Contents
What is mastitis
Mastitis is a condition which causes a woman’s breast tissue to become painful and inflamed (swelling, warmth and redness) that can be caused by an infection, some type of obstruction, or an allergy. You also might have fever and chills. It’s most common in breastfeeding women, usually within the first three months after giving birth, although sometimes mastitis can occur in women who aren’t breast-feeding.
If mastitis is caused by breastfeeding, doctors may refer to it as lactation mastitis or puerperal mastitis. Non-breastfeeding women often have a type called periductal mastitis.
Mastitis can cause you to feel run down, making it difficult to care for your baby.
Sometimes mastitis leads a mother to wean her baby before she intends to, but continuing to breast-feed, even while taking an antibiotic for the mastitis, is better for you and your baby.
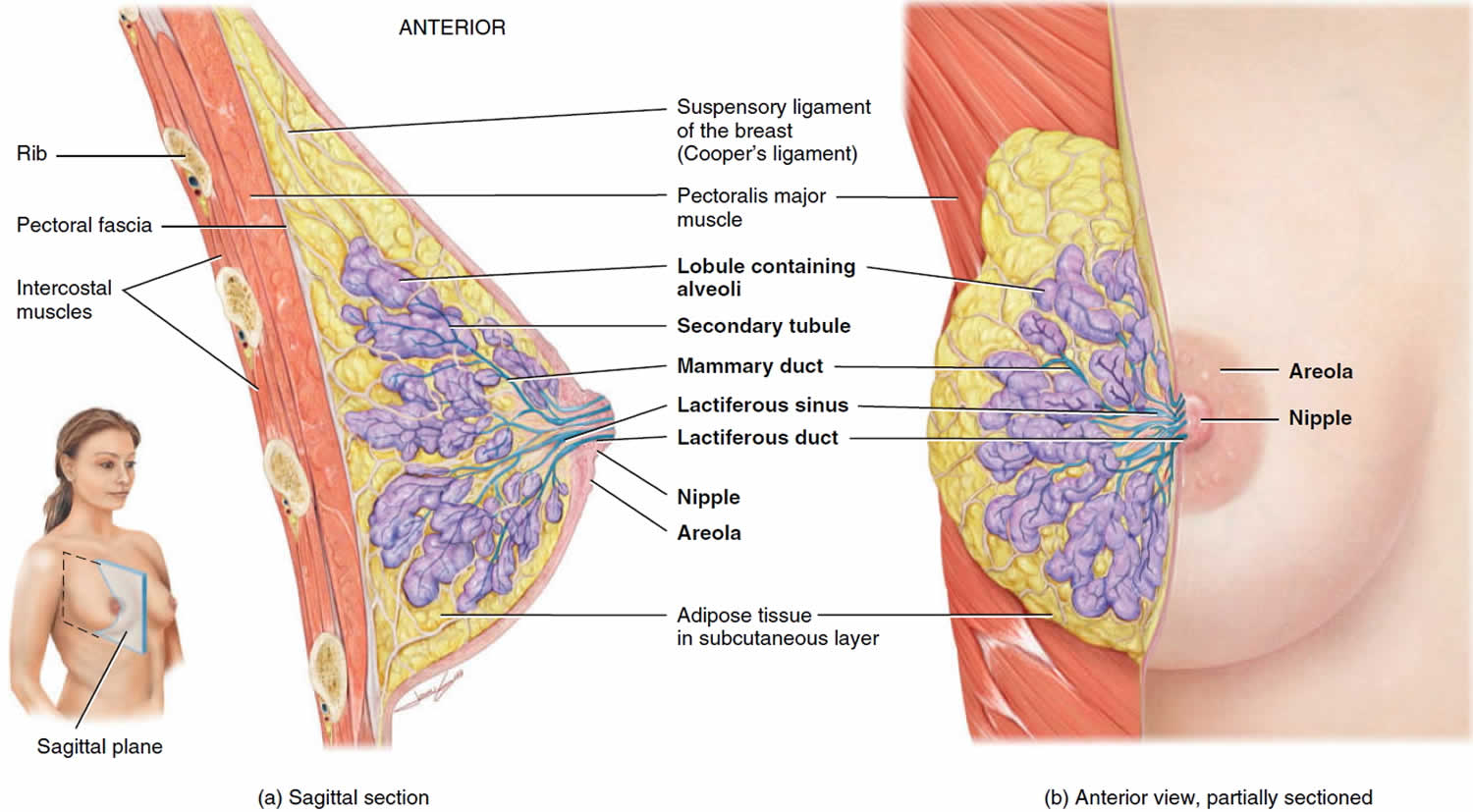
Figure 1. Normal breast (female)
Figure 2. Breast mastitis
Mastitis usually only affects one breast, and symptoms often develop quickly. Symptoms of mastitis can include:
- a red, swollen area on your breast that may feel hot and painful to touch
- a breast lump or area of hardness on your breast
- a burning pain in your breast that may be continuous or may only occur when you are breastfeeding
- nipple discharge, which may be white or contain streaks of blood
You may also experience flu-like symptoms, such as aches, a high temperature (fever), chills and tiredness.
See your doctor as soon as possible if you think you might have mastitis. It may help to try some self-help measures before your appointment.
It’s important to see your doctor promptly as mastitis could lead to a painful collection of pus (breast abscess), which may need to be drained surgically.
Mastitis causes
Breast-feeding is a learned skill, and poor technique can lead to milk being trapped in the breast, a main cause of mastitis.
Mastitis can be caused by a build-up of milk within the breast (milk stasis) or damage to the nipple, which may lead to a bacterial infection.
What causes mastitis
In breastfeeding women, mastitis is often caused by a build-up of milk within the breast. This is known as milk stasis.
Milk stasis can occur for a number of reasons, including:
- a baby not properly attaching to the breast during feeding
- a baby having problems sucking
