Contents
What is Ebstein’s anomaly
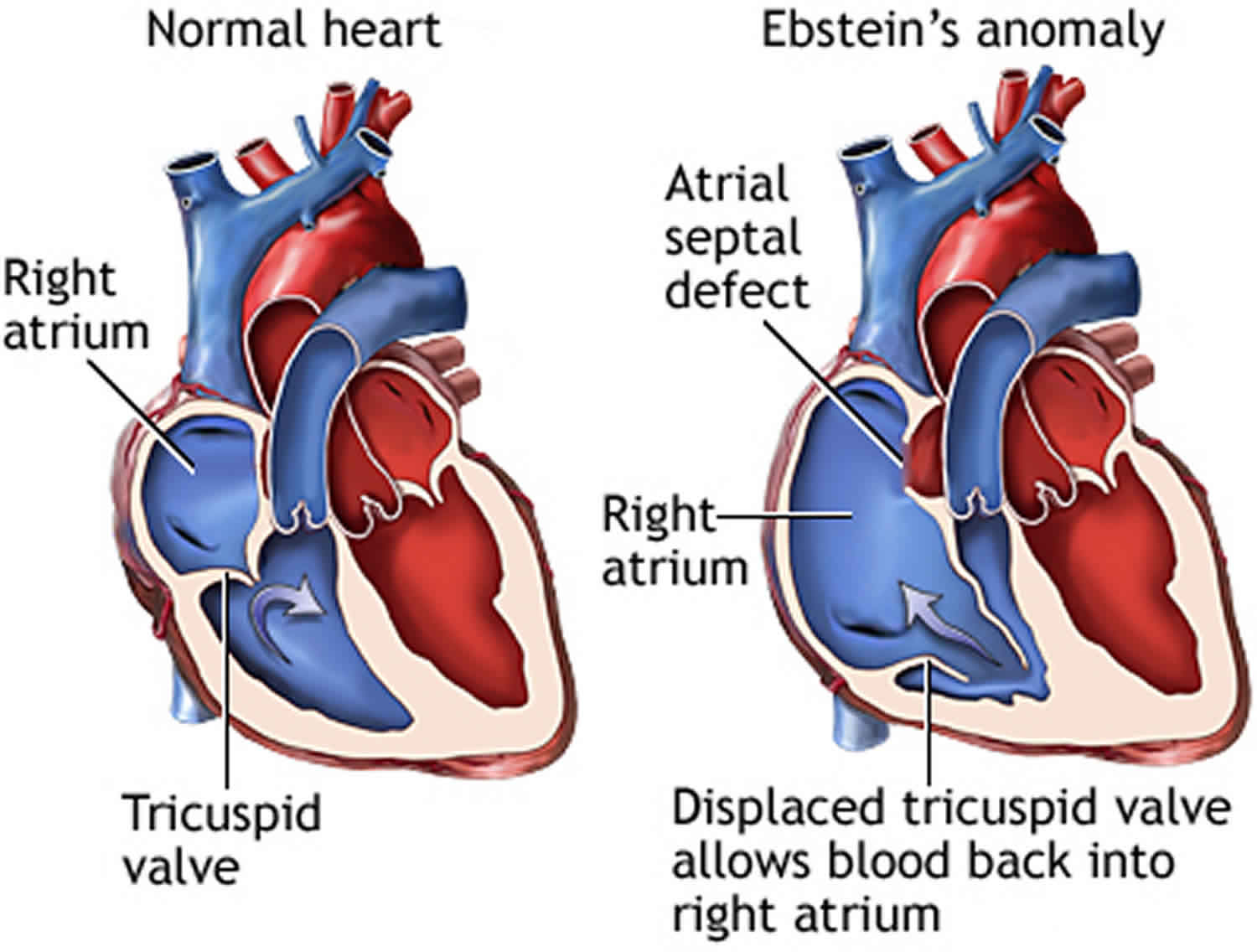
Ebstein’s anomaly is a rare heart defect where the valve on the right side of the heart (the tricuspid valve), which separates the right atrium from the right ventricle, doesn’t develop properly 1). In this condition the tricuspid valve is elongated and displaced downward towards the right ventricle. The abnormality causes the tricuspid valve to leak blood backwards into the right atrium. This means blood can flow the wrong way within the heart, and the right ventricle may be smaller and less effective than normal. The backup of blood flow can lead to heart swelling and fluid buildup in the lungs or liver. Sometimes, not enough blood gets out of the heart into the lungs and the person may appear blue. The condition is congenital, which means it is present at birth. Symptoms range from mild to very severe. Treatment depends on the severity of the defect and may include medications, oxygen therapy, or surgery.
Ebstein’s anomaly can occur on its own, but it often occurs with an atrial septal defect, pulmonic stenosis, and Wolff-Parkinson-White syndrome. It’s estimated that Ebstein’s anomaly accounts for less than 1% of congenital heart disease cases. The estimated risk of Ebstein anomaly in the general population is 1 in 20,000 live births with no predilection for either gender 2).
- Atrial septal defect. About half the people with Ebstein’s anomaly have a hole between the two upper chambers of the heart called an atrial septal defect (ASD). This hole may allow deoxygenated blood in the right atrium to mix with oxygenated blood in the left atrium, decreasing the amount of oxygen available in your blood. This causes a bluish discoloration of the lips and skin (cyanosis). The atrial septal defect associated with Ebstein’s anomaly can increase your risk of a blood clot passing from the veins in your heart into the blood vessels leading to your brain and causing a stroke. If you have surgery to repair your tricuspid valve, your surgeon will also close the atrial septal defect at the same time.
