Contents
What is a cleft palate
A cleft palate happens if the tissue that makes up the roof of the mouth does not join together completely during pregnancy (see Figures 1 and 2). For some babies, both the front and back parts of the palate are open. For other babies, only part of the palate is open. Cleft lip and cleft palate comprise the most common birth defect in the United States. One of every 600 newborns is affected by cleft lip and/or cleft palate. Centers for Disease Control and Prevention 1) recently estimated that, each year in the United States, about 2,650 babies are born with a cleft palate and 4,440 babies are born with a cleft lip with or without a cleft palate 2). Isolated orofacial clefts, or clefts that occur with no other major birth defects, are one of the most common types of birth defects in the United States 3). Depending on the cleft type, the rate of isolated orofacial clefts can vary from 50% to 80% of all clefts 4).
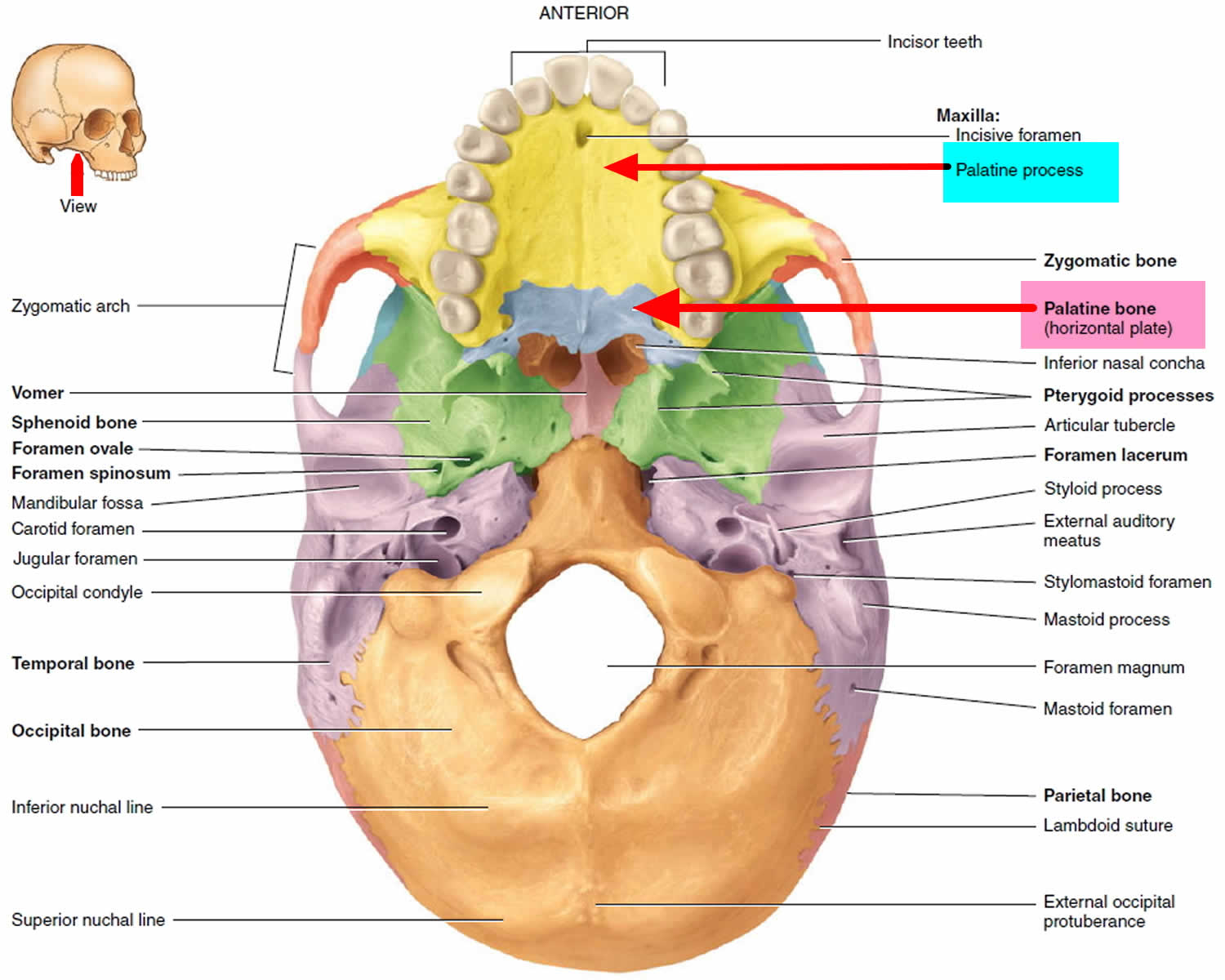
Usually the palatine processes of the maxillary bones unite during weeks 10 to 12 of embryonic development (see Figure 1). Failure to do so can result in one type of cleft palate. The condition may also involve incomplete fusion of the horizontal plates of the palatine bones (see Figure 1). Another form of this condition, called cleft lip, involves a split in the upper lip. Cleft lip and cleft palate often occur together.