- infrequent feeds or missing feeds
In some cases, this build-up of milk can also become infected with bacteria. This is known as infective mastitis.
In non-breastfeeding women, mastitis most often occurs when the breast becomes infected as a result of damage to the nipple, such as a cracked or sore nipple, or a nipple piercing.
Mastitis in breastfeeding
Milk stasis
Many cases of mastitis in breastfeeding women are thought to be caused by milk stasis. This occurs when the milk isn’t properly removed from your breast during breastfeeding.
It can be caused by:
- a baby not properly attaching to the breast during feeding – this may mean that not enough milk is removed; see breastfeeding position and attachment for advice on helping your child feed correctly
- a baby having problems sucking – for example, because they have a tongue-tie, a piece of skin between the underside of their tongue and the floor of their mouth
- infrequent or missed feeds – for example, when they start to sleep through the night
- favoring one breast for breastfeeding – for example, because one of your nipples is sore; this can lead to milk stasis developing in the other breast
- a knock or blow to the breast that damages the milk duct or the glands in your breast
- pressure on your breast – for example, from tight-fitting clothing (including bras), seat belts or sleeping on your front
Milk stasis can cause the milk ducts in your breasts to become blocked, and can cause milk to build up within the affected breast.
Experts aren’t sure exactly why breast milk can cause the breast tissue to become inflamed. One theory is that the pressure building up inside the breast forces some milk into the surrounding tissue.
Your immune system may then mistake proteins in the milk for a bacterial or viral infection and responds by inflaming the breast tissue in an effort to stop the spread of infection.
Infection
Fresh human milk doesn’t usually provide a good environment in which bacteria can breed. However, milk stasis can cause milk to stagnate and become infected. This is known as infective mastitis.
Exactly how bacteria enter the breast tissue hasn’t been conclusively proven.
The bacteria that usually live harmlessly on the skin of your breast may enter through a small crack or break in your skin, or bacteria present in the baby’s mouth and throat may be transferred during breastfeeding.