- Abnormal heartbeats (arrhythmias). Some people with Ebstein’s anomaly have an abnormal heart rhythm (arrhythmia) characterized by rapid heartbeats (tachycardia). These types of arrhythmias (tachyarrhythmias) can make your heart work less effectively, especially when the tricuspid valve is leaking severely. In some cases, a very fast heart rhythm may cause fainting spells (syncope).
- Wolff-Parkinson-White (WPW) syndrome. Some people with Ebstein’s anomaly may also have a condition known as Wolff-Parkinson-White syndrome — an abnormal electrical pathway in the heart. The presence of Wolff-Parkinson-White syndrome can lead to very fast heart rates and fainting spells.
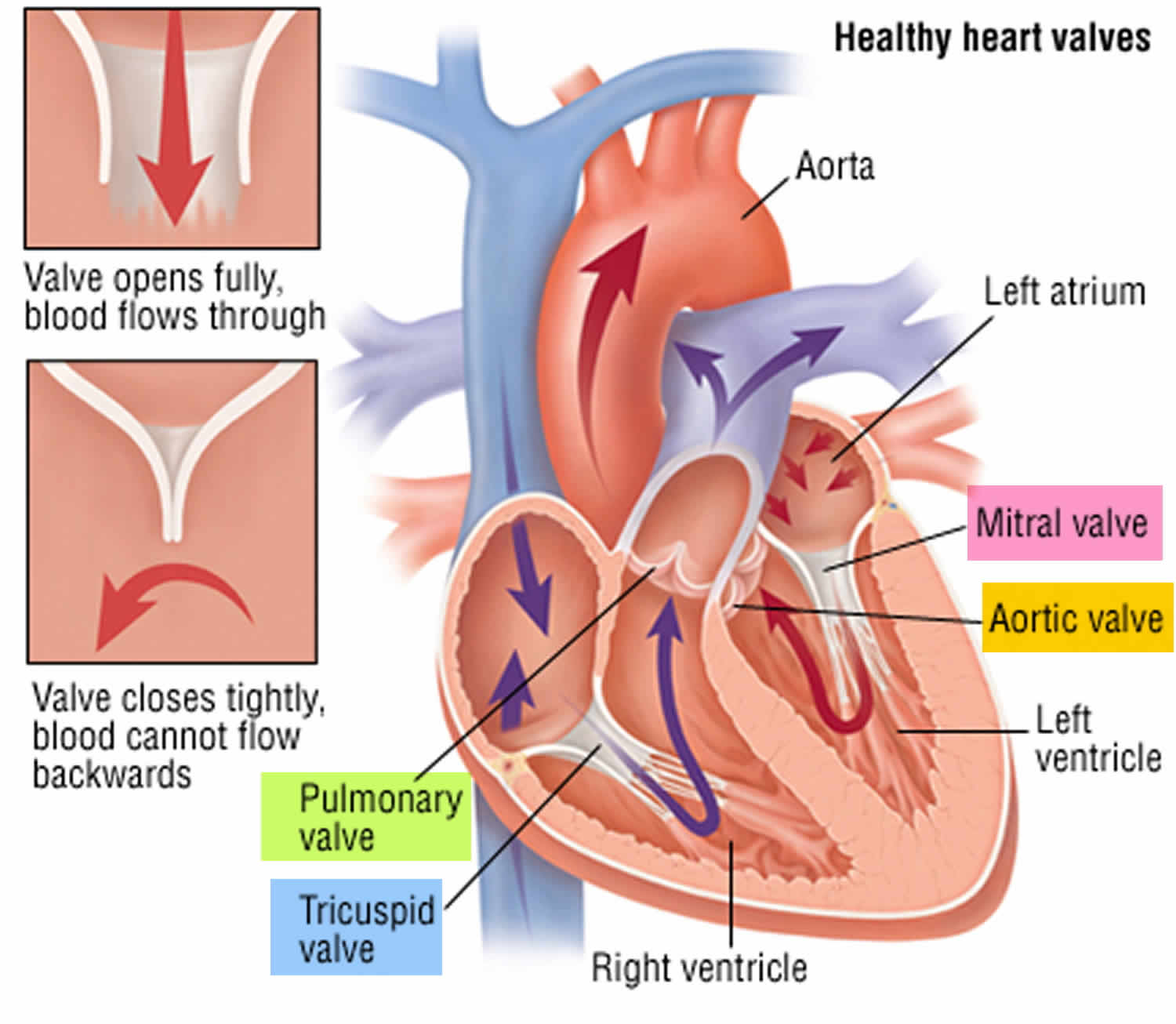
The tricuspid valve is normally made of three parts, called leaflets or flaps. The leaflets open to allow blood to move from the right atrium (top chamber) to the right ventricle (bottom chamber) while the heart relaxes. They close to prevent blood from moving from the right ventricle to the right atrium while the heart pumps.
In persons with Ebstein anomaly, the leaflets are placed deep in the right ventricle instead of the normal position. The leaflets are often larger than normal. The defect most often causes the valve to work poorly, and blood may go the wrong way. Instead of flowing out to the lungs, the blood flows back into the right atrium. The backup of blood flow can lead to heart enlargement and fluid buildup in the body. There may be narrowing of the valve that leads to the lungs (pulmonary valve). Newborns who have a severe leakage across the tricuspid valve will have a very low level of oxygen in their blood and significant heart enlargement. The health care provider may hear abnormal heart sounds, such as a murmur, when listening to the chest with a stethoscope.