Cleft lip and cleft palate are birth defects that occur when a baby’s lip or mouth do not form properly. They happen early during pregnancy. A baby can have a cleft lip, a cleft palate, or both.
- A cleft lip is a separation of the two sides of the lip. The separation often includes the bones of the upper jaw and/or upper gum.
- A cleft palate is an opening in the roof of the mouth in which the two sides of the palate did not fuse, or join together, as the unborn baby was developing. Cleft lip and cleft palate can occur on one side (unilateral cleft lip and/or palate), or on both sides (bilateral cleft lip and/or palate) or a cleft palate may go the full length of the palate. Because the lip and the palate develop separately, it is possible for the child to have a cleft lip, a cleft palate, or both cleft lip and cleft palate.
With cleft lip and palate, the majority of babies (91%) are diagnosed with a cleft lip before birth using a 20 week ultrasound scan, so most parents have a chance to learn more about cleft and prepare for the possibility that their child will have a cleft palate as well (see Cleft Lip Ultrasound Scan below). However for some parents, this isn’t the case, and the birth of their child may be the first time they’ve ever heard of the condition.
A cleft lip and palate can:
- Affect the appearance of the face
- Lead to problems with feeding and speech
- Lead to ear infections
Symptoms
- A child may have one or more birth defects.
- A cleft lip may be just a small notch in the lip. It may also be a complete split in the lip that goes all the way to the base of the nose.
- A cleft palate can be on one or both sides of the roof of the mouth. It may go the full length of the palate.
Other symptoms include:
- Change in nose shape (how much the shape changes varies)
- Poorly aligned teeth
Problems that may be present because of a cleft lip or palate are:
- Failure to gain weight
- Feeding problems
- Flow of milk through nasal passages during feeding
- Poor growth
- Repeated ear infections
- Speech difficulties
Depending on the extent and position of the cleft palate, speech and swallowing may be affected. In addition, children with cleft palate tend to have many ear infections, which can lead to hearing loss. Facial and oral surgeons recommend closure of cleft lip during the first few weeks following birth, and surgical results are excellent. Repair of cleft palate typically is completed between 12 and 18 months of age, ideally before the child begins to talk. Because the palate is important for pronouncing consonants, speech therapy may be required, and orthodontic therapy may be needed to align the teeth. Recent research strongly suggests that supplementation with folic acid (one of the B vitamins) during early pregnancy decreases the incidence of cleft palate and cleft lip. The mechanism behind this is not yet understood.
Babies are more likely to be born with a cleft lip and palate if they have a family history of these conditions or other birth defects.
With treatment, most children with orofacial clefts do well and lead a healthy life. Some children with orofacial clefts may have issues with self-esteem if they are concerned with visible differences between themselves and other children. Parent-to-parent support groups can prove to be useful for families of babies with birth defects of the head and face, such as orofacial clefts.
Many children with cleft palate need the help of a speech pathologist, and some many need an additional operation to improve speech. The most common problem these children experience is an overly nasal tone to their speech.
Figure 1. Inferior view of the skull
Figure 2. Cleft palate
Cleft lip and cleft palate
Cleft lip and cleft palate are birth defects that occur when a baby’s lip or mouth do not form properly during pregnancy. Together, these birth defects commonly are called “orofacial clefts”.