You may be at greater risk of developing infective mastitis if your nipple is damaged – for example, as a result of using a manual breast pump incorrectly or because your baby has a cleft lip or palate, an opening or split in their lip or roof of their mouth.
Mastitis in breastfeeding women is more likely to be caused by an infection if self-help measures to express milk from the affected breast haven’t improved symptoms within 12 to 24 hours.
Mastitis non-breastfeeding
In women who don’t breastfeed, mastitis is often caused by a bacterial infection. This can occur as a result of bacteria getting into the milk ducts through a cracked or sore nipple, or a nipple piercing.
This type of mastitis is known as periductal mastitis. It usually affects women in their late 20s and early 30s, and is more common among women who smoke.
Occasionally, mastitis can occur in non-breastfeeding women as a result of duct ectasia. This is when the milk ducts behind the nipple get shorter and wider as the breasts age. It typically occurs in women approaching the menopause.
Duct ectasia is usually nothing to be concerned about, but in some cases a thick, sticky secretion can collect in the widened ducts, and this can irritate and inflame the duct lining.
Risk factors for mastitis
Risk factors for mastitis include:
- Breast-feeding during the first few weeks after childbirth
- Sore or cracked nipples, although mastitis can develop without broken skin
- Using only one position to breast-feed, which may not fully drain your breast
- Wearing a tightfitting bra or putting pressure on your breast from using a seatbelt or carrying a heavy bag, which may restrict milk flow
- Becoming overly tired or stressed
- Previous bout of mastitis while breast-feeding
- Poor nutrition
Mastitis complications
If mastitis isn’t adequately treated, or it’s related to a blocked duct, a collection of pus (abscess) can develop in your breast and form a breast mass or area of firmness with thickening. An abscess usually requires surgical drainage. To avoid this complication, talk to your doctor as soon as you develop signs or symptoms of mastitis.
How to prevent mastitis
Although mastitis can usually be treated easily, the condition can recur if the underlying cause isn’t addressed.
If you’re breastfeeding, you can help reduce your risk of developing mastitis by taking steps to stop milk building up in your breasts, such as:
- breastfeed exclusively for around six months, if possible
- encourage your baby to feed frequently, particularly when your breasts feel overfull
- ensure your baby is well attached to your breast during feeds – ask for advice if you’re unsure
- let your baby finish their feeds – most babies release the breast when they’ve finished feeding; try not to take your baby off the breast unless they’re finished
- avoid suddenly going longer between feeds – if possible, cut down gradually
- avoid pressure on your breasts from tight clothing, including bras
Your doctor, midwife or health visitor can advise about how to improve your breastfeeding technique.
How to breastfeed
If breastfeeding feels a bit awkward at first, don’t worry. Breastfeeding is a skill that you and your baby learn together, and it can take time to get used to.
In the first few days, you and your baby will be getting to know each other. It may take time for both of you to get the hang of breastfeeding.
This happens more quickly for some women than others. But nearly all women produce enough milk for their baby.
Having skin-to-skin contact with your baby straight after the birth will help to keep them warm and calm, and steady their breathing.
Skin to skin means holding your baby naked or dressed only in a nappy against your skin, usually under your top or under a blanket.
Skin-to-skin time can be a bonding experience for you and your baby. It’s also a great time to have your first breastfeed. If you need any help, your midwife will support you with positioning and attachment.
Skin-to-skin contact is good at any time. It will help to comfort you and your baby over the first few days and weeks as you get to know each other. It also helps your baby attach to your breast using their natural crawling and latching on reflexes.
If skin-to-skin contact is delayed for some reason – for example, if your baby needs to spend some time in special care – it doesn’t mean you won’t be able to bond with or breastfeed your baby.
If necessary, your midwife will show you how to express your breast milk until your baby is ready to breastfeed. They will also help you have skin-to-skin contact with your baby as soon as it’s possible.