In many cases, patients also have a hole in the wall separating the heart’s two upper chambers (atrial septal defect) and blood flow across this hole may cause oxygen-poor blood to go to the body. This can cause cyanosis, a blue tint to the skin caused by oxygen-poor blood.
Ebstein anomaly occurs as a baby develops in the womb. The exact cause is unknown. The use of certain drugs (such as lithium or benzodiazepines) during pregnancy may play a role. The condition is rare. It is more common in white people.
There is a remarkably wide spectrum of presentation, ranging from severely cyanotic newborns to cardiomegaly with mild cyanosis in childhood to a previously asymptomatic adult presenting with atrial arrhythmias or reentry supraventricular tachycardia. The onset of symptoms depends on the degree of tricuspid valve anatomic and functional derangement and presence of accessory pathways (e.g, Wolff-Parkinson-White syndrome). When symptoms result from a severely dysfunctional tricuspid valve, surgical repair should be considered.
If you have no signs or symptoms associated with Ebstein’s anomaly, careful monitoring of your heart may be all that’s necessary. If signs and symptoms bother you, or if the heart is enlarging or becoming weaker, treatment for Ebstein’s anomaly may be necessary. Treatment options include medications and surgery.
What activities will my child be able to do?
If valve leakage is mild and tests show no abnormal heart rhythms, your child can usually participate in most sports. Your cardiologist may recommend avoiding certain intense competitive sports. Ask your child’s cardiologist which activities are appropriate.
What problems might my child have?
Children with Ebstein’s anomaly may have a rapid heart rhythm called supraventricular tachycardia (SVT) often as a result of a condition called Wolf-Parkinson-White syndrome (WPW). An episode of supraventricular tachycardia (SVT) may cause palpitations (older children may feel your heart racing). Sometimes this is associated with fainting, dizziness, lightheadedness or chest discomfort. Infants may be unusually fussy or have other symptoms that can’t easily be connected with rapid heart rhythm. If you child has had these symptoms, contact your doctor. If your symptoms persist, seek immediate attention. Recurrent supraventricular tachycardia (SVT) may be prevented with medicines. In many cases, the source of the abnormal heart rhythm may be removed by a catheter procedure called radiofrequency ablation.
If the valve abnormality is especially severe, you may have decreased stamina, fatigue, cyanosis, and sometimes fluid retention. Infants may not feed or grow normally. The symptoms may respond to medicines such as diuretics. In some instances surgery (described above) may be recommended.
Figure 1. Ebstein’s anomaly of the tricuspid valve
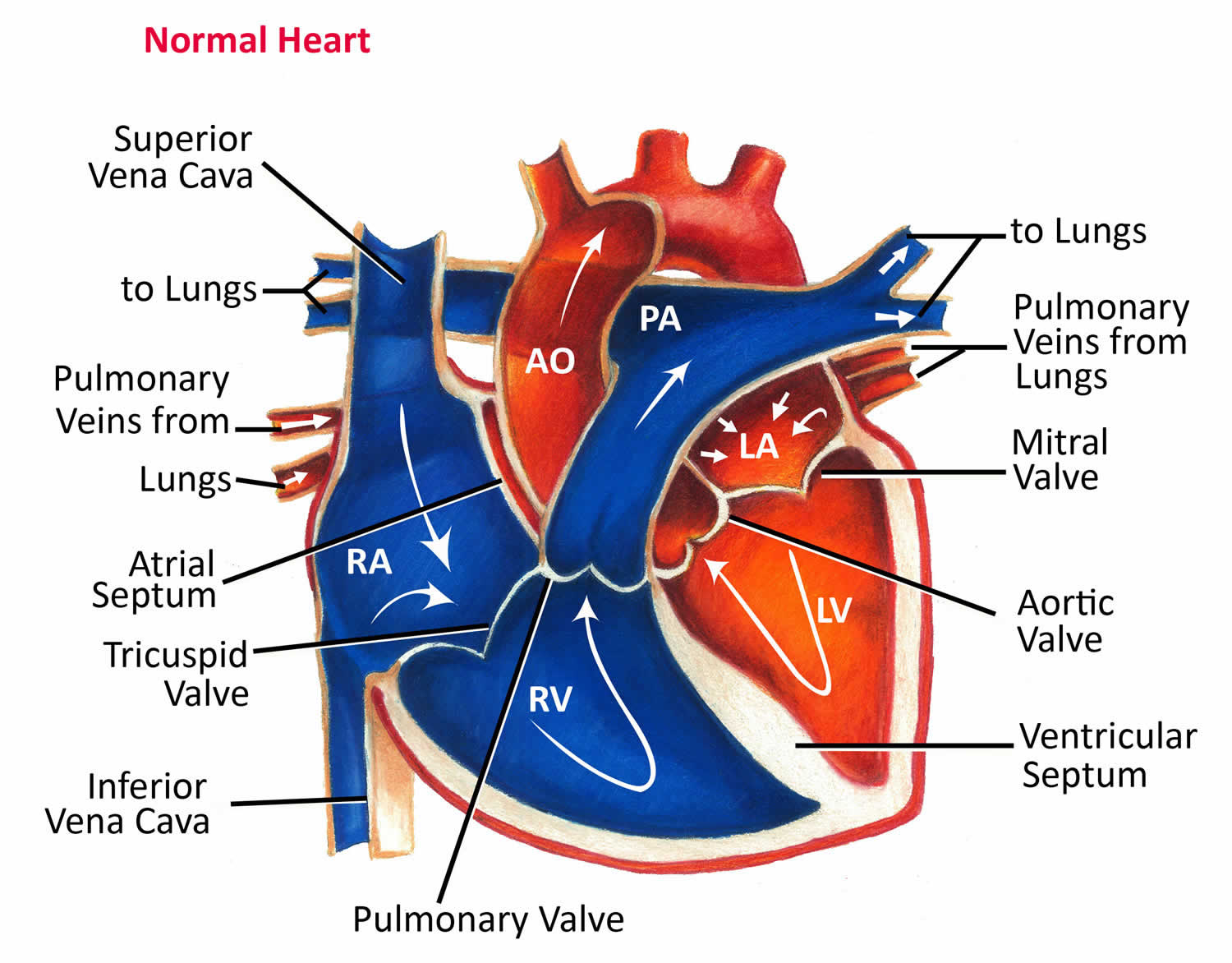
Heart valves
Your heart is a strong muscle about the size of the palm of your hand. Your body depends on the heart’s pumping action to deliver oxygen- and nutrient-rich blood to the body’s cells. When the cells are nourished properly, the body can function normally. Just like an engine makes a car go, the heart keeps your body running. The heart has two pumps separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen-rich blood from the lungs and pumps it to the body.
