health professional there is little or no change in your symptoms after exercising for three months
- Other methods which help some women include weighted vaginal cones, biofeedback and electrical stimulation; consult your doctor, urologist or specialist nurse for more details
Be patient. Don’t give up. It’s just 5 minutes, three times a day. You may not feel your bladder control improve until after 3 to 6 weeks. Still, most women do notice an improvement after a few weeks.
When to do your Kegel exercises
Make Kegel exercises part of your daily routine. You can do Kegel exercises discreetly just about anytime, whether you’re sitting at your desk or relaxing on the couch.
When you’re having trouble
If you’re having trouble doing Kegel exercises, don’t be embarrassed to ask for help. Your doctor or other health care provider can give you important feedback so that you learn to isolate and exercise the correct muscles.
In some cases, vaginal weighted cones or biofeedback might help. To use a vaginal cone, you insert it into your vagina and use pelvic muscle contractions to hold it in place during your daily activities. During a biofeedback session, your doctor or other health care provider inserts a pressure sensor into your vagina or rectum. As you relax and contract your pelvic floor muscles, a monitor will measure and display your pelvic floor activity.
When to expect results
If you do Kegel exercises regularly, you can expect results — such as less frequent urine leakage — within about a few weeks to a few months. For continued benefits, make Kegel exercises a permanent part of your daily routine.
References [ + ]