There are lots of different positions you can use to breastfeed. You just need to check the following points:
- Are you comfortable? It’s worth getting comfortable before a feed. Use pillows or cushions if necessary. Your shoulders and arms should be relaxed.
- Are your baby’s head and body in a straight line? (It’s hard for your baby to swallow if their head and neck are twisted.)
- Are you holding your baby close to you, facing your breast? Supporting their neck, shoulders and back should allow them to tilt their head back and swallow easily.
- Always bring your baby to the breast rather than leaning forward to ‘post’ your breast into your baby’s mouth, as this can lead to poor attachment.
- Your baby needs to get a big mouthful of breast. Placing your baby with their nose level with your nipple will encourage them to open their mouth wide and attach to the breast well.
- Avoid holding the back of your baby’s head, so that they can tip their head back. This way your nipple goes past the hard roof of their mouth and ends up at the back of their mouth against the soft palate.
Colostrum: your first milk
The fluid your breasts produce in the first few days after birth is called colostrum. It’s usually a golden yellow color. It’s a very concentrated food, so your baby will only need about a teaspoonful at each feed.
Your baby may want to feed quite often, perhaps every hour to begin with. They’ll begin to have fewer, longer feeds once your breasts start to produce more “mature” milk after a few days.
The more you breastfeed, the more your baby’s sucking will stimulate your supply and the more milk you’ll make.
Your let-down reflex
Your baby’s sucking causes milk stored in your breasts to be squeezed down ducts towards your nipples. This is called the let-down reflex.
Some women get a tingling feeling, which can be quite strong. Others feel nothing at all.
You’ll see your baby respond when your milk lets down. Their quick sucks will change to deep rhythmic swallows as the milk begins to flow. Babies often pause after the initial quick sucks while they wait for more milk to be delivered.
Occasionally this let-down reflex can be so strong that your baby coughs and splutters. Your midwife, health visitor or breastfeeding supporter can help with this, or see some tips for when you have too much breast milk.
If your baby seems to be falling asleep before the deep swallowing stage of feeds, they may not be properly attached to the breast. Ask your midwife, health visitor or breastfeeding supporter to check your baby’s positioning and attachment.
Sometimes you’ll notice your milk letting down in response to your baby crying or when you have a warm bath or shower. This is normal.
Building up your milk supply
Around two to four days after birth you may notice that your breasts become fuller and warmer. This is often referred to as your milk “coming in”.
Your milk will vary according to your baby’s needs. Each time your baby feeds, your body knows to make more milk for the next feed. The amount of milk you make will increase or decrease depending on how often your baby feeds.
In the early weeks, “topping up” with formula milk or giving your baby a dummy can lower your milk supply.
Feed your baby as often as they want and for as long as they want. This is called responsive feeding. In other words, responding to your baby’s needs. It’s also known as on-demand or baby-led feeding.
In the beginning, it can feel like you’re doing nothing but feeding. But gradually you and your baby will get into a pattern, and the amount of milk you produce will settle down.
It’s important to breastfeed at night because this is when you produce more hormones (prolactin) to build up your milk supply.
Ways to boost your breast milk supply
- Ask your midwife, health visitor or breastfeeding specialist to watch your baby feeding. They can offer guidance and support to help you properly position and attach your baby to the breast.
- Avoid giving your baby bottles of formula or a dummy until breastfeeding is well established. This usually takes a few weeks.
- Feed your baby as often as you and they want to.
- Expressing some breast milk after feeds once breastfeeding is established will help build up your supply.
- Offer both breasts at each feed and alternate which breast you start with.
- Keep your baby close to you and hold them skin to skin. This will help you spot signs your baby is ready to feed early on, before they start crying.
In rare cases, women may need to take a drug to help them produce more milk, but this isn’t usually necessary.
How to latch your baby on to your breast
- Hold your baby close to you with their nose level with the nipple.
- Wait until your baby opens their mouth really wide with their tongue down. You can encourage them to do this by gently stroking their top lip.
- Bring your baby on to your breast.