Figure 3. Cleft lip and cleft palate
Submucous cleft palate
In the submucous cleft palate, the separation of the palate is not complete. In submucous cleft palate there is a cleft in the muscles but it is covered by the lining at the top of the mouth, so it can’t usually been seen by the naked eye but can still have an impact on feeding, speech and hearing. The characteristic in the appearance of the submucous cleft palate is the bifid (double) uvula (see Figure 4 below). The cleft is referred mainly to the muscle layer of the palate, which is separated, and a notch at the back of the hard palate.
The functional problems in the submucous cleft are the same that are observed in the complete types of cleft palate.
- Nasal speech (rinolalia)
- Frequent episodes of otitis media (middle ear infection)
It should be noted that these problems are usually mild or may not exist at all, so it is possible not to be diagnosed.
The diagnosis is made solely with a clinical examination, in which the bifid uvula is observed. By gentle palpation of the palate it is detected a notch (deficit) at the back of in the hard palate.
The doctor starts to suspect the existence of submucous cleft palate when the child has unexplained rinolalia or frequent episodes of otitis media.
The surgical repair in submucous cleft should be performed only in the case that it is detected rinolalia (nasal speech) or frequent episodes of otitis.
Though, it should be noted that the results after the surgical repair for improving the speech or reducing the frequency of otitis media episodes are not always completely satisfactory. They may be less satisfactory than the cases of complete cleft palate.
Figure 4. Submucous cleft palate
What causes cleft palate
There are many causes of cleft lip and palate. Problems with genes passed down from 1 or both parents, drugs, viruses, or other toxins can all cause these birth defects. Cleft lip and palate may occur along with other syndromes or birth defects.
Research tells us it’s often caused by a combination of different genetic and environmental factors, but because of the huge number of factors involved it can be very difficult to narrow these down.
Genetics is all about things inherited from family members, like eye and hair color. Sometimes there is a clear family link, other times it just happens as a ‘one off’.
Environmental factors mean things that happen just before or during pregnancy, like taking a certain medicine or how the baby starts growing in the womb.
Most of the time, a cleft is caused by genetic and environmental factors coming together in a way which can’t be predicted or prevented.
Recently, the Centers for Disease Control and Prevention reported on important findings from research studies about some factors that increase the chance of having a baby with an orofacial cleft:
- Smoking―Women who smoke during pregnancy are more likely to have a baby with an orofacial cleft than women who do not smoke 5), 6).
- Diabetes―Women with diabetes diagnosed before pregnancy have an increased risk of having a child with a cleft lip with or without cleft palate, compared to women who did not have diabetes 7).
- Use of certain medicines―Women who used certain medicines to treat epilepsy, such as topiramate or valproic acid, during the first trimester (the first 3 months) of pregnancy have an increased risk of having a baby with cleft lip with or without cleft palate, compared to women who didn’t take these medicines 8), 9).
The Centers for Disease Control and Prevention continues to study birth defects, such as cleft lip and cleft palate, and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Cleft lip
The lip forms between the fourth and seventh weeks of pregnancy. As a baby develops during pregnancy, body tissue and special cells from each side of the head grow toward the center of the face and join together to make the face. This joining of tissue forms the facial features, like the lips and mouth. A cleft lip happens if the tissue that makes up the lip does not join completely before birth. This results in an opening in the upper lip. The opening in the lip can be a small slit or it can be a large opening that goes through the lip into the nose. A cleft lip can be on one or both sides of the lip or in the middle of the lip, which occurs very rarely. Children with a cleft lip also can have a cleft palate.
Bilateral and Unilateral Cleft Lip: Your baby’s cleft may have been described as ‘bilateral’ or ‘unilateral’. This is just whether or not the cleft affects one (unilateral) or two (bilateral) sides of the lip.
Complete and Incomplete: This describes whether or not the cleft goes all the way up into the nose or not.
Children with a cleft lip or a cleft palate often have problems with feeding and talking. They also might have ear infections, hearing loss, and problems with their teeth.
