Contents
Benign rolandic epilepsy
Benign rolandic epilepsy also called benign rolandic epilepsy with centrotemporal spikes or benign epilepsy of childhood with centrotemporal spikes, is the most common form of childhood epilepsy. The official modern name is “childhood epilepsy with centrotemporal spikes” or CECTS. Yet, many people still just use the term benign rolandic epilepsy to refer to this syndrome. Benign rolandic epilepsy affects 15% of children with epilepsy and can start at any time between the ages of 3 and 10. Benign rolandic epilepsy is referred to as “benign” because most children outgrow the condition by puberty. Benign rolandic epilepsy is characterized by seizures involving a part of the brain called the rolandic area (the lower portion of the central gyrus of Rolando) 1). These seizures typically begin between the ages of 3 and 12 years and occur during the nighttime 2).
The seizures that happen in benign rolandic epilepsy are usually focal seizures, which start in only one part of the brain. Seizures often start as the child is asleep or just about to wake up in the morning. They have a feeling of tingling (like pins and needles) on one side of their mouth, involving the tongue, lips, gum and inner side of their cheek. Children sometimes describe their tongue or lips as being “fizzy” or “buzzing”. The seizure may also involve the throat, which may cause the child’s speech to be unclear and therefore difficult to understand. The child may make strange throaty or gurgling noises, and it is often this which alerts parents that something may be wrong. The child often knows what they want to say but cannot speak properly.
The seizure may also cause twitching movements (called clonic movements) or a stiffness (called a tonic movement) of one side of the mouth or face. These movements may then spread to the arm and/or the leg, usually on the same side as the movements in the face.
Occasionally, the seizure activity may spread to affect both sides of the brain. When this happens, the child loses consciousness, becomes stiff and has regular, jerking movements of their arms and legs. This is called a focal to bilateral tonic-clonic seizure. The child may also be incontinent. After this seizure, the child will be sleepy and some children may sleep for a few hours.
Other features of benign rolandic epilepsy include headaches or migraines and behavioral and/or learning differences 3). Benign rolandic epilepsy is thought to be a genetic disorder because most affected individuals have a family history of epilepsy 4). Treatment for benign rolandic epilepsy may depend on the symptoms and severity in each person. Because benign rolandic epilepsy resolves on its own before adulthood, many children with benign rolandic epilepsy who have infrequent seizures that only occur at night do not take anti-epileptic drugs 5). However, there have been studies suggesting that benign rolandic epilepsy may cause lasting cognitive or behavioral problems in some people 6). Medication is more likely to be recommended in children with frequent or daytime seizures, cognitive impairment, or a learning disorder 7). Medicine can also be considered if there are very frequent discharges on the EEG in sleep. Each family must consult with their physician(s) and make their own decision about whether to treat benign rolandic epilepsy 8). The most commonly used medication is levetiracetam (Keppra). Other medicines including oxcarbazepine, carbamazepine, gabapentin, zonisamide or lacosamide (Vimpat) may also be used. In most cases, seizures respond well to antiseizure medications.
Benign rolandic epilepsy accounts for about 15% of all epilepsies in children. The average age when these seizures begin is about 6 to 8 years old, but they may be seen in children from age 3 to 13. They are a bit more likely to affect boys. Children with benign rolandic epilepsy generally have normal intelligence, which is not affected by the seizures. Much less commonly, children may have learning difficulties and behavioral problems during the period of time that they have seizures. The problems typically disappear once the seizures stop and the EEG (electroencephalogram) goes back to normal.
Benign rolandic epilepsy causes
The cause of benign rolandic epilepsy is unknown. Benign rolandic epilepsy is thought to be a genetic disorder. Benign rolandic epilepsy is more common in children who have close relatives with epilepsy. Studies suggest that certain regions on chromosome 11 (11p13) and chromosome 15 (15q14) may be involved in benign rolandic epilepsy, but a specific gene has not been identified 9). Although in most cases it is seen in those without any other affected family members.