- Your baby will tilt their head back and come to your breast chin first. Remember to support your baby’s neck but not hold the back of their head. They should then be able to take a large mouthful of breast. Your nipple should go towards the roof of their mouth.
Step by Step Guide in Getting your baby into position
Breastfeeding – Step 1. Hold your baby’s whole body close with their nose level with your nipple.
Breastfeeding – Step 2. Let your baby’s head tip back a little so that their top lip can brush against your nipple. This should help your baby to make a wide open mouth.
Breastfeeding – Step 3. When your baby’s mouth opens wide, their chin should be able to touch your breast first, with their head tipped back so that their tongue can reach as much breast as possible.
Breastfeeding – Step 4. With your baby’s chin firmly touching your breast and their nose clear, their mouth should be wide open. You should see much more of the darker nipple skin above your baby’s top lip than below their bottom lip. Your baby’s cheeks will look full and rounded as they feed.
Signs your baby is well attached to your breast
- Your baby has a wide mouth and a large mouthful of breast.
- Your baby’s chin is touching your breast, their lower lip is rolled down (you can’t always see this) and their nose isn’t squashed against your breast.
- You don’t feel any pain in your breasts or nipples when your baby is feeding, although the first few sucks may feel strong.
- You can see more of the dark skin around your nipple (areola) above your baby’s top lip than below their bottom lip.
How to tell if your baby is getting enough milk
- Your baby will appear content and satisfied after most feeds.
- They should be healthy and gaining weight (although it’s normal for babies to lose a little weight in the first days after birth). Talk to your midwife or health visitor if you are concerned your baby is not gaining weight and is unsettled during or after breast feeds.
- After the first few days, your baby should have at least six wet nappies a day.
- After the first few days, they should also pass at least two soft yellow poos (stools) every day.
How often you should feed your baby
How often babies feed varies. As a very rough guide, your baby should feed at least eight times or more every 24 hours during the first few weeks.
It’s fine to feed your baby whenever they are hungry, when your breasts feel full or if you just want to have a cuddle.
It’s not possible to overfeed a breastfed baby.
When your baby is hungry they may:
- get restless
- suck their fist or fingers
- make murmuring sounds
- turn their head and open their mouth (rooting)
It’s best to try and feed your baby during these early feeding cues as a crying baby is difficult to feed.
How to tell if your baby is getting enough milk
When you first start breastfeeding, you may be concerned your baby is not getting enough milk. You can’t always tell how much a breastfed baby is drinking.
It’s very rare that women don’t make enough breast milk for their babies, but it may take a little while before you feel confident your baby is getting what they need.
Your baby will generally let you know, but wet and dirty nappies are a good indication, as well as hearing your baby swallow.
If you need some reassurance your baby is getting enough milk, it’s a good idea to get a midwife, health visitor or breastfeeding specialist to watch your baby feed.
Try to carry on breastfeeding if you can. Introducing bottles of formula milk can fill up your baby’s stomach so they no longer want to breastfeed as frequently. This then reduces the stimulation for you to make more milk.
Signs your baby is getting enough milk
- Your baby starts feeds with a few rapid sucks followed by long, rhythmic sucks and swallows with occasional pauses.
- You can hear and see your baby swallowing.
- Your baby’s cheeks stay rounded, not hollow, during sucking.
- They seem calm and relaxed during feeds.
- Your baby comes off the breast on their own at the end of feeds.
- Their mouth looks moist after feeds.
- Your baby appears content and satisfied after most feeds.
- Your breasts feel softer after feeds.
- Your nipple looks more or less the same after feeds – not flattened, pinched or white.
- You may feel sleepy and relaxed after feeds.
Other signs your baby is feeding well
- Your baby gains weight steadily after the first two weeks – it’s normal for babies to lose some of their birth weight in the first two weeks.
- They appear healthy and alert when they’re awake.
- From the fourth day, they should do at least two soft, yellow poos (stools) every day for the first few weeks.