Often, surgery can close the lip and palate. Cleft lip surgery is usually done before age 12 months, and cleft palate surgery is done before 18 months. Many children have other complications. They may need additional surgeries, dental and orthodontic care, and speech therapy as they get older. With treatment, most children with clefts do well and lead a healthy life.
Figure 5. Cleft lip
Cleft lip causes
There are many causes of cleft lip and palate. Problems with genes passed down from 1 or both parents, drugs, viruses, or other toxins can all cause these birth defects. Cleft lip and palate may occur along with other syndromes or birth defects.
Research tells us it’s often caused by a combination of different genetic and environmental factors, but because of the huge number of factors involved it can be very difficult to narrow these down.
Genetics is all about things inherited from family members, like eye and hair color. Sometimes there is a clear family link, other times it just happens as a ‘one off’.
Environmental factors mean things that happen just before or during pregnancy, like taking a certain medicine or how the baby starts growing in the womb.
Most of the time, a cleft is caused by genetic and environmental factors coming together in a way which can’t be predicted or prevented.
Recently, the Centers for Disease Control and Prevention reported on important findings from research studies about some factors that increase the chance of having a baby with an orofacial cleft:
- Smoking―Women who smoke during pregnancy are more likely to have a baby with an orofacial cleft than women who do not smoke 10), 11).
- Diabetes―Women with diabetes diagnosed before pregnancy have an increased risk of having a child with a cleft lip with or without cleft palate, compared to women who did not have diabetes 12).
- Use of certain medicines―Women who used certain medicines to treat epilepsy, such as topiramate or valproic acid, during the first trimester (the first 3 months) of pregnancy have an increased risk of having a baby with cleft lip with or without cleft palate, compared to women who didn’t take these medicines 13), 14).
The Centers for Disease Control and Prevention continues to study birth defects, such as cleft lip and cleft palate, and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Cleft lip ultrasound
Orofacial clefts, especially cleft lip with or without cleft palate, can be diagnosed during pregnancy by a routine ultrasound. Around 81% of cleft lips are diagnosed before birth, usually at the 20-week anomaly scan where parents can find out their baby’s gender. They can also be diagnosed after the baby is born, especially cleft palate. However, sometimes certain types of cleft palate (for example, submucous cleft palate and bifid uvula) might not be diagnosed until later in life.
Most scans only ever pick up a cleft lip and sometimes a cleft gum (sometimes called a cleft alveolus, which is the bony bit of the gum). A regular ultrasound scan cannot reliably identify a cleft palate, either by itself or along with a cleft lip. If you have received a diagnosis of ‘cleft lip and palate’ from a regular ultrasound scan, it’s very likely that what was actually found was a cleft lip and gum. However, as around 60% of babies with a cleft lip will also have a cleft palate, expectant parents are often given a diagnosis of both. Only a very small number (1%) of cleft palates are actually diagnosed before birth.
If you’ve had an antenatal diagnosis of cleft lip you may be able to get a 3D/4D scan to see your baby in more detail.
What is a 3D/4D Scan?
3D/4D scans can provide more detail than a regular 2D ultrasound such as the one you would have had when the cleft was diagnosed. This can help expectant parents to get an idea of what their child may look like when he or she is born, and being able to see the ‘whole baby’ in this way can help with easing some of the distress that may be experienced after a diagnosis.
Which type should I get?
The only difference between these is that 3D scans take still images, and 4D scans show moving images which you may be able to take home as a DVD. These images will often be sepia-colored (yellowish) as this provides the sonographer with a better picture.
Diagnosis after Birth
Sometimes a cleft lip is not picked up at any scans before birth and can be a big surprise to parents. This is especially likely to happen (30% of cases) if the baby has a cleft lip without a cleft palate.
A cleft palate by itself (called an ‘isolated cleft palate’) is almost impossible to pick up before birth through regular scans, and can be easily missed when a baby is born if it is not looked for. Midwives and other health professionals should visually examine the baby’s mouth with a torch by pressing down on the baby’s tongue so the whole of the mouth can be seen.
Cleft lip repair
Surgery to close the cleft lip is often done when the child is between 6 weeks and 9 months old. However, most times, cleft lip repair is done when the child is 3 to 6 months old.