The heart has four chambers 3), two on the right and two on the left:
- Two upper chambers are called atrium (two is called an atria). The atria collect blood as it flows into the heart.
- Two lower chambers are called ventricles. The ventricles pump blood out of the heart to the lungs or other parts of the body.
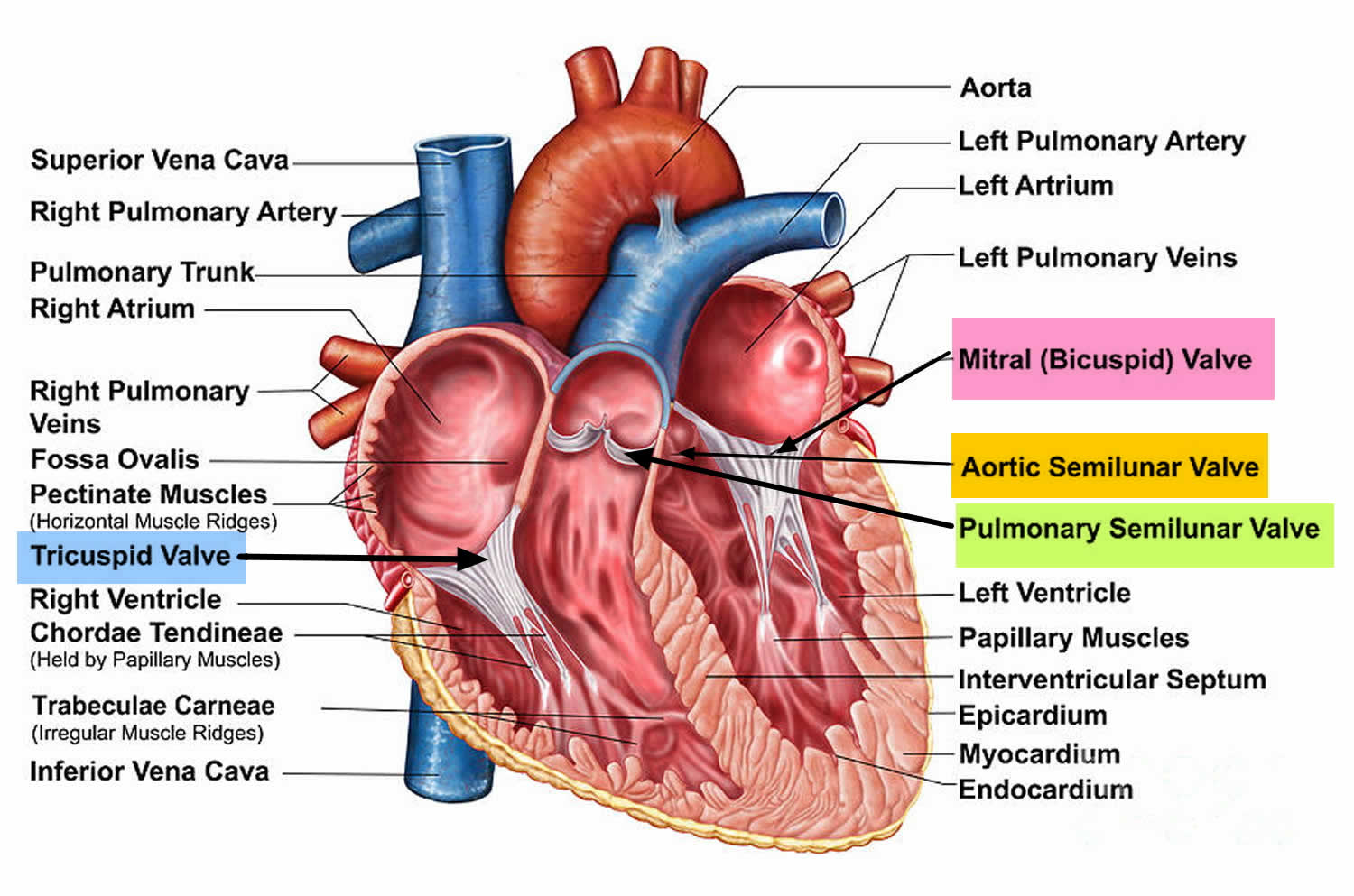
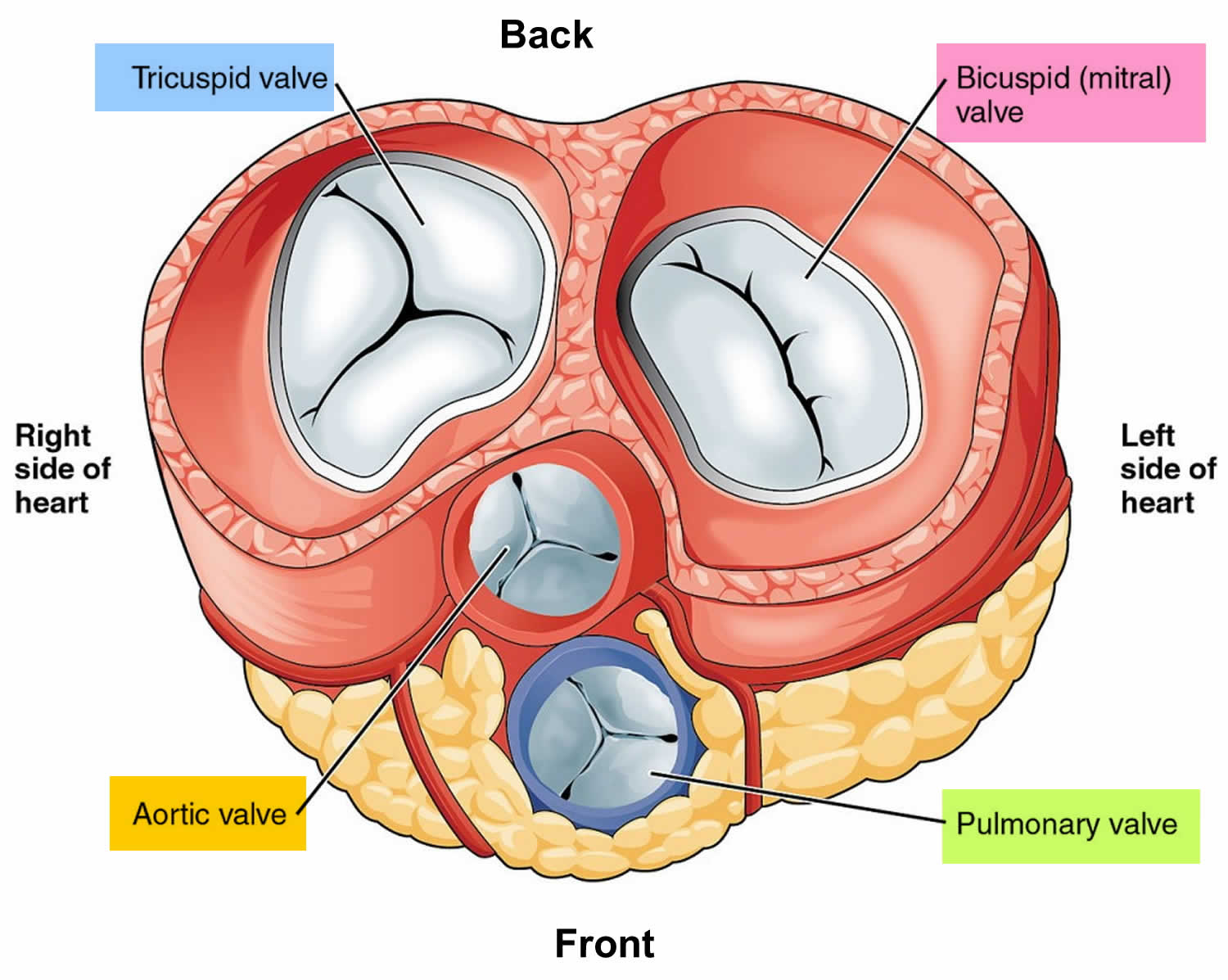
The heart also has four valves that open and close to let blood flow from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart in only one direction when the heart contracts (beats). The four heart valves are:
- Tricuspid valve, located between the right atrium and right ventricle
- Pulmonary or pulmonic valve, between the right ventricle and the pulmonary artery. This artery carries blood from the heart to the lungs.
- Mitral valve, between the left atrium and left ventricle
- Aortic valve, between the left ventricle and the aorta. This aorta carries blood from the heart to the body.
Each valve has a set of flaps (also called leaflets or cusps). The mitral valve has two flaps; the others have three. Valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward. Blood flow occurs only when there’s a difference in pressure across the valves, which causes them to open. Under normal conditions, the valves permit blood to flow in only one direction.
The heart four chambers and four valves and is connected to various blood vessels. Veins are blood vessels that carry blood from the body to the heart. Arteries are blood vessels that carry blood away from the heart to the body.
The heart pumps blood to the lungs and to all the body’s tissues by a sequence of highly organized contractions of the four chambers. For the heart to function properly, the four chambers must beat in an organized way.
When the heart’s valves open and close, they make a “lub-DUB” sound that a doctor can hear using a stethoscope 4).
- The first sound—the “lub”—is made by the mitral and tricuspid valves closing at the beginning of systole. Systole is when the ventricles contract, or squeeze, and pump blood out of the heart.
- The second sound—the “DUB”—is made by the aortic and pulmonary valves closing at the beginning of diastole. Diastole is when the ventricles relax and fill with blood pumped into them by the atria.