- From day five onwards, wet nappies should start to become more frequent, with at least six heavy, wet nappies every 24 hours. In the first 48 hours, your baby is likely to have only two or three wet nappies.
It can be hard to tell if disposable nappies are wet. To get an idea, take a nappy and add two to four tablespoons of water. This will give you an idea of what to look and feel for.
Things that can affect your milk supply
- Poor attachment and positioning.
- Not feeding your baby often enough.
- Drinking alcohol and smoking while breastfeeding – these can both interfere with your milk production.
- Previous breast surgery, particularly if your nipples have been moved.
- Having to spend time away from your baby after the birth – for example, because they were premature: Frequent gentle hand expression will help.
- Illness in you or your baby.
- Giving your baby bottles of formula or a dummy before breastfeeding is well established.
- Using nipple shields – although this may be the only way to feed your baby with damaged nipples and is preferable to stopping feeding.
- Some medications, including dopamine, ergotamine and pyridoxine.
- Anxiety, stress or depression.
- Your baby having a tongue tie that restricts the movement of their tongue.
With skilled help, lots of these problems can be sorted out. If you have concerns about how much milk your baby is getting, it’s important to ask for help early. Speak to your midwife, health visitor or a breastfeeding specialist. They can also tell you where you can get further support.
What medicines can I take while I’m breastfeeding?
Medicines that can be taken while breastfeeding include:
- most antibiotics
- common painkillers, such as paracetamol and ibuprofen – but not aspirin
- asthma inhalers
- vitamins – but only at the recommended dose
You can use some methods of contraception and some cold remedies, but not all.
Always check with your doctor, midwife, health visitor or pharmacist, who can advise you.
It’s fine to have dental treatments, local anesthetics, vaccinations – including MMR, tetanus and flu injections – and most operations.
Common drugs that are NOT recommended when you’re breastfeeding include:
- codeine phosphate – used to control diarrhea
- nasal decongestants – but simple salt water drops are fine
- aspirin for pain relief – although you can take it if your doctor prescribes it for you as an anti-platelet drug
Talk to you doctor or pharmacist before taking antihistamines for allergies or allergy-related conditions, such as hay fever.
The most comprehensive, up-to-date source of information regarding the safety of maternal medications when the mother is breastfeeding is LactMed (https://toxnet.nlm.nih.gov/newtoxnet/lactmed.htm), an Internet-accessed source published by the National Library of Medicine/National Institutes of Health. In general, breastfeeding is not recommended when mothers are receiving medication from the following classes of drugs: amphetamines, chemotherapy agents, ergotamines, and statins.
It’s dangerous to take illegal drugs while you’re breastfeeding. They can affect your ability to look after your baby safely, and reach your baby via your breast milk.
The long-term effects on babies if you use illegal drugs while breastfeeding aren’t known. Talk to your midwife, health visitor or doctor if you’re using them.
Breastfeeding your premature baby
Your breast milk is important to your baby at any age. Research shows that giving your premature baby your breast milk benefits their health as well as yours.
Among other things, your breast milk:
- helps protect your baby from infections, particularly of their gut (premature babies are more prone to these)
- contains hormones, nutrients and growth factors that help your baby to grow and develop
- is easier for your baby to digest than formula milk, because it’s human milk specially designed by your body for your baby
If your baby is too small or sick to breastfeed, you’ll need to start regularly expressing your breast milk soon after they’re born to get your milk supply going. Then you can start breastfeeding once you and your baby are ready.
Even if you weren’t planning to breastfeed, you could express your breast milk for a while and see how it goes.
Spending lots of time close together can help boost your breast milk supply and establish breastfeeding.
As soon as possible, you’ll be encouraged to spend time holding your baby against your skin. This is sometimes called kangaroo care.
Your baby will be dressed just in a nappy and then placed inside your top or under a blanket so they can be held securely against your skin.
This skin-to-skin contact helps you feel close to your baby. Your partner can enjoy this kind of contact as well.