A cleft lip repair involves reconstructing the shape of the lip and the nose and joining the tissues that were not joined before birth. There are a number of different techniques which depend on the shape of your baby’s cleft and the surgeon’s preference. If the palate is involved, part of it may be repaired at the same time.
Dental impressions may be taken before or during the operation so the team has an accurate record of your baby’s cleft to compare with the future development of their mouth.
For cleft lip surgery, your child will have general anesthesia (asleep and not feeling pain). The surgeon will trim the tissues and sew the lip together. The stitches will be very small so that the scar is as small as possible. Most of the stitches will be absorbed into the tissue as the scar heals, so they will not have to be removed later. The surgery usually takes from 1-2 hours depending on the cleft, but your baby will likely be away from the ward for 2-4 hours.
Babies will usually stay in hospital for one or two nights after the operation, however if the cleft is quite small some babies may even be discharged on the same day.
Your baby will look quite different after the surgery, and this can be quite distressing to some parents. Many say that they miss their baby’s ‘old’ smile and that it takes a while to get used to how they look following the cleft repair. Prepare yourself for this as best as you can.
Surgery may be needed later in life if the problem has a major effect on the nose area.
Cleft palate repair
The palate (especially the soft palate) is very important for not just eating and swallowing, but also for speech, so a palate repair surgery aims to make sure the palate works as well as possible.
A cleft palate is most often closed within the first year of life so that the child’s speech develops normally. Most times, cleft palate repair is done when the child is older, between 9 months and 1 year old. This allows the palate to change as the baby grows. Doing the repair when the child is this age will help prevent further speech problems as the child develops.
A cleft palate is usually repaired in layers, with the focus on reconstructing the muscle of the soft palate.
Sometimes, a prosthetic device is temporarily used to close the palate so the baby can feed and grow until surgery can be done.
In cleft palate repair, your child will have general anesthesia (asleep and not feeling pain). Tissue from the roof of the mouth may be moved over to cover the soft palate. Sometimes a child will need more than one surgery to close the palate.
During these procedures, the surgeon may also need to repair the tip of your child’s nose. This surgery is called rhinoplasty.
Continued follow-up may be needed with speech therapists and orthodontists.
Alveolar Bone Graft (ABG) Surgery
If there is a gap in your baby’s gums, this will be repaired as his or her adult teeth are coming through with an Alveolar Bone Graft (ABG) operation at around 8-12 years old. The timing of treatment will be discussed with you by the cleft team. If your child’s cleft affects the alveolus (the bone in the gum where the teeth sit), they will probably need surgery to fill the gap in their gum so that their adult teeth can erupt (come through) properly. A ‘bone graft’ involves borrowing a bit of bone from one part of the body to help repair another.
Assessment for this surgery will begin between 7 and 9 years of age, and the surgery itself will usually be completed by age 12.
The orthodontist will often need to widen the area around the cleft to allow the surgeon to access it easier. This can involve a brace being fitted, most commonly a ‘quadhelix’. This takes place 6-9 months before the Alveolar Bone Graft (ABG) surgery. The orthodontist may also want to arrange to take out some of your child’s top baby teeth next to the cleft. This will give them more room to work with inside the mouth.
During the procedure, bone marrow will be taken (usually from the hip, sometimes from the tibia (shin) bone) and grafted into the gap left by the cleft. If the bone is taken from the hip, a small cut around 5 cm long is made low down on the tummy in an area that is usually covered by swimwear, a window is made in the outer surface of the bone and the inner marrow bone is scooped out. This is then closed and stitched up. The marrow will eventually grow back and the hip will be good as new.
The mucosa (red tissue covering the bone of the gum) is then opened up and peeled away from the gap in the bone. The mucosa from each side is then stitched together to make a ‘pocket’, and the bone marrow is packed into this pocket so the entire gap is filled. The gum is then closed over the bone. The ‘floor’ of the nose may also be repaired at this time. This can help the bottom of the nose look straighter, but won’t change the shape of the face.
Most children are admitted onto the ward the day before surgery and are able to go home the day after. Complications are rare and minor, and the scar on the donor site (hip or shin) will fade considerably with time.