Figure 2. The anatomy of the heart valves
Figure 3. Top view of the 4 heart valves
Figure 4. Normal heart blood flow
Figure 5. Heart valves function
Ebstein’s anomaly in adults
Because the tricuspid valve is malformed in Ebstein’s anomaly, it often doesn’t work properly and may leak. If the valve leaks, some of the blood pumped by the right ventricle goes backwards through the valve with each heartbeat. This may result in significant enlargement of the right atrium. In more extreme cases the size of the right ventricle is too small to allow for enough blood to go to the lungs.
If the leakage of the tricuspid valve is moderate or severe, symptoms including exercise intolerance and swelling of the abdomen and legs may develop. Heart rhythm problems may also occur. In extreme cases when the right ventricle is underformed, babies may be very blue. In these cases, patients may have required surgeries similar to patients with single ventricles.
Ebstein’s anomaly is mild in most adults who have it, so they don’t need surgery. But sometimes the tricuspid valve leaks severely enough to result in heart failure or cyanosis. Then surgery may be required. Several different operations have been used in patients with Ebstein’s anomaly. The most common involves a repair of the tricuspid valve. The valve can’t be made normal, but often surgery significantly reduces the amount of leaking. In some cases the tricuspid valve can’t be adequately repaired. Then it’s replaced with an artificial valve. If there’s an atrial septal defect, it’s usually closed at the same time. In some patients, the atrial septal defect is the main problem and can be closed either with a device or with surgery.
People with Ebstein’s anomaly may have a rapid heart rhythm called supraventricular tachycardia (SVT). An episode of SVT may cause palpitations. (You feel your heart racing.) Sometimes this is associated with fainting, dizziness, lightheadedness or chest discomfort. If you have these symptoms, contact your doctor. If your symptoms persist, seek immediate attention. Recurrent SVT may be prevented with medicines. In many cases, the source of the abnormal heart rhythm may be treated by a catheter procedure called radiofrequency ablation.
If the valve abnormality is especially severe, you may have decreased stamina, fatigue, cyanosis and sometimes fluid retention. These problems usually develop because the valve has become leakier. If you have these symptoms, contact your cardiologist. The symptoms may respond to medicines such as diuretics, which cause you to lose excess fluid. In some instances surgery may be recommended.
Ebstein’s anomaly life expectancy
In general, the earlier symptoms develop, the more severe the disease. The earlier that heart failure or abnormal rhythms begin, the more serious is the condition. Some patients may have either no symptoms or very mild symptoms. Others may worsen over time, developing blue coloring (cyanosis), heart failure, heart block, or dangerous heart rhythms.
For those children diagnosed after one year of life, the outcome is usually very good with people living normal lives. Of course they will have to see a cardiologist for routine exams, echocardiograms and medication management. Depending on how leaky the valve is, your child may be restricted from certain activities or intense competitive sports. Your child will also have to take antibiotics prior to and just after any dental procedures or other surgeries.
The average life expectancy at birth of individuals with Ebstein’s anomaly determined from 219 cases was 37 years 5). It was 33 years for males and nearly 39 for females. The differences in survival rates between male and female patients at ages 10 and 15 was significant and favored the male.
A severe leakage can lead to swelling of the heart and liver, and congestive heart failure.
Other complications may include:
- Abnormal heart rhythms (arrhythmias), including abnormally fast rhythms (tachyarrhythmias) and abnormally slow rhythms (bradyarrhythmias and heart block)
- Blood clots from the heart to other parts of the body
- Brain abscess
Ebstein’s anomaly complications
Many people with mild Ebstein’s anomaly have few complications. However, you may need to take some precautions in certain situations:
- Being active. If you have mild Ebstein’s anomaly with a nearly normal heart size and no heart rhythm disturbances, you can probably participate in most physical activities. Depending on your signs and symptoms, your doctor may recommend that you avoid certain competitive sports, such as football or basketball. Your doctor can help you decide which activities are right for you.
- During pregnancy. In many cases, women with mild Ebstein’s anomaly can safely have children. But pregnancy does have risks. If you plan on becoming pregnant, be sure to talk to your doctor ahead of time. He or she can tell you if it’s safe for you to become pregnant and help decide how much extra monitoring you may need throughout pregnancy and childbirth. He or she may also suggest other treatments for your condition or symptoms before you become pregnant. Being pregnant puts additional strain on your heart and circulatory system not only during pregnancy, but also during labor and delivery. However, vaginal delivery may be possible. Rarely, severe complications can develop that can cause death to the mother or baby.
Other complications that may result from Ebstein’s anomaly include heart failure, heart rhythm problems and, less commonly, sudden cardiac arrest or stroke.
Ebstein’s anomaly causes
Ebstein’s anomaly is a heart defect that you have at birth (congenital). Why it occurs is still unknown.
In Ebstein’s anomaly, the tricuspid valve sits lower than normal in the right ventricle. This makes it so that a portion of the right ventricle becomes part of the right atrium (becomes atrialized), causing the right atrium to be larger than usual. Because of this, the right ventricle can’t work properly.
Also, the tricuspid valve’s leaflets are abnormally formed. This can lead to blood leaking backward into the right atrium (tricuspid valve regurgitation).
The placement of the valve and how poorly it’s formed may vary among people. Some people may have a mildly abnormal valve. Others may have a valve that is extremely displaced, and it may leak severely.
The more the tricuspid valve leaks, the more the right atrium enlarges as it receives more blood. At the same time, the right ventricle enlarges (dilates) as it tries to cope with the leaky valve and still deliver blood to the lungs. Thus, the right-sided chambers of the heart enlarge, and as they do, they weaken, which may lead to heart failure.