For your premature baby, skin-to-skin contact:
- reduces stress and/or pain
- promotes healthy weight gain
- helps to establish breastfeeding
- helps them adapt to their environment
- helps to regulate and support their heart rate and breathing
For mums, skin-to-skin contact:
- helps prevent postnatal depression
- increases your confidence as a new parent
- supports the hormones that help with breast milk production and supply
For dads, holding your baby skin to skin:
- helps you bond with your baby – babies can hear both parents’ voices in the womb and will be calmed by the sound of your voice as well as their mum’s
- helps you feel more confident as a parent
Expressing milk if your baby is premature
Always ask for help early if you have any worries or questions.
It’s recommended you express eight to 10 times a day to begin with, including at least once at night, to keep your milk supply up.
In the early days, it’s often easier to express your milk by hand. Your midwife or a breastfeeding supporter can show you how.
You’ll probably only express a few drops to begin with but, if you hand express often, this will increase.
In the early days you can collect your breast milk in a small, sterile cup and store it in a syringe. Every drop is beneficial for your baby.
Once you are producing more milk, you could try using a breast pump. If your baby is in a neonatal unit, the hospital will usually be able to lend you an electric breast pump for expressing your milk. If they can’t lend you one, you can hire one.
Dealing with leaking breasts
Sometimes, breast milk may leak unexpectedly from your nipples. Press the heel of your hand gently but firmly on your breast when this happens.
Wearing breast pads will stop your clothes becoming wet with breast milk. Remember to change them frequently to prevent any infection.
Expressing some milk may also help. Only express enough to feel comfortable as you don’t want to overstimulate your supply.
If your baby hasn’t fed recently you could offer them a feed as breastfeeding is also about you being comfortable.
Mastitis signs and symptoms
With mastitis, signs and symptoms can appear suddenly and may include:
- Breast tenderness or warmth to the touch
- Generally feeling ill (malaise)
- Breast swelling
- Pain or a burning sensation continuously or while breast-feeding
- Skin redness, often in a wedge-shaped pattern
- Fever of 101 °F (38.3 °C) or greater
Although mastitis usually occurs in the first several weeks of breast-feeding, it can happen anytime during breast-feeding. Lactation mastitis tends to affect only one breast.
In most cases, you’ll feel ill with flu-like symptoms for several hours before you recognize that your breast has an area of tenderness and redness. As soon as you recognize this combination of signs and symptoms, it’s time to contact your doctor.
Breast mastitis diagnosis
Your doctor can often diagnose mastitis based on your symptoms and an examination of your breasts.
If you’re breastfeeding, they may ask you to show them how you breastfeed. Try not to feel as if you’re being tested or blamed – it can take time and practice to breastfeed correctly.
Your doctor may request a small sample of your breast milk for testing if:
- your symptoms are particularly severe
- you’ve had recurrent episodes of mastitis
- you’ve been given antibiotics and your condition hasn’t improved
This will help determine whether you have a bacterial infection and allow your doctor to prescribe an effective antibiotic.
If you have mastitis and aren’t breastfeeding, your doctor should refer you to hospital for a specialist examination and a breast scan to rule out other conditions, particularly if your symptoms haven’t improved after a few days of treatment.
A rare form of breast cancer — inflammatory breast cancer — also can cause redness and swelling that could initially be confused with mastitis. Your doctor may recommend a diagnostic ultrasound scan and a mammogram (X-ray of the breast). If your signs and symptoms persist even after you complete a course of antibiotics, you may need a biopsy to make sure you don’t have breast cancer.
Mastitis treatment
Mastitis can usually be easily treated and most women make a full recovery very quickly.