Benign rolandic epilepsy symptoms
Seizures in benign rolandic epilepsy can occur when the child is awake or during sleep. Benign rolandic epilepsy typically begins between the ages of 3 and 13 years with nighttime seizures. The episodes usually begin with twitching and stiffness of one side of the face, but often progress to a generalized tonic-clonic seizure that often wakes up the individual 10). They typically are seen shortly after the child goes to sleep or just before they wake up. They can also be seen during daytime naps. There may also be a tingling feeling on one side of the mouth that involves the tongue, lips, gums and inside of the cheek 11). Seizures that begin during wakefulness involve twitching, numbness, or tingling of one side of the face or tongue. These symptoms can interfere with speech and may cause drooling. The child remains fully aware. These seizures are typically brief, lasting no more than 2 minutes in most cases, and are usually infrequent.
The seizure can also involve the throat, which may make speech unclear and difficult to understand 12). Occasionally, both sides of the body may be affected, which can lead to stiffness and jerking movements of the arms and legs, and loss of consciousness. Loss of bladder control (incontinence) may also occur 13).
Some individuals with benign rolandic epilepsy experience headaches or migraines, learning difficulties, and behavioral problems during the period of time that they have seizures. In many children, once seizures stop and brain activity returns to normal, these issues resolve 14). Children may have very few seizures and most become seizure-free by the age of 16. However, there have been studies suggesting that cognitive or behavioral problems may persist in some people 15). More studies regarding whether there is an increased chance of long-term impairments in those with benign rolandic epilepsy are needed 16).
Benign rolandic epilepsy diagnosis
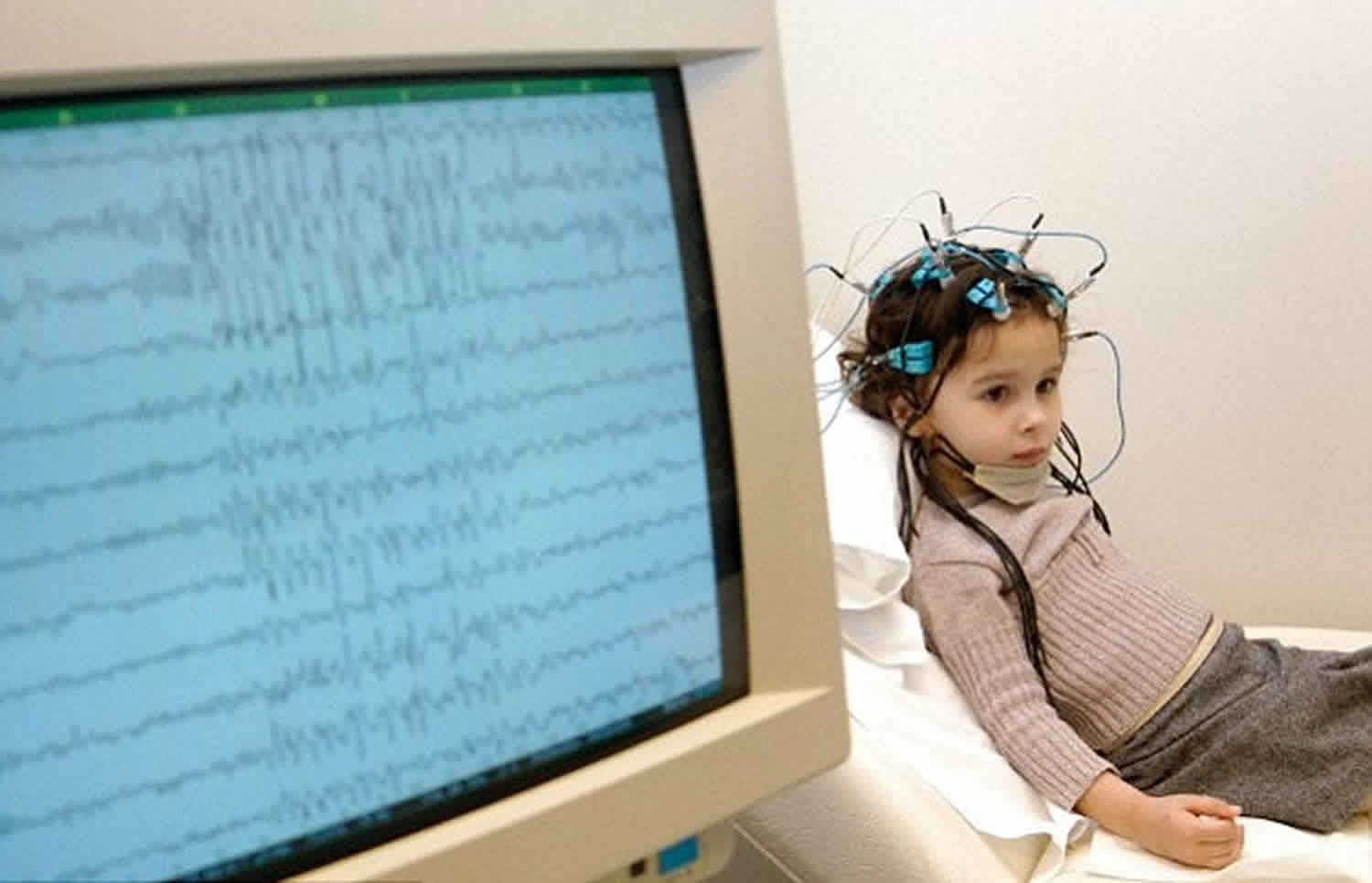
The diagnosis of benign rolandic epilepsy involves a full and accurate history of the seizure(s) and an electroencephalogram (EEG) test. The EEG records the electrical activity in the brain. In benign epilepsy of childhood with centrotemporal spikes, the EEG will pick up epileptic activity in the centro-temporal – also known as the rolandic – area of the brain. Sometimes the EEG may be normal. This doesn’t mean that the child doesn’t have this epilepsy syndrome. Occasionally, if the first EEG is normal, the hospital doctor will arrange a sleep-deprived EEG recording. This is because abnormal brain activity on the EEG is more easily seen when someone is tired or falls asleep.