After Alveolar Bone Graft (ABG) Surgery
Afterwards, the ‘donor’ site where the bone was taken is often sore, and your child’s mouth will feel quite strange. They will have a ‘drip’ with painkillers to help ease the discomfort.
Your surgeon will be able to advise on when your child will be able to eat and drink again. They’ll have to stick to ‘soft’ foods for a while after they go home until they’re healed.
It’s vital that the mouth is kept very clean for the first 10-14 days after surgery. This is because the bone placed in the gap will have ‘new’ bone growing around it, and at this time it’s very vulnerable to infection. Good, careful brushing and using a mouthwash recommended by your surgeon will help your child recover.
Usually your child will need at least a week of school to make sure they don’t get an infection from anyone and can rest and recover. Any sporting activities should be avoided for at least two weeks, but check with your surgeon about this. It may take several weeks before the swelling of the face goes down and the inside of your child’s mouth starts to feel normal again.
Your child will need to come back a few weeks after the operation so the consultant can make sure everything is healing properly. After 6 months, your child will have an x-ray to see how successful the treatment has been. It may take several months or even a year before the adult canine tooth erupts through the new bone graft. If teeth are crooked once they’ve come through, these can be straightened 3-6 months after the bone graft. Braces are usually not used until all a child’s permanent teeth have erupted into the mouth.
Cleft palate surgery risks
Risks from any anesthesia and any surgery include:
- Breathing problems
- Reactions to the medicines
- Bleeding
- Infection
- Need for further surgery
Problems these surgeries may cause are:
- The bones in the middle of the face may not grow correctly.
- The connection between the mouth and nose may not be normal.
Before the Procedure
You will meet with a speech therapist or feeding therapist soon after your child is born. The therapist will help you find the best way to feed your child before the surgery. Your child must gain weight and be healthy before surgery.
Your child’s health care provider may:
- Test your child’s blood (do a complete blood count and “type and cross” to check your child’s blood type)
- Take a complete medical history of your child
- Do a complete physical exam of your child
Always tell your child’s provider:
What medicines you are giving your child. Include drugs, herbs, and vitamins you bought without a prescription.
During the days before the surgery:
- About 10 days before the surgery, you will be asked to stop giving your child aspirin, ibuprofen (Advil, Motrin), warfarin (Coumadin), and any other drugs that make it hard for your child’s blood to clot.
- Ask which drugs the child should still take on the day of the surgery.
On the day of the surgery:
Most times, your child will not be able to drink or eat anything for several hours before the surgery.
- Give your child a small sip of water with any drugs your doctor told you to give your child.
- You will be told when to arrive for the surgery.
- The provider will make sure your child is healthy before the surgery. If your child is ill, surgery may be delayed.
Dental impressions may be taken before or during the operation so the team has an accurate record of your baby’s cleft to compare with the future development of their mouth.
Sometimes, small incisions are made to the side of the cleft to ‘loosen’ the tissue and give the surgeon more to work with, but these will heal very quickly.
After the Procedure
Your child will probably be in the hospital for 5 to 7 days right after surgery. Complete recovery can take up to 4 weeks.
The surgery wound must be kept very clean as it heals. It must not be stretched or have any pressure put on it for 3 to 4 weeks. Your child’s nurse should show you how to take care of the wound. You will need to clean it with soap and water or a special cleaning liquid, and keep it moist with ointment.
Until the wound heals, your child will be on a liquid diet. Your child will probably have to wear arm cuffs or splints to prevent picking at the wound. It is important for your child not to put hands or toys in their mouth.
Cleft palate surgery outlook (prognosis)
Most babies heal without problems. How your child will look after healing often depends on how serious the defect was. Your child might need another surgery to fix the scar from the surgery wound.
A child who had a cleft palate repair may need to see a dentist or orthodontist. The teeth may need correcting as they come in.
Hearing problems are common in children with cleft lip or cleft palate. Your child should have a hearing test early on, and it should be repeated over time.
Your child may still have problems with speech after the surgery. This is caused by muscle problems in the palate. Speech therapy will help your child.
Many children with cleft palate need the help of a speech pathologist, and some many need an additional operation to improve speech. The most common problem these children experience is an overly nasal tone to their speech.
References [ + ]