Home remedies for mastitis
Many cases of mastitis that aren’t caused by an infection often improve through using self-care techniques, such as:
- Continue to breast-feed as often and as long as your baby is hungry
- Making sure you get plenty of rest, preferably in bed with your baby, which will encourage frequent feedings
- Drinking plenty of fluids
- Avoid prolonged overfilling of your breast with milk (engorgement) before breast-feeding
- Using over-the-counter painkillers such as paracetamol (acetaminophen) or ibuprofen to reduce any pain or fever – a small amount of paracetamol can enter the breast milk, but it’s not enough to harm your baby (it’s not safe to take aspirin while breastfeeding)
- Avoiding tight-fitting clothing, including bras, until your symptoms improve
- Wear a supportive bra
- If you’re breastfeeding, regularly expressing milk from your breasts
- Placing a warm cloth soaked with warm water (a compress) over your breast to help relieve the pain – a warm shower or bath may also help
- Vary your breast-feeding positions
- If breast-feeding on the infected breast is too painful or your infant refuses to nurse on that breast, try pumping or hand-expressing milk.
Breastfeeding your baby when you have mastitis, even if you have an infection, won’t harm your baby and can help improve your symptoms.
It may also help to feed more frequently than usual, express any remaining milk after a feed, and express milk between feeds.
For non-breastfeeding women with mastitis and breastfeeding women with a suspected infection, a course of antibiotic tablets will usually be prescribed to bring the infection under control.
Expressing breast milk
If you’re breastfeeding and you have mastitis, it’s likely to be caused by a build-up of milk within the affected breast. Regularly expressing milk from your breast can often help improve the condition quickly.
One of the best ways to express milk from your breast is to continue breastfeeding your baby, or expressing milk by hand or using a pump. Continuing to breastfeed your baby won’t harm them, even if your breast is also infected.
The milk from the affected breast may be a little saltier than normal, but it’s safe for your baby to drink. Any bacteria present in the milk will be harmlessly absorbed by the baby’s digestive system and won’t cause any problems.
You may find that expressing breast milk becomes easier by:
- breastfeeding your baby as often and as long as they’re willing to feed, starting feeds with the sore breast first
- making sure your baby is properly positioned and attached to your breasts – your midwife or health visitor will advise you about how to do this
- experimenting by feeding your baby in different positions
- massaging your breast to clear any blockages – stroke from the lumpy or tender area towards your nipple to help the milk flow
- warming your breast with warm water – this can soften it and help your breast milk flow better, making it easier for your baby to feed
- making sure your breast is empty after feeds by expressing any remaining milk
- if necessary, expressing milk between feeds – see expressing breast milk for more information
Contact your doctor if your symptoms worsen or don’t improve within 12 to 24 hours of trying these techniques. If this happens, it’s likely that you have an infection and will need antibiotics.
Antibiotics
If you’re breastfeeding and the above measures haven’t helped improve your symptoms, or your doctor can see your nipple is clearly infected, you’ll be prescribed a course of antibiotics to kill the bacteria responsible. These should be taken in addition to continuing the self-help measures above.
Your doctor will also usually prescribe a course of antibiotics if you develop mastitis and aren’t breastfeeding.
If you’re breastfeeding, your doctor will prescribe a safe antibiotic. This will usually be a tablet or capsule that you take by mouth (orally) four times a day for up to 14 days.
A very small amount of the antibiotic may enter your breast milk, which may make your baby irritable and restless. Their stools may become looser and more frequent.
This is usually temporary and will resolve once you’ve finished the course of antibiotics. They don’t pose a risk to your baby.
Contact your doctor again if your symptoms worsen or haven’t begun to improve within 48 hours of starting antibiotic treatment.
Surgery
Surgery to remove one or more of your milk ducts may be recommended in some cases in non-breastfeeding women that recur frequently or persist despite treatment.
This operation is usually performed with a general anesthetic where you’re asleep, and lasts about 30 minutes. Most people can go home the same day as the procedure or the day after.
If all of the milk ducts in one of your breasts are removed during this operation, you’ll no longer be able to breastfeed using that breast. You may also lose some sensation in the nipple of the treated breast(s).
Make sure you discuss all the risks and implications of surgery with your doctor and surgeon beforehand.