Other heart conditions associated with Ebstein’s anomaly
Several other heart conditions may be associated with Ebstein’s anomaly. A few common conditions include:
- Holes in the heart. Many people with Ebstein’s anomaly have a hole between the two upper chambers of the heart called an atrial septal defect or a small flap-like opening called a patent foramen ovale. A patent foramen ovale is a hole between the upper heart chambers that is present in all babies before birth but usually closes after birth, although it may remain open in some people without causing issues.These holes may allow oxygen-poor blood in the right atrium to mix with oxygen-rich blood in the left atrium, decreasing the amount of oxygen available in your blood. This causes a bluish discoloration of the lips and skin (cyanosis).
- Abnormal heartbeats (arrhythmias). Some people with Ebstein’s anomaly have an abnormal heart rhythm (arrhythmia) characterized by rapid heartbeats (tachycardia). These types of arrhythmias can make your heart work less effectively, especially when the tricuspid valve is leaking severely. In some cases, a very fast heart rhythm may cause fainting spells (syncope).
- Wolff-Parkinson-White (WPW) syndrome. Some people with Ebstein’s anomaly may also have a condition known as Wolff-Parkinson-White syndrome — an abnormal electrical pathway in the heart. The presence of Wolff-Parkinson-White syndrome can lead to very fast heart rates and fainting spells.
Risk factors for Ebstein’s anomaly
Congenital heart defects, such as Ebstein’s anomaly, happen early in the development of a baby’s heart.
It’s uncertain what risk factors might cause the defect. Genetic and environmental factors are both thought to play a role. People with a family history of heart defects may be more likely to have Ebstein’s anomaly. A mother’s exposure to certain medications, such as lithium, may be associated with Ebstein’s anomaly in the child.
Ebstein’s anomaly prevention
There is no known prevention, other than talking with your provider before a pregnancy if you are taking medicines that are thought to be related to developing this disease. You may be able to prevent some of the complications of the disease. For example, taking antibiotics before dental surgery may help prevent endocarditis.
Ebstein’s anomaly symptoms
Symptoms range from mild to very severe. Symptoms develop soon after birth, and include bluish-colored lips and nails due to low blood oxygen levels (cyanosis). In severe cases, the baby appears very sick and has trouble breathing. In mild cases, the affected person may be asymptomatic for many years.
Symptoms in older children may include:
- Cough
- Failure to grow
- Fatigue
- Rapid breathing
- Shortness of breath
- Very fast heartbeat
Ebstein’s anomaly diagnosis
To diagnose Ebstein’s anomaly, your doctor may review your signs and symptoms and conduct a physical examination. If your doctor suspects an underlying problem, such as congenital heart disease, or if you have other signs and symptoms that may suggest Ebstein’s anomaly, your doctor may recommend several tests, including:
- Echocardiogram. This test is often used to diagnose Ebstein’s anomaly and other congenital heart defects. In this test, sound waves produce detailed images of your heart. This test assesses the structure of your heart, the tricuspid valve and the blood flow through your heart. Your doctor may also order a transesophageal echocardiogram. In this test, your doctor inserts a tube with a tiny sound device (transducer) into the part of your digestive tract that runs from your throat to your stomach (esophagus). Because the esophagus lies close to your heart, the transducer provides a detailed image of your heart.
- Electrocardiogram (ECG). An ECG uses sensors (electrodes) attached to your chest and limbs to measure the timing and duration of your heartbeat. An ECG can help your doctor detect irregularities in your heart’s rhythm and structure, and offer clues as to the presence of an extra pathway.
- Chest X-ray. A chest X-ray shows a picture of your heart, lungs and blood vessels. It can reveal if your heart is enlarged, which may be due to Ebstein’s anomaly.
- Cardiac MRI. A cardiac MRI uses magnetic fields and radio waves to create detailed images of your heart. This test may be used to determine the severity of your condition, get a detailed view of the tricuspid valve, and assess the size and function of your lower right heart chamber (right ventricle).
- Holter monitor. This is a portable version of an ECG. It’s especially useful in diagnosing rhythm disturbances that occur at unpredictable times. You wear the monitor under your clothing. It records information about the electrical activity of your heart as you go about your normal activities for a day or two.
- Pulse oximetry. In this test, a sensor attached to your finger or toe measures the amount of oxygen in your blood.
- Exercise stress test. During this test, you walk on a treadmill or ride a stationary bicycle while your blood pressure, heart rate, heart rhythm and breathing are monitored. A stress test may be used to get an idea of how your heart responds to exercise. It can help your doctor decide what level of physical activity is safe for you.
- Electrophysiology study. This test may be used to diagnose irregular heart rhythms (arrhythmias). In this test, doctors thread thin, flexible tubes (catheters) tipped with electrodes through your blood vessels to a variety of spots within your heart. Once in place, the electrodes can map the spread of electrical impulses through your heart. In addition, your doctor can use the electrodes to stimulate your heart to beat at rates that may trigger — or halt — an arrhythmia. This may help your doctor to determine if medications may help treat the arrhythmia.
- Cardiac catheterization. Doctors rarely use this test to diagnose Ebstein’s anomaly. However, in a few cases doctors may order it to obtain additional information, to confirm findings from other tests, or to check heart arteries. In this procedure, doctors insert a long, thin tube (catheter) into a blood vessel in your groin, arm or neck and guide it to your heart using X-ray imaging. A special dye injected through the catheter helps your doctor see the blood flow through your heart, blood vessels and valves; measure pressures and oxygen levels in your heart; and look for abnormalities inside the heart and lungs.