Brain scans, including magnetic resonance imaging (MRI) scans are usually normal. The majority of children with a very clear and obvious history and EEG of benign rolandic epilepsy with centrotemporal spikes do not need to have an MRI brain scan.
Benign rolandic epilepsy treatment
Treatment for benign rolandic epilepsy may depend on the symptoms and severity in each person. In general, benign rolandic epilepsy typically does not require intensive therapy 17). Because seizures may be infrequent and usually occur at night, and because of the potential side affects of anti-epileptic drugs, many children with benign rolandic epilepsy do not take medication 18). However, emerging data on neuropsychological problems in people with benign rolandic epilepsy suggests that the syndrome may not be entirely without long-term effects 19). A recently recognized concern in children with benign rolandic epilepsy is a higher incidence of neuropsychological deficits 20). Each family must consult with their physician(s) and make their own decision about whether they are more comfortable treating or not treating benign rolandic epilepsy 21). The need for medication is generally bigger if a child has frequent seizures, daytime seizures, cognitive problems, or a learning disorder 22).
When benign rolandic epilepsy is treated, medications may include anti-epileptic drugs such as carbamazepine (Tegretol), gabapentin, levetiracetam (Keppra), lamotrigine (Lamictal), or sodium valproate (Epilim). Most children with benign rolandic epilepsy respond to a low dose of a single drug, but some have seizures that are more drug-resistant, requiring higher doses or more than one drug 23).
Benign rolandic epilepsy prognosis
Most children stop having seizures within 2 to 4 years after they begin. Nearly all children with benign rolandic epilepsy will outgrow the tendency to have seizures when they reach puberty, and nearly always before their 16th birthday. Medicines can be withdrawn under the guidance of the treating physician without seizure recurrence.
Children who have benign rolandic epilepsy do not usually have learning difficulties. However, some children will have difficulties with reading and language, and might need some support in school. Most children cope well with school work.
References [ + ]