Ebstein’s anomaly treatment
Treatment depends on the severity of the defect and the specific symptoms. The goal of treatment is to reduce your symptoms and avoid future complications, such as heart failure and arrhythmias.
Medical care may include:
- Medications to help with heart failure, such as diuretics
- Oxygen and other breathing support
- Surgery to correct the valve
- Replacement of the tricuspid valve. This may be needed for children who continue to worsen or who have more serious complications.
Regular monitoring
If you have no signs or symptoms or abnormal heart rhythms, your doctor may recommend only careful monitoring of your heart condition with regular checkups.
Follow-up appointments generally include a physical examination and tests. Tests may include an electrocardiogram, echocardiogram, a Holter monitor test and an exercise stress test.
Medications
If you have heart rhythm disturbances, medications may help control your heart rate and maintain normal heart rhythm.
Your doctor may also prescribe medications for signs and symptoms of heart failure, if needed, such as drugs to prevent water retention (diuretics) and other medications. You also may be given medications to prevent blood clots if you have certain heart rhythm problems or a hole (atrial septal defect) between the upper heart chambers.
Some babies may be given a medication to keep a connection (ductus arteriosus) open between two major blood vessels leading from the heart — the aorta and pulmonary artery. This can help increase blood flow to the lungs. Some babies also may be given an inhaled substance called nitric oxide to help improve blood flow to the lungs.
Surgery
Your doctor may recommend surgery when your symptoms are affecting your quality of life. Surgery may also be recommended if you have mild symptoms but your heart is beginning to enlarge and your overall heart function is beginning to decrease. Because Ebstein’s anomaly is rare, choose a surgeon who’s familiar with the defect and who has training and experience performing procedures to correct it.
Several different types of procedures can be used to surgically treat Ebstein’s anomaly and associated defects, including:
- Tricuspid valve repair. In this procedure, surgeons reduce the size of the valve opening and allow the existing valve leaflets to come together to work properly. A band may be placed around the valve to stabilize the repair. This procedure is usually done when there’s enough valve tissue to allow for repair. Some surgeons perform a newer form of tricuspid valve repair called cone reconstruction. In cone reconstruction, surgeons separate the leaflets of the tricuspid valve from the heart muscle. The leaflets are then rotated and reattached, creating a “leaflet cone.” In some cases, your valve may need to be repaired again or your valve may need to be replaced in the future.
- Tricuspid valve replacement. If the existing valve can’t be repaired, your surgeon may replace the valve by removing the deformed valve and inserting either a biological tissue (bioprosthetic) or mechanical valve. Mechanical valves generally aren’t used often in tricuspid valve replacement. If a mechanical valve is used, you’ll need to take a blood-thinning medication for the rest of your life.
- Closure of the atrial septal defect. If a hole is present between the two upper chambers of the heart (atrial septal defect), your surgeon can close the hole during surgery to repair or replace the defective valve. Your surgeon can also repair other associated heart defects that may be present during surgery to repair or replace the tricuspid valve.
- Maze procedure. If you have fast heart rhythms, your surgeon may perform the maze procedure to correct the fast heart rhythms during surgery to repair or replace the tricuspid valve. In this procedure, your surgeon makes small incisions in the upper chambers of your heart to create a pattern or maze of scar tissue. Because scar tissue doesn’t conduct electricity, it interferes with stray electrical impulses that cause some types of fast heart rhythms. Extreme cold (cryotherapy) or radiofrequency energy may also be used to create the scars.
Radiofrequency catheter ablation
If you have fast or abnormal heart rhythms, your doctor may perform radiofrequency catheter ablation. In this procedure, your doctor threads one or more catheters through your blood vessels to your heart. Electrodes at the catheter tips can use radiofrequency energy to damage (ablate) a small spot of heart tissue and create an electrical block along the pathway that’s causing your arrhythmia. In some cases, repeat procedures may be necessary.
Heart transplantation
If you have severe Ebstein’s anomaly and poor heart function, a heart transplant may be necessary.
Coping and support
If you or your child has mild Ebstein’s anomaly, here are some steps that may help you cope:
- Follow up on medical care. Be sure to follow up with your cardiologist trained in congenital heart disease for regular evaluations. Be an active participant in monitoring the condition and report any new or worsening signs or symptoms to your doctor. Timely treatment can keep the condition from becoming worse.
- Take medications as prescribed. Taking medications at the right dose and the right time can help improve symptoms such as racing heartbeats, fatigue and shortness of breath.
- Stay active. Be as physically active as your or your child’s doctor allows. Exercise can help strengthen the heart and improve blood circulation. If you’re a parent of a child with Ebstein’s anomaly, it’s natural to want to protect your child from harm. But remember that your child needs to live life as normally as possible. Encourage playtime with breaks as needed. Ask your doctor for a note you can give to your child’s teachers or caregivers describing any restrictions on his or her physical activity.
- Develop a support network. Although many people with congenital heart defects lead normal, healthy lives, living with a heart defect isn’t always easy, particularly when you or your child needs continued specialized care. The physical, emotional and financial stress of coping with a serious health condition can be overwhelming. Having family and friends you can rely on is critical to successful coping. In addition, you may wish to ask your doctor about local support groups that may be helpful. Support groups can be a great source of practical information, comfort and friendship.
References [ + ]